Abstract
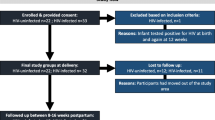
HIV-exposed infants born to depressed women may be at risk for adverse developmental outcomes. Half of HIV-infected women in rural South Africa (SA) may suffer from pregnancy-related depression. This pilot study examined the impact of depression in HIV-infected women in rural SA on infant development. Mother-infant dyads (N = 69) were recruited in rural SA. Demographics, HIV disclosure, depression, male involvement, and alcohol use at baseline (18.35 ± 5.47 weeks gestation) were assessed. Male involvement, depression, infant HIV serostatus and development were assessed 12 months postnatally. Half of the women (age = 29 ± 5) reported depression prenatally and one-third reported depression postnatally. In multivariable logistic regression, not cohabiting with their male partner, nondisclosure of HIV status, and postnatal depression predicted cognitive delay; decreased prenatal male involvement predicted delayed gross motor development (ps < 0.05). Assessing pregnancy-related depression among HIV-infected women and infant development and increasing male involvement may reduce negative developmental outcomes among HIV-exposed or infected infants.
Resumen
Los bebés expuestos al VIH, provenientes de mujeres deprimidas, pueden estar a riesgo de resultados adversos en el desarrollo. La mitad de las mujeres infectadas con VIH, en Sudáfrica (SA) rural, pueden sufrir de depresión relacionada con el embarazo. Este estudio piloto examinó el impacto de la depresión en el desarrollo infantil entre mujeres infectadas con VIH en SA rural. Parejas (N = 69) de madre e infante fueron reclutadas en SA rural. Se evaluaron datos demográficos, revelación de estatus de VIH a su pareja masculina, depresión, participación masculina en el embarazo y consumo de alcohol al inicio del estudio (18,35 ± 5,47 semanas de gestación). La participación masculina, depresión, el estatus serológico de VIH y el desarrollo infantil se evaluaron 12 meses postnatalmente. La mitad de las mujeres (edad = 29 ± 5) presentaron depresión prenatal y un tercio depresión postparto. En regresión logística multivariable, no vivir con su pareja, no revelar su estatus de VIH, y depresión postnatal predijeron retraso cognitivo; la disminución de participación masculina durante el embarazo predijo el desarrollo motor grueso retardado (p < 0,05). Evaluar la depresión relacionada con el embarazo entre mujeres infectadas con VIH y el desarrollo infantil; así, como aumentar la participación de las parejas masculinas pudieran reducir los resultados adversos en el desarrollo de niños expuestos a, o infectados por, el VIH.
Similar content being viewed by others
References
Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N, et al. The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Gen Hosp Psychiatry. 2009;31(5):403–13.
Roehr B. American Psychiatric Association explains DSM-5. BMJ. 2013;346:f3591.
Natamba B, Achan J, Arbach A, Oyok T, Ghosh S, Mehta S, et al. Reliability and validity of the center for epidemiologic studies-depression scale in screening for depression among HIV-infected and-uninfected pregnant women attending antenatal services in northern Uganda: a cross-sectional study. BMC psychiatry. 2014;14(1):1.
Stringer EM, Meltzer-Brody S, Kasaro M, Stuebe AM, Wiegand S, Paul R, et al. Depression, pregnancy, and HIV: the case to strengthen mental health services for pregnant and post-partum women in sub-Saharan Africa. Lancet Psychiatry. 2014;1(2):159–62.
Dow A, Dube Q, Pence BW, Van Rie A. Postpartum depression and HIV infection among women in Malawi. Jaids-J Acq Imm Def. 2014;65(3):359–65.
Sawyer A, Ayers S, Smith H. Pre- and postnatal psychological wellbeing in Africa: a systematic review. J Affect Disorders. 2010;123(1–3):17–29.
Peltzer K, Rodriguez VJ, Jones D. Prevalence of prenatal depression and associated factors among HIV-positive women in primary care in Mpumalanga province, South Africa. Sahara J-J Soc Asp H. 2016;13(1):60–7.
O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psycho. 2013;9:379–407.
