Abstract
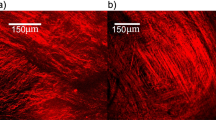
The artery relies on interlamellar structural components, mainly elastin and collagen fibers, for maintaining its integrity and resisting dissection propagation. In this study, the contribution of arterial elastin and collagen fibers to interlamellar bonding was studied through mechanical testing, multiphoton imaging and finite element modeling. Steady-state peeling experiments were performed on porcine aortic media and the purified elastin network in the circumferential (Circ) and longitudinal (Long) directions. The peeling force and energy release rate associated with mode-I failure are much higher for aortic media than for the elastin network. Also, longitudinal peeling exhibits a higher energy release rate and strength than circumferential peeling for both the aortic media and elastin. Multiphoton imaging shows the recruitment of both elastin and collagen fibers within the interlamellar space and points to in-plane anisotropy of fiber distributions as a potential mechanism for the direction-dependent phenomena of peeling tests. Three-dimensional finite element models based on cohesive zone model (CZM) of fracture were created to simulate the peeling tests with the interlamellar energy release rate and separation distance at damage initiation obtained directly from peeling test. Our experimental results show that the separation distance at damage initiation is 80 μm for aortic media and 40 μm for elastin. The damage initiation stress was estimated from the model for aortic media (Circ: 60 kPa; Long: 95 kPa) and elastin (Circ: 9 kPa; Long: 14 kPa). The interlamellar separation distance at complete failure was estimated to be 3 - 4 mm for both media and elastin. Furthermore, elastin and collagen fibers both play an important role in bonding of the arterial wall, while collagen has a higher contribution than elastin to interlamellar stiffness, strength and toughness. These results on microstructural interlamellar failure shed light on the pathological development and progression of aortic dissection.








Similar content being viewed by others
References
Barenblatt GI (1962) The mathematical theory of equilibrium cracks in brittle fracture. Adv Appl Mech 7:55–129. https://doi.org/10.1016/S0065-2156(08)70121-2
Blount KJ, Hagspiel KD (2009) Aortic diameter, true lumen, and false lumen growth rates in chronic type B aortic dissection. AJR Am J Roentgenol 192:W222–W229. https://doi.org/10.2214/AJR.07.3986
Carson MW, Roach MR (1990) The strength of the aortic media and its role in the propagation of aortic dissection. J Biomech 23:579–588. https://doi.org/10.1016/0021-9290(90)90050-D
Chitsaz S, Azadani AN, Matthews PB, Chuter TA, Tseng EE, Ge L (2012) Hemodynamic determinants of aortic dissection propagation by 2D computational modeling: implications for endovascular stent-grafting. J Cardiovasc Surg 53:631–640
Chow MJ, Choi M, Yun SH, Zhang Y (2013a) The effect of static stretch on elastin degradation in arteries. PLoS ONE 8:e81951. https://doi.org/10.1371/journal.pone.0081951
Chow MJ, Mondonedo JR, Johnson VM, Zhang Y (2013b) Progressive structural and biomechanical changes in elastin degraded aorta. Biomech Model Mechanobiol 12:361–372. https://doi.org/10.1007/s10237-012-0404-9
Chow MJ, Turcotte R, Lin CP, Zhang Y (2014) Arterial extracellular matrix: a mechanobiological study of the contributions and interactions of elastin and collagen. Biophys J 106:2684–2692. https://doi.org/10.1016/j.bpj.2014.05.014
Dillon-Murphy D, Noorani A, Nordsletten D, Figueroa CA (2016) Multi-modality image-based computational analysis of haemodynamics in aortic dissection. Biomech Model Mechanobiol 15:857–876. https://doi.org/10.1007/s10237-015-0729-2
Doyle BJ, Norman PE (2016) Computational biomechanics in thoracic aortic dissection: today’s approaches and tomorrow’s opportunities. Ann Biomed Eng 44:71–83. https://doi.org/10.1007/s10439-015-1366-8
Dugdale DS (1960) Yielding of steel sheets containing slits. J Mech Phys Solids 8:100–104. https://doi.org/10.1016/0022-5096(60)90013-2
Erbel R, Alfonso F, Boileau C, Dirsch O, Eber B, Haverich A, Rakowski H, Struyven J, Radegran K, Sechtem U, Taylor J, Zollikofer Ch, Klein WW, Mulder B, Providencia LA (2001) Diagnosis and management of aortic dissection: recommendations of the Task Force on Aortic Dissection, European Society of Cardiology. Eur Heart J 22:1642–1681. https://doi.org/10.1053/euhj.2001.2782
Ferrara A, Pandolfi A (2008) Numerical modelling of fracture in human arteries. Comput Methods Biomech Biomed Eng 11:553–567. https://doi.org/10.1080/10255840701771743
Ferrara A, Pandolfi A (2010) A numerical study of arterial media dissection processes. Int J Fract 166:21–33. https://doi.org/10.1007/s10704-010-9480-y
Gasser TC, Holzapfel GA (2006) Modeling the propagation of arterial dissection. Eur J Mech A Solids 25:617–633. https://doi.org/10.1016/j.euromechsol.2006.05.004
