Abstract
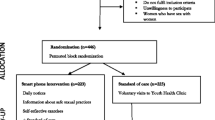
Recall and social desirability bias undermine self-report of paper-and-pencil questionnaires. Mobile phone questionnaires may overcome these challenges. We assessed and compared sexual risk behavior reporting via in-clinic paper-and-pencil and mobile phone questionnaires. HVTN 915 was a prospective cohort study of 50 adult women in Soweto, who completed daily mobile phone, and eight interviewer-administered in-clinic questionnaires over 12 weeks to assess sexual risk. Daily mobile phone response rates were 82% (n = 3486/4500); 45% (n = 1565/3486) reported vaginal sex (median sex acts 2 (IQR: 1–3)) within 24 h and 40% (n = 618/1565) consistent condom. Vaginal sex reporting was significantly higher via mobile phone across all visits (p < 0.0001). There was no significant difference in condom use reporting by mobile phone and in-clinic paper-based questionnaires across all visits (p = 0.5134). The results show high adherence and reporting of sex on the mobile phone questionnaire. We demonstrate feasibility in collecting mobile phone sexual risk data.


Similar content being viewed by others
Notes
This is the sex frequency as indicated at the start of the sentence. At each follow-up visit, the reported sex frequencies dropped by 0.0418.
References
Shisana O, Rehle T, Simbayi LC, et al. South African national HIV prevalence, incidence, behaviour and communication survey 2008: a turning tide among teenagers. Cape Town: HSRC Press; 2009.
Shisana O, Rehle T, Simbayi LC, et al. South African national HIV prevalence, incidence, behaviour and communication survey 2012. Cape Town: HSRC Press; 2014.
Wechsberg WM, Myers B, Kline TL, Careny T, Browne FA, Novak SP. The relationship of alcohol and other drug use typologies to sex risk behaviors among vulnerable women in Cape Town, South Africa. J AIDS Clin Res. 2012;1(15):1–17.
Hedden SL, Whitaker D, Floyd L, Latimer WW. Gender differences in the prevalence and behavioral risk factors of HIV in South African drug users. AIDS Behav. 2009;13(2):288–96.
Needle R, Kroeger K, Belani H, Achrekar A, Parry CD, Dewing S. Sex, drugs, and HIV: rapid assessment of HIV risk behaviors among street-based drug using sex workers in Durban, South Africa. Soc Sci Med. 2008;67(9):1447–55.
Dunkle KL, Beksinska ME, Rees VH, Ballard RC, Htun Y, Wilson ML. Risk factors for HIV infection among sex workers in Johannesburg, South Africa. Int J STD AIDS. 2005;16(3):256–61.
Parry CD, Dewing S, Petersen P, et al. Rapid assessment of HIV risk behavior in drug using sex workers in three cities in South Africa. AIDS Behav. 2009;13(5):849–59.
Kalichman SC, Simbayi LC, Kagee A, et al. Associations of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Soc Sci Med. 2006;62(7):1641–9.
Gray GE, Metch B, Churchyard G, et al. Does participation in an HIV vaccine efficacy trial affect risk behaviour in South Africa? Vaccine. 2013;31(16):2089–96.
Brooks RA, Landovitz MD, Kaplan RL, Lieber E, Lee SJ, Barkley TW. Sexual risk behaviors and acceptability of HIV Pre-exposure Prophylaxis among HIV-negative gay and bisexual men in serodiscordant relationships: a mixed methods study. AIDS Patient Care STDs. 2011;25(2):1–8.
Phillips A, Gomez GB, Boily MC, Garnett GP. A systematic review and meta-analysis of quantitative interviewing tools to investigate self-reported HIV and STI associated behaviours in low- and middle-income countries. Int J Epidemiol. 2010;39:1541–55.
Gray G, Moodie Z, Metch B, et al. Recombinant adenovirus type 5 HIV gag/pol/nef vaccine in South Africa: unblinded, long-term follow-up of the phase 2b HVTN 503/Phambili study. Lancet. 2014;14(5):388–96.