Ammassari A, Antinori A, Aloisi MS, Trotta MP, Murri R, Bartoli L, et al. Depressive symptoms, neurocognitive impairment, and adherence to highly active antiretroviral therapy among HIV-infected persons. Psychosomatics. 2004;45(5):394–402.
French AL, Gawel SH, Hershow R, Benning L, Hessol NA, Levine AM, et al. Trends in mortality and causes of death among women with HIV in the US: a ten-year study. J Acquir Immune Defic Syndr. 2009;51(4):399–406.
Ickovics JR, Reed E, Magriples U, Westdahl C, Schindler Rising S, Kershaw TS. Effects of group prenatal care on psychosocial risk in pregnancy: results from a randomised controlled trial. Psychol Health. 2011;26(2):235–50.
Kapetanovic S, Christensen S, Karim R, Lin F, Mack WJ, Operskalski E, et al. Correlates of perinatal depression in HIV-infected women. AIDS Patient Care STDS. 2009;23(2):101–8.
Nachega JB, Mutamba B, Basangwa D, Nguyen H, Dowdy DW, Mills EJ, et al. Severe mental illness at ART initiation is associated with worse retention in care among HIV-infected Ugandan adults. Trop Med Int Health. 2013;18(1):53–7.
Turner BJ, Hecht FM. Improving on a coin toss to predict patient adherence to medications. Ann Intern Med. 2001;134(10):1004–6.
Levine AB, Aaron EZ, Criniti SM. Screening for depression in pregnant women with HIV infection. J Reprod Med. 2008;53(5):352–6.
Blaney NT, Fernandez MI, Ethier KA, Wilson TE, Walter E, Koenig LJ, et al. Psychosocial and behavioral correlates of depression among HIV-infected pregnant women. Aids Patient Care St. 2004;18(7):405–15.
Bonacquisti A, Geller PA, Aaron E. Rates and predictors of prenatal depression in women living with and without HIV. Aids Care. 2014;26(1):100–6.
Casale M, Wild L, Cluver L, Kuo C. Social support as a protective factor for depression among women caring for children in HIV-endemic South Africa. J Behav Med. 2015;38(1):17–27.
Davies T, Schneider M, Nyatsanza M, Lund C. “The sun has set even though it is morning”: experiences and explanations of perinatal depression in an urban township, Cape Town. Transcult Psychiatry. 2016;53(3):286–312.
Van den Bergh BR, Mulder EJ, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms, A review. Neurosci Biobehav Rev. 2005;29(2):237–58.
Kingston D, McDonald S, Austin MP, Tough S. Association between prenatal and postnatal psychological distress and toddler cognitive development: a systematic review. PLoS ONE. 2015;. doi:10.1371/journal.pone.0126929.
Murray L, Fiori-Cowley A, Hooper R, Cooper P. The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev. 1996;67(5):2512–26.
Murray L, Kempton C, Woolgar M, Hooper R. Depressed mothers speech to their infants and its relation to infant gender and cognitive-development. J Child Psychol Psyc. 1993;34(7):1083–101.
Field T. Prenatal depression effects on early development: a review. Infant Behav Dev. 2011;34(1):1–14.
Sinclair D, Murray L. Effects of postnatal depression on children’s adjustment to school—teacher’s reports. Brit J Psychiat. 1998;172:58–63.
O’Hara MW. Postpartum depression: what we know. J Clin Psychol. 2009;65(12):1258–69.
Goodman S, Brand S, Hammen C. Maternal depression and infant mental health. Handbook of depression and its treatment. 2nd ed. New York: Guilford; 2008. p. 249–76.
Dobrova-Krol NA, van IJzendoorn MH, Bakermans-Kranenburg MJ, Juffer F. Effects of perinatal HIV infection and early institutional rearing on physical and cognitive development of children in Ukraine. Child Dev. 2010;81(1):237–51.
Le Doare K, Bland R, Newell ML. Neurodevelopment in children born to HIV-infected mothers by infection and treatment status. Pediatrics. 2012;130(5):E1326–44.
Whitehead N, Potterton J, Coovadia A. The neurodevelopment of HIV-infected infants on HAART compared to HIV-exposed but uninfected infants. Aids Care. 2014;26(4):497–504.
