Abstract
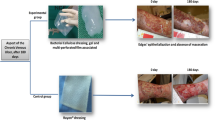
Venous leg ulcer is a pathological condition afflicting prevalently elderly patients, which has been found to have a major impact on individuals’ health and social aspects of quality of life. Actually, the best practice treatment is recommended to include wound dressing and multilayer compression therapy. In this study, we have tested the effectiveness and safety of Vulnamin®, a novel dressing in the form of a metal cellulose gel containing the amino acids glycine, l-lysine, l-proline, l-leucine, and hyaluronic acid, and elastic compressive bandages in the treatment of chronic venous ulcers of the lower limbs. The study has been conducted in two groups of patients, one treated with Vulnamin® plus Ca-alginate (ulcer duration = 25.4 ± 6.2 weeks; mean baseline ulcer area = 13.9 ± 4.5 cm2) and a control group treated with Ca-alginate alone (ulcer duration = 23.4 ± 4.2 weeks; mean baseline ulcer area = 15.1 ± 4.7 cm2). Results have shown that after 70 days of treatment patients significantly ameliorate their pathological condition if they are treated with Vulnamin®, as compared with patients treated with Ca-alginate alone. In fact, at the end of the treatment, complete healing closure was 61% in the group treated with Vulnamin® and, respectively, 27% in the control group. Moreover, ulcer areas showed a significant reduction in patients treated with Vulnamin® (mean ulcer area = 3.04 ± 0.8 cm2), as compared with controls (mean ulcer area = 10.96 ± 3.8 cm2). Overall, the results of this study indicate that Vulnamin® together with elastocompression is safe and more effective than standard dressing together with elastocompression in inducing a faster healing in chronic venous ulcers of the lower limb.





Similar content being viewed by others
References
Nicolaides AN, Hussein MK, Szendro G, Christopoulos D, Vasdekis S, Clarke H (1993) The relation of venous ulceration with ambulatory venous pressure measurements. J Vasc Surg 17:414–419
Pappas PJ, De Fouw DO, Venezio LM et al (1997) Morphometric assessment of the dermal microcirculation in patients with chronic venous insufficiency. J Vasc Surg 26:784–795
Rich A, Mc Lachlan L (2003) How living with a leg ulcer affects peoples’ daily life: a nurse-led study. J Wound Care 12:51–54
Smith PC (2006) The cause of skin damage and leg ulceration in chronic venous disease. Int J Low Extrem Wounds 5:160–168
Partsch H (1991) Compression therapy of legs. J Dermatol Surg Oncol 17:799–905
Moffatt CJ (2002) Four-layer bandaging: from concept to practice. Int J Low Extrem Wounds 1:13–26
Cassino R, Ricci E (2005) Aminoacids and wound bed: a possible interaction for a topic and general treatment in the chronic skin lesion repair. Acta Vulnologica 3:111–115
Cohn IK, Diegelman RF, Lindlab WJ et al (1992) Wound healing: biochemical and clinical aspects. Philadelphia/London, WB Saunders
Banda WJ, Knighton DR, Hunt TK, Werb Z (1992) Isolation of a non mitogenic angiogenic factor from wound fluid. Proc Natl Acad Sci USA 79:7773–7777
Brown LF, Kiang-Teck Y, Berse B et al (1992) Expression of vascular permeability factor (vascular endothelial growth factor) by epidermal keratinocytes during wound healing. J Exp Med 176:1375–1379
Niessen NN, Gamelli RL, Polverini PJ et al (1996) Basic fibroblast growth factor mediates angiogenic activity in early surgical wounds. Surgery 119:465–547
Favia G, Mariggiò MA, Maiorano E, Cassano A, Capodiferro S, Ribatti D (2008) Accelerated wound healing of oral soft tissues and angiogenic effect induced by a pool of aminoacids combined to sodium hyaluronate (AMINOGAM). J Biol Regul Homeost Agents 22:109–116
Vercruysse KP, Prestwich GD (1998) Hyaluronate derivatives in drug delivery. Crit Rev Ther Carrier Syst 15:513–555
Yerushalmi N, Arad A, Margalit R (1994) Molecular and cellular studies of hyaluronic acid-modified liposomes as bioadhesive carriers for topical drug delivery in wound healing. Arch Biochem Biophys 313:267–273
Voinchet V, Vasseur P, Kern J (2006) Efficacy and safety of hyaluronic acid in the management of acute wounds. Am J Dermatol 7:353–357
Barbul A (2008) Proline precursors to sustain mammalian collagen synthesis. J Nutr 138:2021S–2024S
Mock WL, Green PC, Boyer KD (1990) Specificity and pH dependence for acylproline cleavage by prolidase. J Biol Chem 265:19600–19605
Yaron A, Naider F (1993) Proline-dependent structural and biological properties of peptides and proteins. Crit Rev Biochem Mol Biol 28:31–81
Mariggiò MA, Cassano A, Vinella A et al (2009) Enhancement of fibroblast proliferation, collagen biosynthesis, an production of growth factors as a result of combining sodium hyaluronate and aminoacids. Int J Immunopathol Immunopharmacol 22:485–492
Acknowledgments
This study was supported by Errekappa Euroterapici, Milan, Italy.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maggio, G., Armenio, A., Ruccia, F. et al. A new protocol for the treatment of the chronic venous ulcers of the lower limb. Clin Exp Med 12, 55–60 (2012). https://doi.org/10.1007/s10238-011-0136-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-011-0136-7