Pettifor A, MacPhail C, Hughes JP, et al. The effect of a conditional cash transfer on HIV incidence in young women in rural South Africa (HPTN 068): a phase 3, randomised controlled trial. Lancet. 2016;4(12):e978–88.
Ritchwood TD, Hughes JP, Jennings L, et al. Characteristics of age-discordant partnerships associated with HIV risk among young South African women (HPTN 068). JAIDS. 2016;72(4):423–9.
Stalgaitis C, Glick SN. The use of web-based diaries in sexual risk behaviour research: a systematic review. Sex Transm Infect. 2014;90(5):374–81.
Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV: issues in methodology, interpretation, and prevention. Am Psychol. 1993;48(10):1035–45.
Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. accuracy of self-reports. Ann Behav Med. 2003;26(2):104–23.
Fenton AK, Johnson AM, McManus S, Erens B. Measuring sexual behaviour: methodological challenges in survey research. BMJ. 2001;77(2):84–92.
Weinhardt L, Forsyth A, Carey M, Jaworski B, Durant L. Reliability and validity of self-report measures of HIV-related sexual behavior: progress since 1990 and recommendations for research and practice. Arch Sex Behav. 1998;27(2):155–80.
Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960;34(4):349–54.
Latkin CA, Vlahov D. Socially desirable response tendency as a correlate of accuracy of self-reported HIV serostatus for HIV seropositive injection drug users. Addiction. 1998;93(8):1191–7.
Loo R, Thorpe K. Confirmatory factor analyses of the full and short versions of the Marlowe–Crowne social desirability scale. J Soc Psychol. 2000;140(5):628–35.
Catania JA, Binson D, Van der Straten A, Stone V. Methodological research on sexual behavior in the AIDS era. J Sex Res. 1995;6:77–125.
Catania JA, Gibson DR, Chitwood DD, Coates T. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull. 1990;108(3):339–62.
Delamater J. Methodological issues in the study of pre-marital sexuality. Sociol Methods Res. 1974;3:30–61.
James NJ, Bignell CJ, Gillies PA. The reliability of self reported sexual behaviour. AIDS. 1991;5:333–6.
Anderson B, Broffitt B. Is there a reliable and valid self-report measure of sexual behaviour. Arch Sex Behav. 1988;17:509–25.
Blake SM, Sharp SS, Temoshok L, et al. Methodological considerations in developing measures of HIV risk-relevant behaviors and attitudes; an empirical illustration. Psychol Health. 1992;6:265–80.
Kauth MR, St Lawrence JS, Kelly JA. Reliability of retrospective assessments of sexual HIV risk behavior: a comparison of biweekly, three-month and twelve month self-reports. AIDS Educ Prev. 1991;3:207–14.
Shiffman S, Stone AA, Huffors MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32.
Militello LK, Kelly SA, Melnyk BM. Systematic review of text-messaging interventions to promote healthy behaviors in pediatric and adolescent populations: implications for clinical practice and research. Worldviews Evid Based Nurs. 2012;9(2):66–77.
Ybarra ML, Bull SS. Current trends in internet and cell phone–based HIV prevention and intervention programs. Curr HIV/AIDS Rep. 2007;4(4):201–7.
Broaddus MR, Dickson-Gomez J. Text messaging for sexual communication and safety among African American young adults. Qual Health Res. 2013;23(10):1344–53.
Horvath KJ, Danilenko GP, Williams ML, et al. Technology use and reasons to participate in social networking health websites among people living with HIV in the US. AIDS Behav. 2012;16(4):900–10.
Gold J, Lim MS, Hocking JS, Keogh LA, Spelman T, Hellard ME. Determining the impact of text messaging for sexual health promotion to young people. Sex Transm Dis. 2011;38(4):247–52.
Lim MS, Hocking JS, Aitken CK, et al. Impact of text and email messaging on the sexual health of young people: a randomised controlled trial. J Epidemiol Community Health. 2012;66(1):69–74.
Levine D, McCright J, Dobkin L, Woodruff AJ, Klausner JD. SEXINFO: a sexual health text messaging service for San Francisco youth. Am J Public Health. 2008;98(3):393–5.
