Abstract
Objective
We try to establish designs for the macromolecular agents possessing high Gd3+-chelating stability, because free Gd3+ ion released from Gd chelates is known as a risk factor to cause toxic side effects and a safety concern.
Materials and methods
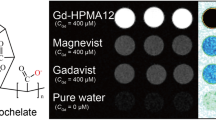
We prepared three types of Gd-based macromolecular MRI contrast agents from a synthetic polymer (poly(glutamic acid) homopolymer or poly(ethylene glycol)-b-poly(lysine) block copolymer) and a chelating moiety (DO3A or DOTA) having two strategic designs for high chelate stability. Then, we examine the in vitro Gd3+-chelate stability of these macromolecular MRI contrast agents.
Results
The prepared macromolecular agents exhibited the same or higher Gd3+-chelate stability as/than did Gd-DOTA that possesses the highest Gd3+-chelate stability among the approved small-MW Gd-chelate MRI contrast agent.
Discussion
Our macromolecular design was considered to work well for high Gd3+-chelate stability.




Similar content being viewed by others
References
Caravan P, Ellison JJ, McMurry TJ, Lauffer RB (1999) Gadolinium(III) chelates as MRI contrast agents: structure, dynamics, and applications. Chem Rev 99:2293–2352. https://doi.org/10.1021/cr980440x
Kubíček V, Tóth É (2009) Design and function of metal complexes as contrast agents in MRI. Adv Inorg Chem 61:63–129. https://doi.org/10.1016/S0898-8838(09)00202-5
Aime S, Caravan PJ (2009) Biodistribution of gadolinium-based contrast agents, including gadolinium deposition. Magn Reson Imaging 30:1259–1267. https://doi.org/10.1002/jmri.21969
Tóth É, Helm L, Merbach AE (2009) Metal complexes as MRI contrast enhancement agents. In: McCleverty JA, Meyer J (eds) Comprehensive coordination chemistry II, vol 9. Elsevier Science, Amsterdam, pp 841–881. https://doi.org/10.1016/B0-08-043748-6/09007-1
Pesaresi I, Cosottini M (2010) MR angiography contrast agents. In: Neri R, Cosottini M, Caramella D (eds) MR angiography of the body technique and clinical application. Springer, New York, pp 7–16. https://doi.org/10.1007/978-3-540-79717-3
Tóth É, Helm L, Merbach AE (2015) Metal complexes as MRI contrast enhancement agents. In: Reference module in chemistry, molecular sciences and chemical engineering. Elsevier, Amsterdam. https://doi.org/10.1016/B978-0-12-409547-2.11263-6
Tweedle MF (1992) Physicochemical properties of gadoteridol and other magnetic resonance contrast agents. Investig Radiol 27(Suppl 1):S7
Marckmann P, Skov L, Rossen K, Dupont A, Damholt MB, Heaf JG, Thomsen HS (2006) Nephrogenic systemic fibrosis: suspected causative role of gadodiamide used for contrast-enhanced magnetic resonance imaging. J Am Soc Nephrol 17:2359–2362. https://doi.org/10.1681/ASN.2006060601
Do C, Barnes JL, Tan C, Wagner B (2014) Type of MRI contrast, tissue gadolinium, and fibrosis. Am J Physiol Renal Physiol 307:F844–855. https://doi.org/10.1152/ajprenal.00379.2014
Thomsen HS, Morcos SK, Dawson P (2006) Is there a causal relation between the administration of gadolinium based contrast media and the development of nephrogenic systemic fibrosis (NSF)? Clin Radiol 61:905–906. https://doi.org/10.1016/j.crad.2006.09.003
Thomsen HS (2006) Nephrogenic systemic fibrosis: a serious late adverse reaction to gadodiamide. Eur Radiol 16:2619–2621. https://doi.org/10.1007/s00330-006-0495-8
