Abstract
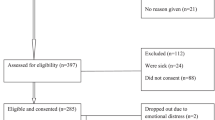
HIV-positive pregnant and postpartum women’s status disclosure to male sexual partners is associated with improved HIV and maternal and child health outcomes. Yet, status disclosure remains a challenge for many women living with HIV in sub-Saharan Africa, particularly those who are fearful of violence. The objective of the present study is to advance the current understanding of the relationship between intimate partner violence against women and their HIV status disclosure behaviors. We specifically evaluate how the severity, frequency, and type of violence against postpartum HIV-positive women affect status disclosure within married/cohabiting couples. A cross-sectional survey was administered by trained local research assistants to 320 HIV-positive postpartum women attending a large public health center for pediatric immunizations in Lusaka, Zambia. Survey data captured women’s self-reports of various forms of intimate partner violence and whether they disclosed their HIV status to the current male partner. Multiple logistic regression models determined the odds of status disclosure by the severity, frequency, and type of violence women experienced. Our findings indicate a negative dose–response relationship between the severity and frequency of intimate partner violence and status disclosure to male partners. Physical violence has a more pronounced affect on status disclosure than sexual or emotional violence. Safe options for women living with HIV who experience intimate partner violence, particularly severe and frequent physical violence, are urgently needed. This includes HIV counselors’ ability to evaluate the pros and cons of status disclosure among women and support some women’s decisions not to disclose.


Similar content being viewed by others
References
Maman S. HIV status disclosure to families for social support in South Africa (NIMH project accept/HPTN 043). AIDS Care. 2014;26(2):226–32.
Matthews C, et al. Disclosure of HIV status and its consequences. S Afr Med J. 1999;89:1238.
Peltzer K, et al. Promoting male involvement to improve PMTCT uptake and reduce antenatal HIV infection: a cluster randomized controlled trial protocol. BMC Public Health. 2011;11:778.
Hampanda KM. Intimate partner violence and HIV-positive women’s non-adherence to antiretroviral medication for the purpose of prevention of mother-to-child transmission in Lusaka, Zambia. Soc Sci Med. 2016;153:123–30.
Stirratt MJ, et al. The role of HIV serostatus disclosure in antiretroviral medication adherence. AIDS Behav. 2006;10(5):483–93.
Medley A, et al. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. 2004;82(4):299–307.
Etiebet MA, et al. Integrating prevention of mother-to-child HIV transmission into antenatal care: learning from the experiences of women in South Africa. AIDS Care. 2004;16(1):37–46.
Msellati P. Improving mothers’ access to PMTCT programs in West Africa: a public health perspective. Soc Sci Med. 2009;69(6):807–12.
Mucheto P, et al. Determinants of nondisclosure of HIV status among women attending the prevention of mother to child transmission programme, Makonde district, Zimbabwe, 2009. Pan Afr Med J. 2011;8:51.
Tam M, Amzel A, Phelps BR. Disclosure of HIV serostatus among pregnant and postpartum women in sub-Saharan Africa: a systematic review. AIDS Care. 2015;27(4):436–50.
CSO, Zambia Demographic and Health Survey 2013-14. Central Statistical Office, Ministry of Health, and ICF International: Rockville, Maryland, USA; 2014.
Hampanda K. Intimate partner violence and HIV-positive women’s non-adherence to antiretroviral medication for the purpose of prevention of mother-to-child transmission in Lusaka, Zambia. Soc Sci Med. 2016;153:123–30.
Hampanda K. Intimate partner violence against HIV-positive women is associated with sub-optimal infant feeding practices in Lusaka, Zambia. Matern Child Health J. 2016;20(12):2599–606.
Hampanda KM, Nimz AM, Abuogi LL. Barriers to uptake of early infant HIV testing in Zambia: the role of intimate partner violence and HIV status disclosure within couples. AIDS Res Ther. 2017;14(1):17.
Chen HN, Cohen P, Chen S. How big is a big odds ratio? interpreting the magnitudes of odds ratios in epidemiological studies. Commun Stat-Simul Comput. 2010;39(4):860–4.
Faul F, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91.
Simoni JM, et al. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10(3):227–45.
National Statistical Office and ICF Macro, Malawi Demographic and Health Survey 2010. 2011, NSO and ICF Macro: Zomba, Malawi, and Calverton, Maryland, USA.