O’Connor TG, Heron J, Glover V, Team AS. Antenatal anxiety predicts child behavioral/emotional problems independently of postnatal depression. J Am Acad Child Psy. 2002;41(12):1470–7.
Buss C, Davis EP, Hobel CJ, Sandman CA. Maternal pregnancy-specific anxiety is associated with child executive function at 6–9 years age. Stress. 2011;14(6):665–76.
van den Berg S, Shapiro DA, Bickerstaffe D, Cavanagh K. Computerized cognitive-behaviour therapy for anxiety and depression: a practical solution to the shortage of trained therapists. J Psychiatr Ment Health Nurs. 2004;11(5):508–13.
Mellins CA, Kang E, Leu CS, Havens JF, Chesney MA. Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS Patient Care STDS. 2003;17(8):407–16.
Talge NM, Neal C, Glover V, Early Stress TR, Prevention Science Network F Neonatal Experience on C, et al. Antenatal maternal stress and long-term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry. 2007;48(3–4):245–61.
Emerson E, Einfeld S. Emotional and behavioural difficulties in young children with and without developmental delay: a bi-national perspective. J Child Psychol Psychiatry. 2010;51(5):583–93.
Feldman M, Hancock C, Rielly N, Minnes P, Cairns C. Behavior problems in young children with or at risk for developmental delay. J Child Fam Stud. 2000;9(2):247–61.
Sheeber L, Davis B, Hops H. Gender-specific vulnerability to depression in children of depressed mothers. Children of depressed parents: Mechanisms of risk and implications for treatment. 2002:253–74.
Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1–27.
Hauser-Cram P, Woodman AC. Trajectories of internalizing and externalizing behavior problems in children with developmental disabilities. J Abnorm Child Psychol. 2016;44(4):811–21.
Lowe K, Allen D, Jones E, Brophy S, Moore K, James W. Challenging behaviours: prevalence and topographies. J Intellect Disabil Res. 2007;51(Pt 8):625–36.
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–19.
Hartley C, Pretorius K, Mohamed A, Laughton B, Madhi S, Cotton MF, et al. Maternal postpartum depression and infant social withdrawal among human immunodeficiency virus (HIV) positive mother-infant dyads. Psychol Health Med. 2010;15(3):278–87.
Avan B, Richter LM, Ramchandani PG, Norris SA, Stein A. Maternal postnatal depression and children’s growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Arch Dis Child. 2010;95(9):690–5.
Tomlinson M, Cooper P, Murray L. The mother-infant relationship and infant attachment in a south African peri-urban settlement. Child Dev. 2005;76(5):1044–54.
Hadley C, Tegegn A, Tessema F, Asefa M, Galea S. Parental symptoms of common mental disorders and children’s social, motor, and language development in sub-Saharan Africa. Ann Hum Biol. 2008;35(3):259–75.
Jones D, Peltzer K, Weiss SM, Sifunda S, Dwane N, Ramlagan S, et al. Implementing comprehensive prevention of mother-to-child transmission and HIV prevention for South African couples: study protocol for a randomized controlled trial. Trials. 2014;15:417.
Kershaw TS, Magriples U, Westdahl C, Rising SS, Ickovics J. Pregnancy as a window of opportunity for HIV prevention: effects of an HIV intervention delivered within prenatal care. Am J Public Health. 2009;99(11):2079–86.
Metzger DS, Koblin B, Turner C, Navaline H, Valenti F, Holte S, et al. Randomized controlled trial of audio computer-assisted self-interviewing: utility and acceptability in longitudinal studies. HIVNET Vaccine Preparedness Study Protocol Team. Am J Epidemiol. 2000;152(2):99–106.
Bayley N, Reuner G. Bayley scales of infant and toddler development: Bayley-III: Harcourt Assessment. Tex: Psych. Corporation San Antonio; 2006.
Rademeyer V, Jacklin L. A study to evaluate the performance of black South African urban infants on the Bayley Scales of Infant Development III. S. Afr. J Child Health. 2013;7(2):54–9.
Ferguson G, Jelsma J. The prevalence of motor delay among HIV infected children living in Cape Town, South Africa. Int J Rehabil Res. 2009;32(2):108–14.
