Abstract
Background
The pathogenesis of left ventricular (LV) dysfunction in diabetes has been attracting attention. It has been reported that LV longitudinal systolic myocardial function determined by speckle tracking echocardiography (STE) is associated with diabetic polyneuropathy (DPN). However, the relationship between the severity of peripheral neuropathy and LV myocardial dysfunction is unknown. This study examined the relationship between the severity of DPN and echocardiographic parameters as well as clinical features.
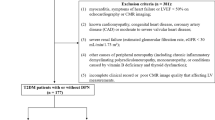
Methods
The subjects were 166 patients (57 ± 14 years old) with diabetes who had a normal LV ejection fraction (≥ 55%). To assess LV longitudinal systolic function, global longitudinal strain (GLS) was calculated by two-dimensional STE as the average peak strain of 18 LV segments in three standard apical views. A nerve conduction study (NCS) was performed in each subject to assess the severity of neuropathy based on the NCS Baba Classification (Grade 0: no apparent abnormalities–Grade IV: abolition). Three nerves in the lower extremity were examined: tibial nerve (F-wave latency, motor nerve conduction velocity, and amplitude), sural nerve (sensory conduction velocity and amplitude), and peroneal nerve (motor nerve conduction velocity and amplitude).
Results
Of the 166 subjects, 112 subjects (67.5%) were confirmed to have DPN, and all the subjects were divided into two groups according to the presence/absence of DPN. When multivariate analysis was performed using significant factors from univariate logistic regression analysis as explanatory variables, GLS was found to be an independent determinant of DPN (odds ratio: 0.55, p < 0.001). In multivariate analysis of NCS data, F-wave latency was the most important determinant of DPN (odds ratio: 1.43, p < 0.001). There was a significant negative correlation between F-wave latency and GLS (r = − 0.43, p < 0.001). Regarding the relation between GLS and the severity of DPN, GLS was significantly lower in patients with Grade I or higher DPN than in patients without DPN, but showed no significant difference between the grades of neuropathy. In addition, GLS was significantly lower when 2–3 lower extremity nerves were affected by DPN than in patients without DPN.
Conclusion
Patients with diabetes may already have subclinical LV myocardial dysfunction when DPN is Grade I. Assessment of LV longitudinal systolic function by GLS may be important in diabetic patients with DPN.






Similar content being viewed by others
References
Rubler S, Dlugash J, Yuceoglu YZ, et al. New type of cardiomyopathy associated with diabetic glomerulosclerosis. Am J Cardiol. 1972;30:595–602.
Boyer JK, Thanigaraj S, Schechtman KB, et al. Prevalence of ventricular diastolic dysfunction in asymptomatic, normotensive patients with diabetes mellitus. Am J Cardiol. 2004;93:870–5.
Enomoto M, Ishizu T, Seo Y, et al. Myocardial dysfunction identified by three-dimensional speckle tracking echocardiography in type 2 diabetes patients relates to complications of microangiopathy. J Cardiol. 2016;68:282–7.
Seino Y, Nanjo K, Tajima N, Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus, et al. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Investig. 2010;1:212–28.
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.
Baba M. Electrophysiological grading of diabetic polyneuropathy by nerve conduction study. Jpn J Clin Neurophysiol. 2013;41:143–50.
International Diabetes Federation. IDF Diabetes Atlas 8th Edition. Brussels, Belgium 2017. https://www.idf.org/e-library/epidemiology-research/diabetes-atlas.html. Accessed Feb 2018
Ministry of Health, Labour and Welfare. Results of Heisei 28 “National Health and Nutrition Survey” [published in Japanese]. Tokyo, Japan 2017[cited 2017 Sep 21]. http://www.mhlw.go.jp/stf/houdou/0000177189.html. Accessed Feb 2018
Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation. 2007;115:3213–23.
Asghar O, Al-Sunni A, Khavandi K, et al. Diabetic cardiomyopathy. Clin Sci (Lond). 2009;116:741–60.
Acar E, Ural D, Bildirici U, et al. Diabetic cardiomyopathy. Anadolu Kardiyol Derg. 2011;11:732–7.
Zhang X, Chen C. A new insight of mechanisms, diagnosis and treatment of diabetic cardiomyopathy. Endocrine. 2012;41:398–409.
Yu CM, Lin H, Yang H, et al. Progression of systolic abnormalities in patients with “isolated” diastolic heart failure and diastolic dysfunction. Circulation. 2002;105:1195–201.
Kato TS, Noda A, Izawa H, et al. Discrimination of nonobstructive hypertrophic cardiomyopathy from hypertensive left ventricular hypertrophy on the basis of strain rate imaging by tissue Doppler ultrasonography. Circulation. 2004;110:3808–14.
Greenbaum RA, Ho SY, Gibson DG, et al. Left ventricular fibre architecture in man. Br Heart J. 1981;45:29–34.
Henein MY, Gibson DG. Normal long axis function. Heart. 1999;81:111–3.
Henein MY, Gibson DG. Long axis function in disease. Heart. 1999;81:229–31.
Stokke TM, Hasselberg NE, Smedsrud MK, et al. Geometry as a confounder when assessing ventricular systolic function: comparison between ejection fraction and strain. J Am Coll Cardiol. 2017;70:942–54.
Ng AC, Delgado V, Bertini M, et al. Findings from left ventricular strain and strain rate imaging in asymptomatic patients with type 2 diabetes mellitus. Am J Cardiol. 2009;104:1398–401.