Morcos SK (2007) Nephrogenic systemic fibrosis following the administration of extracellular gadolinium based contrast agents: is the stability of the contrast agent molecule an important factor in the pathogenesis of this condition? Br J Radiol 80:73–76. https://doi.org/10.1259/bjr/17111243
Braveman IM, Cowper S (2010) Nephrogenic systemic fibrosis. F1000 Med Rep 2:84. https://doi.org/10.3410/M2-84
Ramalho J, Ramalho M, Jay M, Burke LM, Semelka RC (2016) Gadolinium toxicity and treatment. Magn Reson Imaging 34:1394–1398. https://doi.org/10.1016/j.mri.2016.09.005
Semelka RC, Ramalho M, AlObaidy M, Ramalho J (2016) Gadolinium in humans: a family of disorders. Am J Roentgenol 207:229–233. https://doi.org/10.2214/AJR.15.15842
Hao D, Ai T, Goerner F, Hu X, Runge VM, Tweedle M (2012) MRI contrast agents: basic chemistry and safety. J Magn Reson Imaging 36:1060–1071. https://doi.org/10.1002/jmri.23725
Kanda T, Ishii K, Kawaguchi H, Kitajima K, Takenaka D (2014) High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology 270:834–841. https://doi.org/10.1148/radiol.13131669
Kanda T, Osawa M, Oba H, Toyoda K, Kotoku J, Haruyama T, Takeshita K, Furui S (2015) High signal intensity in dentate nucleus on unenhanced T1-weighted MR images: association with linear versus macrocyclic gadolinium chelate administration. Radiology 275:803–809. https://doi.org/10.1148/radiol.14140364
Kanda T, Fukusato T, Matsuda M, Toyoda K, Oba H, Kotoku J, Haruyama T, Kitajima K, Furui S (2015) Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: evaluation of autopsy brain specimens with inductively coupled plasma mass spectroscopy. Radiology 276:228–232. https://doi.org/10.1148/radiol.2015142690
Kanda T, Nakai Y, Oba H, Toyoda K, Kitajima K, Furui S (2016) Gadolinium deposition in the brain. Magn Reson Imaging 34:1346–1350. https://doi.org/10.1016/j.mri.2016.08.024
Tweedle MF, Hagan JJ, Kumar K, Mantha S, Chang CA (1991) Reaction of gadolinium chelates with endogenously available ions. Magn Reson Imaging 9:409–415
Wedeking P, Kumar K, Tweedle MF (1992) Dissociation of gadolinium chelates in mice: relationship to chemical characteristics. Magn Reson Imaging 10:641–648
Tweedle MF (2016) Gadolinium deposition: is it chelated or dissociated gadolinium? How can we tell? Magn Reson Imaging 34:1377–1382. https://doi.org/10.1016/j.mri.2016.09.003
Idée JM, Port M, Raynal I, Schaefer M, Le Greneur S, Corot C (2006) Clinical and biological consequences of transmetallation induced by contrast agents for magnetic resonance imaging: a review. Fundam Clin Pharmacol 20:563–576. https://doi.org/10.1111/j.1472-8206.2006.00447.x
White GW, Gibby WA, Tweedle MF (2006) Comparison of Gd(DTPA-BMA) (Omniscan) versus Gd(HP-DO3A) (ProHance) relative to gadolinium retention in human bone tissue by inductively coupled plasma mass spectroscopy. Investig Radiol 41:272–278. https://doi.org/10.1097/01.rli.0000186569.32408.95
Gibby WA, Gibby KA, Gibby WA (2004) Comparison of Gd DTPA-BMA (Omniscan) versus Gd HP-DO3A (ProHance) retention in human bone tissue by inductively coupled plasma atomic emission spectroscopy. Investig Radiol 39:138–142