Suffoletto B, Akers A, McGinnis KA, Calabria J, Wiesenfeld HC, Clark DB. A sex risk reduction text-message program for young adult females discharged from the emergency department. J Adolesc Health. 2013;53(3):387–93.
Mitchell JW, Torres MB, Joe J, Danh T, Gass B, Horvath KJ. Formative work to develop a tailored HIV testing smartphone app for diverse, at-risk, HIV-negative men who have sex with men: a focus group study. JMIR mHealth uHealth. 2016;4(4):e128.
Horvath KJ, Alemu D, Danh T, Baker JV, Carrico AW. Creating effective mobile phone apps to optimize antiretroviral therapy adherence: perspectives from stimulant-using HIV-positive men who have sex with men. JMIR mHealth uHealth. 2016;4(2):e48.
Puccio JA, Belzer M, Olson J, et al. The use of cell phone reminder calls for assisting HIV-infected adolescents and young adults to adhere to highly active antiretroviral therapy: a pilot study. AIDS Patient Care STDS. 2006;20(6):438–44.
Andrasik MP, Karuna ST, Nebergall M, Koblin BA. Kublin JG, and NIAID HIV Vaccine Trials Network. Behavioral risk assessment in HIV Vaccine Trials Network (HVTN) clinical trials: a qualitative study exploring HVTN staff perspectives. Vaccine. 2013;31(40):4398–405.
Statistics South Africa. General household survey 2013. Pretoria: Statistics South Africa; 2012.
Effective Measure. South African mobile report: a survey of desktop user’s attitudes and uses of mobile phones February 2016. https://cdn2.hubspot.net/hubfs/2622125/Content/Blogs/South-Africa-Mobile-Report-Feb-2016.pdf?__hssc=40513789.4.1519806204883&__hstc=40513789.4cdbb6f1b23fc01bb6f998b188ef5345.1519806204882.1519806204882.1519806204882.1&__hsfp=3596955054&hsCtaTracking=fbb82af1-25ee-4cd4-b7e2-b9c39d870a96%7C52a197c6-f951-4210-a660-20806c1d18d2. Accessed 28 Feb 2018.
Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Glob Health. 2006;2:9.
Mukund Bahadur KC, Murray PJ. Cell phone short messaging service (SMS) for HIV/AIDS in South Africa: a literature review. Stud Health Technol Inform. 2010;160(1):530–4.
Deglise C, Suggs S, Odermatt P. Short message service (SMS) applications for disease prevention in developing countries. JMIR. 2012;14(1):e3.
Lester RT, Gelmon L, Plummer FA. Cell phones: tightening the communication gap in resource-limited antiretroviral programmes? AIDS. 2006;20(17):2242–4.
Dietrich J. A prospective cohort study evaluating the use of self-administered vaginal swabs to detect HIV-1 virions among 18 to 25 year-old women in South Africa. Innovative Uses of Technology in HIV Clinical Trials. Newark, United States, 2016 [oral presentation].
Lemos M, Morgan C, Lazarus E, et al. High adherence to daily vaginal swabs and reliable sexual behavior reporting via mobile phone aa for assessing HIV virion exposure (HVTN 915). HIVR4P. Chicago, USA, 2016 [poster presentation].
Nkala B, Khunwane M, Dietrich J, et al. Kganya Motsha Adolescent Centre: a model for adolescent friendly HIV management and reproductive health for adolescents in Soweto, South Africa. AIDS Care. 2015;27(6):697–702.
Dietrich JJ, Coetzee J, Otwombe K, et al. Adolescent-friendly technologies as potential adjuncts for health promotion. Health Educ. 2014;114(4):304–18.
Dietrich J, Laher F, Hornschuh S, et al. Access, use and potential for social networking as a health promotion tool among adolescents in Soweto, South Africa. JMIR Public Health Surveill. 2016;2(2):e154.
South African Tourism. South Africa’s township taverns-Shebeens. Available at: http://www.southafrica.net/za/en/articles/entry/article-southafrica.net-shebeens. Accessed 22 Dec 2016.