Nakai H, Takeuchi M, Nishikage T, et al. Subclinical left ventricular dysfunction in asymptomatic diabetic patients assessed by two-dimensional speckle tracking echocardiography: correlation with diabetic duration. Eur J Echocardiogr. 2009;10:926–32.
Ernande L, Bergerot C, Girerd N, et al. Longitudinal myocardial strain alteration is associated with left ventricular remodeling in asymptomatic patients with type 2 diabetes mellitus. J Am Soc Echocardiogr. 2014;27:479–88.
Liu JH, Chen Y, Yuen M, et al. Incremental prognostic value of global longitudinal strain in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2016;15:22.
Holland DJ, Marwick TH, Haluska BA, et al. Subclinical LV dysfunction and 10-year outcomes in type 2 diabetes mellitus. Heart. 2015;101:1061–6.
Fang ZY, Prins JB, Marwick TH. Diabetic cardiomyopathy: evidence, mechanisms, and therapeutic implications. Endocr Rev. 2004;25:543–67.
Stoddard MF, Pearson AC, Kern MJ, et al. Influence of alteration in preload on the pattern of left ventricular diastolic filling as assessed by Doppler echocardiography in humans. Circulation. 1989;79:1226–36.
Nishimura RA, Abel MD, Hatle LK, et al. Relation of pulmonary vein to mitral flow velocities by transesophageal Doppler echocardiography. Effect of different loading condition. Circulation. 1990;81:1488–97.
Hayashi T, Yamada S, Iwano H, et al. Left ventricular global strain for estimating relaxation and filling pressure—a multicenter study. Circ J. 2016;80:1163–70.
Satoh Jo, Baba Masayuki, Yagihashi Soroku, et al. Frequency of diabetic polyneuropathy(DPN) and clinical significance of achilles tendon reflex in diagnosis of DPN-Survey of 15,000 patients in Tohoku, Japan. J Jpn Diabetes Soc. 2007;50:799–806.
Japan Physicians Association research group. Study on Diabetic Neuropathy (1st Report) actual condition and complications of diabetes in Japan. J Jpn Phys Assoc. 2001;16:167–95.
Dyck PJ, Davies JL, Litchy WJ, et al. Longitudinal assessment of diabetic polyneuropathy using a composite score in the Rochester Diabetic Neuropathy Study cohort. Neurology. 1997;49:229–39.
Dyck PJ, Overland CJ, Low PA, et al. Signs and symptoms versus nerve conduction studies to diagnose diabetic sensorimotor polyneuropathy: Cl vs. NPhys trial. Muscle Nerve. 2010;42:157–64.
Ishizu T, Seo Y, Kameda Y, et al. Left ventricular strain and transmural distribution of structural remodeling in hypertensive heart disease. Hypertension. 2014;63:500–6.
Krzesiński P, Uziębło-Życzkowska B, Gielerak G, et al. Global longitudinal two-dimensional systolic strain is associated with hemodynamic alterations in arterial hypertension. J Am Soc Hypertens. 2015;9:680–9.
Kim D, Shim CY, Hong GR, et al. Differences in left ventricular functional adaptation to arterial stiffness and neurohormonal activation in patients with hypertension: a study with two-dimensional layer-specific speckle tracking echocardiography. Clin Hypertens. 2017;23:21.
Andersen H, Stålberg E, Falck B. F-wave latency, the most sensitive nerve conduction parameter in patients with diabetes mellitus. Muscle Nerve. 1997;20:1296–302.
Mochizuki Y, Tanaka H, Matsumoto K, et al. Association of peripheral nerve conduction in diabetic neuropathy with subclinical left ventricular systolic dysfunction. Cardiovasc Diabetol. 2015;14:47.
Low PA, Schmelzer JD, Ward KK. The effect of age on energy metabolism and resistance to ischaemic conduction failure in rat peripheral nerve. J Physiol. 1986;374:263–71.
Yagihashi S. Pathology and pathogenetic mechanisms of diabetic neuropathy. Diabetes Metab Rev. 1995;11:193–225.
Obrosova IG. Diabetes and the peripheral nerve. Biochim Biophys Acta. 2009;1792:931–40.
Nishizawa Y, Wada R, Baba M, et al. Neuropathy induced by exogenously administered advanced glycation end-products in rats. J Diabetes Investig. 2010;1:40–9.
Geraldes P, King GL. Activation of protein kinase C isoforms and its impact on diabetic complications. Circ Res. 2010;106:1319–31.
Yagihashi S, Mizukami H, Sugimoto K. Mechanism of diabetic neuropathy: where are we now and where to go? J Diabetes Investig. 2011;2:18–32.
Takigiku K, Takeuchi M, Izumi C, et al. Normal range of left ventricular 2-dimensional strain: japanese Ultrasound Speckle Tracking of the Left Ventricle (JUSTICE) study. Circ J. 2012;76:2623–32.
Yingchoncharoen T, Agarwal S, Popović ZB, et al. Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr. 2013;26:185–91.
Acknowledgements
The authors thank Kunio Sugiyama and the staff of the neurophysiological laboratory at Toho University Medical Center Omori Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflict of interest in the research associated with this article.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. This research was approved by the Ethics Committee of Toho University Medical Center Omori Hospital (approval No. M17264) and was conducted after the Committee made a decision that informed consent was not required.
About this article
Cite this article
Tabako, S., Harada, M., Sugiyama, K. et al. Association of left ventricular myocardial dysfunction with diabetic polyneuropathy. J Med Ultrasonics 46, 69–79 (2019). https://doi.org/10.1007/s10396-018-0898-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-018-0898-6