Ostrowitzki S, Fick J, Roberts TP, Wendland MF, Aldape KD, Mann JS, Israel MA, Brasch RC (1998) Comparison of gadopentetate dimeglumine and albumin-(Gd-DTPA)30 for microvessel characterization in an intracranial glioma model. J Magn Reson Imaging 8:799–806. https://doi.org/10.1002/jmri.1880080408
Helbich TH, Gossman A, Mareski PA, Radüchel B, Roberts TP, Shames DM, Mühler M, Turetschek K, Brasch RC (2000) A new polysaccharide macromolecular contrast agent for MR imaging: biodistribution and imaging characteristics. J Magn Reson Imaging 11:694–701. https://doi.org/10.1002/1522-2586(200006)11:6%3c694:AID-JMRI17%3e3.0.CO;2-1
Granato L, Vander Elst L, Henoumont C, Muller RN, Laurent S (2018) Optimizing water exchange rates and rotational mobility for high-relaxivity of a novel Gd-DO3A derivative complex conjugated to inulin as macromolecular contrast agents for MRI. Chem Biodivers 15:e1700487. https://doi.org/10.1002/cbdv.201700487
Lu ZR, Wang X, Parker DL, Goodrich KC, Buswell HR (2003) Poly(l-glutamic acid) Gd(III)-DOTA conjugate with a degradable spacer for magnetic resonance imaging. Bioconj Chem 14:715–719. https://doi.org/10.1021/bc0340464
Ye F, Ke T, Jeong EK, Wang X, Sun Y, Johnson M, Lu ZR (2003) Noninvasive visualization of in vivo drug delivery of poly(l-glutamic acid) using contrast-enhanced MRI. Mol Pharm 3:507–515. https://doi.org/10.1021/mp060052g
Schuhmann-Giampieri G, Schmitt-Willich H, Frenzel T, Press WR, Weinmann HJ (1991) In vivo and in vitro evaluation of Gd-DTPA-polylysine as a macromolecular contrast agent for magnetic resonance imaging. Investig Radiol 26:969–974
Grandin C, Van Beers BE, Demeure R, Goudemant JF, Mottet I, Pringot J (1995) Comparison of gadolinium-DTPA and polylysine-gadolinium-DTPA-enhanced magnetic resonance imaging of hepatocarcinoma in the rat. Investig Radiol 30:572–581
Bogdanov A Jr, Wright SC, Marecos EM, Bogdanova A, Martin C, Petherick P, Weissleder R (1997) A long-circulating co-polymer in “passive targeting” to solid tumors. Drug Target 4:321–330. https://doi.org/10.3109/10611869708995848
Bogdanov AA Jr, Weissleder R, Frank W, Bogdanova AV, Nossif N, Schaffer BK, Tsai E, Papisov MI, Brady TJ (1993) A new macromolecule as a contrast agent for MR angiography: preparation, properties, and animal studies. Radiology 187:701–706. https://doi.org/10.1148/radiology.187.3.8497616
Tombach B, Schneider J, Reimer P, Mahler M, Ebert W, Shams K, Heindel W (2006) CMR 2005: 6.05; Phase I clinical trial of gadomer. Contrast Media Mol Imaging 1:69. https://doi.org/10.1002/cmmi.38
Kobayashi H, Kawamoto S, Choyke PL, Sato N, Knopp MV, Star RA, Waldmann TA, Tagaya Y, Brechbiel MW (2003) Comparison of dendrimer-based macromolecular contrast agents for dynamic micro-magnetic resonance lymphangiography. Magn Reson Med 50:758–766. https://doi.org/10.1002/mrm.10583
Venditto VJ, Regino CA, Brechbiel MW (2005) PAMAM dendrimer based macromolecules as improved contrast agents. Mol Pharm 2:302–311. https://doi.org/10.1021/mp050019e
Ndiaye M, Malytskyi V, Vangijzegem T, Sauvage F, Wels M, Cadiou C, Moreau J, Henoumont C, Boutry S, Muller RN, Harakat D, Smedt S, Laurent S, Chuburu F (2019) Comparison of MRI properties between multimeric DOTAGA and DO3A Gadolinium-Dendron conjugates. Inorg Chem 58:12798–12808. https://doi.org/10.1021/acs.inorgchem.9b01747
