Abstract
Among persons living with HIV/AIDS (PLHIV), approximately two-thirds report moderate to severe pain. Chronic pain can negatively affect PLHIVs’ health behaviors and outcomes by interfering with their reciprocity (mutual exchange) of support in their caregiving relationships, which has been found to be associated with PLHIVs’ antiretroviral adherence and viral suppression. Data were longitudinal (baseline, 6- and 12-month follow-up) from 383 PLHIV who were formerly or currently using drugs. Utilizing a longitudinal lagged fixed effects structural equation model, we found that never having pain in the past 6 months was predictive of increased reciprocity of support. Sub-analyses by care relationship type revealed never having pain was a significant predictor of greater reciprocity for sexual partner caregiving dyads, but not for kin or friend caregiving dyads. Our study emphasizes the importance of pain management in quality caregiving relationships characterized by reciprocity, which has consistently been found to be associated with stronger, more supportive caregiving relationships and better quality of life. Our findings suggest the importance of pain management intervention for improving reciprocity between vulnerable PLHIVs and their primary caregivers, especially between PLHIVs and caregivers who are current or former sexual partners.


Similar content being viewed by others
References
Merlin JS, Cen L, Praestgaard A, et al. Pain and physical and psychological symptoms in ambulatory HIV patients in the current treatment era. J Pain Symptom Manage. 2012;43(3):638–45.
Merlin JS, Westfall AO, Raper JL, et al. Pain, mood, and substance abuse in HIV: implications for clinic visit utilization, antiretroviral therapy adherence, and virologic failure. J Acquir Immune Defic Syndr. 2012;61(2):164–70.
Merlin JS, Zinski A, Norton WE, et al. A conceptual framework for understanding chronic pain in patients with HIV. Pain Pract. 2014;14(3):207–16.
Miaskowski C, Penko JM, Guzman D, Mattson JE, Bangsberg DR, Kushel MB. Occurrence and characteristics of chronic pain in a community-based cohort of indigent adults living with HIV infection. J Pain. 2011;12(9):1004–16.
Merlin JS, Childers J, Arnold RM. Chronic pain in the outpatient palliative care clinic. Am J Hosp Palliat Care. 2013;30(2):197–203.
Knowlton AR, Hua W, Latkin C. Social support networks and medical service use among HIV-positive injection drug users: implications to intervention. AIDS Care. 2005;17(4):479–92.
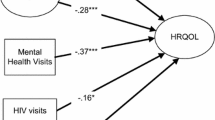
Mitchell MM, Robinson AC, Nguyen TQ, Knowlton AR. Informal caregiver characteristics associated with viral load suppression among current or former drug users living with HIV/AIDS. AIDS Behav. 2015;19(11):2117–22.
Lucas GM, Griswold M, Gebo KA, Keruly J, Chaisson RE, Moore RD. Illicit drug use and HIV-1 disease progression: a longitudinal study in the era of highly active antiretroviral therapy. Am J Epidemiol. 2006;163(5):412–20.
Lemly DC, Shepherd BE, Hulgan T, et al. Race and sex differences in antiretroviral therapy use and mortality among HIV-infected persons in care. J Infect Dis. 2009;199(7):991–8.
Losina E, Schackman BR, Sadownik SN, et al. Racial and sex disparities in life expectancy losses among HIV-infected persons in the united states: impact of risk behavior, late initiation, and early discontinuation of antiretroviral therapy. Clin Infect Dis. 2009;49(10):1570–8.
Chandola T, Marmot M, Siegrist J. Failed reciprocity in close social relationships and health: findings from the Whitehall II study. J Psychosom Res. 2007;63(4):403–11.
Horwitz AV. Siblings as caregivers for the seriously mentally ill. Milbank Q. 1993;71(2):323–39.
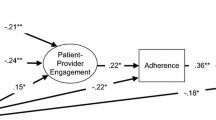
Knowlton AR, Yang C, Bohnert A, Wissow L, Chander G, Arnsten JA. Informal care and reciprocity of support are associated with HAART adherence among men in Baltimore, MD, USA. AIDS Behav. 2011;15(7):1429–36.
Knowlton AR, Arnsten JH, Gourevitch MN, et al. Microsocial environmental influences on highly active antiretroviral therapy outcomes among active injection drug users: the role of informal caregiving and household factors. J Acquir Immune Defic Syndr. 2007;46(Suppl 2):S110–9.
Mitchell MM, Robinson AC, Wolff J, Knowlton AR. Perceived mental health status of injection drug users living with HIV/AIDS: concordance between informal HIV caregivers and care recipient self-reports and associations with caregiving burden and reciprocity. AIDS Behav. 2014;18(6):1103–13.
Knowlton AR, Mitchell MM, Robinson AC, Nguyen TQ, Isenberg S, Denison J. Informal HIV caregiver proxy reports of care recipients’ treatment adherence: relationship factors associated with concordance with recipients’ viral suppression. AIDS Behav. 2015;19(11):2123–9.
Holzemer WL, Henry SB, Nokes KM, et al. Validation of the sign and symptom check-list for persons with HIV disease (SSC-HIV). J Adv Nurs. 1999;30(5):1041–9.
Allison PD. Causal inference with panel data. Paper presented at the Annual Meeting of the American Sociological Association in August 2005; Philadelphia, PA; 2005.
Bollen KA, Brand JE. A general panel model with random and fixed effects: a structural equations approach. Soc Forces. 2010;89(1):1–34.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55.
Brown TA. Confirmatory factor analysis for applied research. 2nd ed. New York: Guilford Publications; 2014.
Cohen J. Statistical power analysis for the behavioral sciences. Burlington: Elsevier Sciences; 2013.
Bandura A. Social learning theory. Englewood Cliffs: Prentice-Hall; 1977.
Kelley AS, Morrison RS. Palliative care for the seriously ill. N Engl J Med. 2015;373(8):747–55.
Leblanc AJ, London AS, Aneshensel CS. The physical costs of AIDS caregiving. Soc Sci Med. 1997;45(6):915–23.
Acknowledgements
The study was supported by Grants R01 DA019413 and R01NR014050, and the Johns Hopkins Center for AIDS Research Grant 1P30 AI094189 from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The auhtors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Mitchell, M.M., Isenberg, S.R., Maragh-Bass, A.C. et al. Chronic Pain Predicting Reciprocity of Support Among Vulnerable, Predominantly African-American Persons Living with HIV/AIDS. AIDS Behav 22, 2002–2007 (2018). https://doi.org/10.1007/s10461-017-1775-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1775-9