Marlow N. Measuring neurodevelopmental outcome in neonatal trials: a continuing and increasing challenge. Arch Dis Child Fetal Neonatal Ed. 2013;98:F554–8.
Hutchings J, Potterton J. Developmental delay in HIV-exposed infants in Harare, Zimbabwe. Vulnerable Children Youth Stud. 2014;9(1):43–55.
Van Rie A, Mupuala A, Dow A. Impact of the HIV/AIDS epidemic on the neurodevelopment of preschool-aged children in Kinshasa, Democratic Republic of the Congo. Pediatrics. 2008;122(1):e123–8.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression—development of the 10-Item Edinburgh postnatal depression scale. Brit J Psychiat. 1987;150:782–6.
Lawrie TA, Hofmeyr GJ, de Jager M, Berk M. Validation of the Edinburgh postnatal depression scale on a cohort of South African women. S Afr Med J. 1998;88(10):1340–4.
Byamugisha R, Tumwine JK, Semiyaga N, Tylleskar T. Determinants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: a cross-sectional survey. Reprod Health. 2010;7.
Koutra K, Chatzi L, Bagkeris M, Vassilaki M, Bitsios P, Kogevinas M. Antenatal and postnatal maternal mental health as determinants of infant neurodevelopment at 18 months of age in a mother-child cohort (Rhea Study) in Crete, Greece. Soc Psych Psych Epid. 2013;48(8):1335–45.
Barker ED, Jaffee SR, Uher R, Maughan B. The Contribution of prenatal and postnatal maternal anxiety and depression to child mal adjustment. Depress Anxiety. 2011;28(8):696–702.
Korhonen M, Luoma I, Salmelin R, Tamminen T. A longitudinal study of maternal prenatal, postnatal and concurrent depressive symptoms and adolescent well-being. J Affect Disorders. 2012;136(3):680–92.
Peltzer, K., Mlambo, M., Matseke, M. G., Shikwane, E., Louw, J., & Kekana, Q. (2011). Report on PMTCT comprehensive community intervention package including male involvement, infant follow-up, peer support, partner violence and infant feeding in Nkangala District, Mpumalanga province.
Olley BO, Seedat S, Nei DG, Stein DJ. Predictors of major depression in recently diagnosed patients with HIV/AIDS in South Africa. AIDS Patient Care STDS. 2004;18(8):481–7.
Sarkadi A, Kristiansson R, Oberklaid F, Bremberg S. Fathers’ involvement and children’s developmental outcomes: a systematic review of longitudinal studies. Acta Paediatr. 2008;97(2):153–8.
Rhodes KV, Lauderdale DS, He T, Howes DS, Levinson W. “Between me and the computer”: increased detection of intimate partner violence using a computer questionnaire. Ann Emerg Med. 2002;40(5):476–84.
Lewis AJ, Austin E, Knapp R, Vaiano T, Galbally M. Perinatal maternal mental health, fetal programming and child development. Healthcare (Basel). 2015;3(4):1212–27.
Aluisio AR, Bosire R, Bourke B, Gatuguta A, Kiarie JN, Nduati R, et al. Male partner participation in antenatal clinic services is associated with improved HIV-free survival among infants in Nairobi, Kenya: a Prospective Cohort Study. Jaids-J Acq Imm Def. 2016;73(2):169–76.
Crozier SR, Robinson SM, Borland SE, Godfrey KM, Cooper C, Inskip HM, et al. Do women change their health behaviours in pregnancy? Findings from the Southampton Women’s Survey. Paediatr Perinat Epidemiol. 2009;23(5):446–53.
Acknowledgements
This study was funded by a collaborative NIH/PEPFAR grant, R01HD078187-S. Activities were conducted with the support of the University of Miami Miller School of Medicine Center for AIDS Research, funded by an NIH grant, P30AI073961.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rodriguez, V.J., Matseke, G., Cook, R. et al. Infant Development and Pre- and Post-partum Depression in Rural South African HIV-Infected Women. AIDS Behav 22, 1766–1774 (2018). https://doi.org/10.1007/s10461-017-1925-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1925-0