Ladd DL, Hollister R, Peng X, Wei D, Wu G, Delecki D, Snow RA, Toner JL, Kellar K, Eck J, Desai VC, Raymond G, Kinter LB, Desser TS, Rubin DL (1999) Polymeric gadolinium chelate magnetic resonance imaging contrast agents: design, synthesis, and properties. Bioconj Chem 10:361–370. https://doi.org/10.1021/bc980086+
Ye Z, Zhou Z, Ayat N, Wu X, Jin E, Shi X, Lu ZR (2016) A neutral polydisulfide containing Gd(III) DOTA monoamide as a redox-sensitive biodegradable macromolecular MRI contrast agent. Contrast Media Mol Imaging 11:32–40. https://doi.org/10.1002/cmmi.1655
Matsumura Y, Maeda H (1986) A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res 46:6387–6392
Maeda H (2012) Macromolecular therapeutics in cancer treatment: the EPR effect and beyond. J Control Release 164:138–144. https://doi.org/10.1016/j.jconrel.2012.04.038
Thonon D, Jacques V, Desreux JF (2007) A gadolinium triacetic monoamide DOTA derivative with a methanethiosulfonate anchor group. Relaxivity properties and conjugation with albumin and thiolated particles. Contrast Media Mol Imaging 2:24–34. https://doi.org/10.1002/cmmi.121
Shiraishi K, Kawano K, Minowa T, Maitani Y, Yokoyama M (2009) Preparation and in vivo imaging of PEG-poly(l-lysine)-based polymeric micelle MRI contrast agents. J Control Release 136:14–20. https://doi.org/10.1016/j.jconrel.2009.01.010
Frenzel T, Lengsfeld P, Schirmer H, Hütter J, Weinmann HJ (2008) Stability of gadolinium-based magnetic resonance imaging contrast agents in human serum at 37 degrees C. Investig Radiol 4:817–828. https://doi.org/10.1097/RLI.0b013e3181852171
Ma H, Shiraishi K, Minowa T, Kawano K, Yokoyama M, Hattori Y, Maitani Y (2010) Accelerated blood clearance was not induced for a gadolinium-containing PEG-poly(l-lysine)-based polymeric micelle in mice. Pharm Res 27:296–302. https://doi.org/10.1007/s11095-009-0018-9
Yokoyama M, Kwon GS, Okano T, Sakurai Y, Seto T, Kataoka K (1992) Preparation of micelle-forming polymer-drug conjugates. Bioconj Chem 3:295–301
Duncan R, Kopecková-Rejmanová P, Strohalm J, Hume I, Cable HC, Pohl J, Lloyd JB, Kopecek J (1987) Anticancer agents coupled to N-(2-hydroxypropyl)methacrylamide copolymers. I. Evaluation of daunomycin and puromycin conjugates in vitro. Br J Cancer 55:165–174. https://doi.org/10.1038/bjc.1987.33
Funding
This research was supported by the Ministry of Education, Science, Sports and Culture, Grant-in-Aid for Scientific Research (B) (No. 26282139).
Author information
Authors and Affiliations
Contributions
Both the authors designed and planned the study. Both the authors synthesized macromolecular agents. MY performed Gd-chelate stability analysis and wrote the first draft of the manuscript, and both the authors contributed to the revision of the manuscript. Both the authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
Since this research does not include any clinical work or animal experiment, we need not any ethical approval or standard for this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yokoyama, M., Shiraishi, K. Stability evaluation of Gd chelates for macromolecular MRI contrast agents. Magn Reson Mater Phy 33, 527–536 (2020). https://doi.org/10.1007/s10334-019-00805-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-019-00805-8