Ramjee G, Weber AE, Morar NS. Recording sexual behavior: comparison of recall questionnaires with a coital diary. Sex Transm Dis. 1999;26(7):374–80.
SurveyCTO. SurveyCTO [homepage on the internet]. http://www.surveycto.com/index.html. Accessed 8 Dec 2016.
Vodacom. Data bundles explained. http://now.vodacom.co.za/article/2013/07/18/what-is-a-data-bundle. Accessed 25 May 2017.
Egleston BL, Miller SM, Meropol NJ. The impact of misclassification due to survey response fatigue on estimation and identifiability of treatment effects. Stat Med. 2011;30(30):3560–72.
Curran K, Mugo NR, Kurth A, et al. Daily short message service surveys to measure sexual behavior and pre-exposure prophylaxis use among Kenyan men and women. AIDS Behav. 2013;17(9):2977–85.
Baseman JG, Revere D, Painter I, Toyoji M, Thiede H, Duchin J. Public health communications and alert fatigue. BMC Health Serv Res. 2013;13(295):1–8.
Anhoj J, Moldrup C. Feasibility of collecting diary data from asthma patients through mobile phones and SMS (Short Message Service): response rate analysis and focus group evaluation from a pilot study. JMIR. 2004;6(4):e42.
Sartor CE, O’Malley SS. Brief Report: a web-based pilot study of childhood sexual abuse, recent stressful events, and alcohol use in women. Am J Addict. 2016;25(3):184–7.
Lim MS, Sacks-Davis R, Aitken CK, Hocking JS, Hellard ME. Randomised controlled trial of paper, online and SMS diaries for collecting sexual behaviour information from young people. J Epidemiol Community Health. 2010;64(10):885–9.
Wray TB, Kahler CW, Monti PM. Using ecological momentary assessment (EMA) to study sex events among very high-risk men who have sex with men (MSM). AIDS Behav. 2016;20(10):2231–42.
Yang C, Linas B, Kirk G, et al. Feasibility and acceptability of smartphone-based ecological momentary assessment of alcohol use among African American men who have sex with men in Baltimore. JMIR mHealth uHealth. 2015;3(2):e67.
Rowe C, Hern J, DeMartini A, et al. Concordance of text message ecological momentary assessment and retrospective survey data among substance-using men who have sex with men: a secondary analysis of a randomized controlled trial. JMIR mHealth uHealth. 2016;4(2):e44.
Christie A, Dagfinrud H, Dale O, Schulz T, Hagen KB. Collection of patient-reported outcomes; - text messages on mobile phones provide valid scores and high response rates. BMC Med Res Methodol. 2014;2014(14):52.
Funding
The authors wish to thank the trial participants, the HVTN core, the Soweto Clinical Research Site study team, and iKapadata. The HVTN 915 study was funded by the National Institute of Allergy and Infectious Diseases (NIAID) U.S. Public Health Service Grants UM1 AI068614 [LOC: HIV Vaccine Trials Network], UM1 AI068635 [SDMC: HIV Vaccine Trials Network], UM1 AI068618 [HVTN Laboratory Center] and UM1 AI069453 [Soweto-Bara Clinical Research Site]. Dr. Janan Dietrich received a Thuthuka post Ph.D. funding award (2014–2016) from the South African National Research Foundation (NRF). Any opinion, findings, conclusion or recommendation expressed in this material is solely the responsibility of the authors, and does not necessarily represent the official views of the NIAID, National Institutes of Health (NIH), or SA NRF. Any opinion, finding, conclusion or recommendation expressed in this material is that of the authors and the SA NRF does not accept any liability in this regard.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All authors have declared that they have no conflict of interest.
Ethical Approval
This study involved human participants. All procedures performed in this study were in accordance with the ethical standards of the HVTN, the University of the Witwatersrand and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Dietrich, J.J., Lazarus, E., Andrasik, M. et al. Mobile Phone Questionnaires for Sexual Risk Data Collection Among Young Women in Soweto, South Africa. AIDS Behav 22, 2312–2321 (2018). https://doi.org/10.1007/s10461-018-2080-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2080-y