World Health Organization (WHO). Putting women first: ethical and safety recommendations for research on domestic violence against women. Department of Gender and Women’s Health Family and Community Health. 2012. http://www.who.int/gender/violence/womenfirtseng.pdf.
Straus MA, et al. The revised conflict tactics scales (CTS2)—development and preliminary psychometric data. J Fam Issues. 1996;17(3):283–316.
CSO, Zambia Demographic and Health Survey 2007. Central Statistical Office (CSO), Ministry of Health (MOH), Tropical diseases research centre (TDRC), University of Zambia, & Macro International Inc.: Calverton, Maryland, USA; 2009.
MacQuarrie KL, Winter R, Kishor S. Spousal violence in Sub-Saharan Africa: structure, forms, and levels, in population association of America. Annual Meeting. Boston, MA; 2014.
Filmer D, Pritchett L. Estimating wealth effect without expenditure data or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32.
Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger, P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27(1):85–95.
StataCorp. Stata statistical software: release 11. College Station, TX: StataCorp LP; 2009.
Shamu S, et al. Intimate partner violence after disclosure of HIV test results among pregnant women in Harare, Zimbabwe. PLoS ONE. 2014;9(10):e109447.
Kiula ES, Damian DJ, Msuya SE. Predictors of HIV serostatus disclosure to partners among HIV-positive pregnant women in Morogoro, Tanzania. BMC Public Health. 2013;13:433.
Antelman G, et al. Predictors of HIV-1 serostatus disclosure: a prospective study among HIV-infected pregnant women in Dar es Salaam, Tanzania. AIDS. 2001;15(14):1865–74.
Walcott MM, et al. Facilitating HIV status disclosure for pregnant women and partners in rural Kenya: a qualitative study. BMC Public Health. 2013;13:1115.
Osoti AO, et al. Home visits during pregnancy enhance male partner HIV counselling and testing in Kenya: a randomized clinical trial. AIDS. 2014;28(1):95–103.
Hatcher AM, et al. Bidirectional links between HIV and intimate partner violence in pregnancy: implications for prevention of mother-to-child transmission. J Int AIDS Soc. 2014;17:19233.
Maman S, et al. Diagnosis and disclosure of HIV status: implications for women’s risk of physical partner violence in the postpartum period. J Acquir Immune Defic Syndr. 2016;72(5):546–51.
Kennedy CE, et al. Safer disclosure of HIV serostatus for women living with HIV who experience or fear violence: a systematic review. J Int AIDS Soc. 2015;18(6 Suppl 5):20292.
Wagman JA, et al. Effectiveness of an integrated intimate partner violence and HIV prevention intervention in Rakai, Uganda: analysis of an intervention in an existing cluster randomised cohort. Lancet Glob Health. 2015;3(1):e23–33.
Maman S, et al. Efficacy of enhanced HIV counseling for risk reduction during pregnancy and in the postpartum period: a randomized controlled trial. PLoS ONE. 2014;9(5):e97092.
Jasseron C, et al. Non-disclosure of a pregnant woman’s HIV status to her partner is associated with non-optimal prevention of mother-to-child transmission. AIDS Behav. 2013;17(2):488–97.
Acknowledgements
The authors would like to thank Dr. Yusuf Ahmed, Christine Chewe Sakala, Grace Lungeani Phiri, Franklin Munsanje, and Bibi Lambert Manda for their contribution to the study. Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health (Award Number F31MH107348) and the University of Colorado Center for Global Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was funded by the National Institute of Mental Health of the National Institutes of Health (Award Number F31MH107348) and the University of Colorado Center for Global Health. Dr. Hampanda declares that she has no conflict of interest. Dr. Rael declares that she has no conflict of interest. All procedures performed involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. The study was approved by the Colorado Multiple Institutional Review Board (COMIRB) and the Excellence in Research Ethics and Science (ERES) Converge Zambia. Informed written consent (or a thumbprint) was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no conflicting interests.
Rights and permissions
About this article
Cite this article
Hampanda, K.M., Rael, C.T. HIV Status Disclosure Among Postpartum Women in Zambia with Varied Intimate Partner Violence Experiences. AIDS Behav 22, 1652–1661 (2018). https://doi.org/10.1007/s10461-017-1909-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1909-0