Gasser TC, Ogden RW, Holzapfel GA (2006) Hyperelastic modelling of arterial layers with distributed collagen fibre orientations. J R Soc Interface 3:15–35. https://doi.org/10.1098/rsif.2005.0073
Gentleman E, Lay AN, Dickerson DA, Nauman EA, Livesay GA, Dee KC (2003) Mechanical characterization of collagen fibers and scaffolds for tissue engineering. Biomaterials 24:3805–3813. https://doi.org/10.1016/S0142-9612(03)00206-0
Gültekin O, Holzapfel GA (2018) A brief review on computational modeling of rupture in soft biological tissues. In: Oñate E, Peric D, de Souza Neto E, Chiumenti M (eds) Advances in computational plasticity. Computational methods in applied sciences, vol 46. Springer, Cham, pp 113–144. https://doi.org/10.1007/978-3-319-60885-3_6
Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, Evangelista A, Fattori R, Suzuki T, Oh JK, Moore AG, Malouf JF, Pape LA, Gaca C, Sechtem U, Lenferink S, Deutsch HJ, Diedrichs H, Marcos y Robles J, Llovet A, Gilon D, Das SK, Armstrong WF, Deeb GM, Eagle KA (2000) The international registry of acute aortic dissection (IRAD): new insights into an old disease. JAMA 283:897–903. https://doi.org/10.1001/jama.283.7.897
Holzapfel GA, Gasser TC, Ogden RW (2000) A new constitutive framework for arterial wall mechanics and a comparative study of material models. J Elast 61:1–48. https://doi.org/10.1023/a:1010835316564
Holzapfel GA, Sommer G, Gasser CT, Regitnig P (2005) Determination of layer-specific mechanical properties of human coronary arteries with nonatherosclerotic intimal thickening and related constitutive modeling. Am J Physiol Heart Circ Physiol 289:H2048–H2058. https://doi.org/10.1152/ajpheart.00934.2004
Holzapfel GA, Sommer G, Auer M, Regitnig P, Ogden RW (2007) Layer-specific 3D residual deformations of human aortas with non-atherosclerotic intimal thickening. Ann Biomed Eng 35:530–545. https://doi.org/10.1007/s10439-006-9252-z
Khan IA, Nair CK (2002) Clinical, diagnostic, and management perspectives of aortic dissection. Chest 122:311–328. https://doi.org/10.1378/chest.122.1.311
Leng X, Chen X, Deng X, Sutton MA, Lessner SM (2015) Modeling of experimental atherosclerotic plaque delamination. Ann Biomed Eng 43:2838–2851. https://doi.org/10.1007/s10439-015-1357-9
Leng X, Davis LA, Deng X, Sutton MA, Lessner SM (2016) Numerical modeling of experimental human fibrous cap delamination. J Mech Behav Biomed Mater 59:322–336. https://doi.org/10.1016/j.jmbbm.2016.02.011
Leng X, Zhou B, Deng X, Davis L, Lessner SM, Sutton MA, Shazly T (2018) Experimental and numerical studies of two arterial wall delamination modes. J Mech Behav Biomed Mater 77:321–330. https://doi.org/10.1016/j.jmbbm.2017.09.025
Lillie MA, Gosline JM (2002) The viscoelastic basis for the tensile strength of elastin. Int J Biol Macromol 30:119–127. https://doi.org/10.1016/S0141-8130(02)00008-9
Lu Q, Ganesan K, Simionescu DT, Vyavahare NR (2004) Novel porous aortic elastin and collagen scaffolds for tissue engineering. Biomaterials 25:5227–5237. https://doi.org/10.1016/j.biomaterials.2003.12.019
MacLean NF, Dudek NL, Roach MR (1999) The role of radial elastic properties in the development of aortic dissections. J Vasc Surg 29:703–710. https://doi.org/10.1016/S0741-5214(99)70317-4
Manopoulos C, Karathanasis I, Kouerinis I, Angouras DC, Lazaris A, Tsangaris S, Sokolis DP (2018) Identification of regional/layer differences in failure properties and thickness as important biomechanical factors responsible for the initiation of aortic dissections. J Biomech 80:102–110. https://doi.org/10.1016/j.jbiomech.2018.08.024
Mattson JM, Turcotte R, Zhang Y (2017) Glycosaminoglycans contribute to extracellular matrix fiber recruitment and arterial wall mechanics. Biomech Model Mechanobiol 16:213–225. https://doi.org/10.1007/s10237-016-0811-4
Merei B, Badel P, Davis L, Sutton MA, Avril S, Lessner SM (2017) Atherosclerotic plaque delamination: experiments and 2D finite element model to simulate plaque peeling in two strains of transgenic mice. J Mech Behav Biomed Mater 67:19–30. https://doi.org/10.1016/j.jmbbm.2016.12.001
Nienaber CA, Clough RE (2015) Management of acute aortic dissection. Lancet 385:800–811. https://doi.org/10.1016/S0140-6736(14)61005-9
Nienaber CA, Clough RE, Sakalihasan N, Suzuki T, Gibbs R, Mussa F, Jenkins MP, Thompson MM, Evangelista A, Yeh JS, Cheshire N, Rosendahl U, Pepper J (2016) Aortic dissection. Nat Rev Dis Primers 2:16053. https://doi.org/10.1038/nrdp.2016.53
Noble C, Smulders N, Lewis R, Carré MJ, Franklin SE, MacNeil S, Taylor ZA (2016) Controlled peel testing of a model tissue for diseased aorta. J Biomech 49:3667–3675. https://doi.org/10.1016/j.jbiomech.2016.09.040
O’Connell MK, Murthy S, Phan S, Xu C, Buchanan JA, Spilker R, Dalman RL, Zarins CK, Denk W, Taylor CA (2008) The three-dimensional micro- and nanostructure of the aortic medial lamellar unit measured using 3D confocal and electron microscopy imaging. Matrix Biol 27:171–181. https://doi.org/10.1016/j.matbio.2007.10.008
Pal S, Tsamis A, Pasta S, D’Amore A, Gleason TG, Vorp DA, Maiti S (2014) A mechanistic model on the role of “radially-running” collagen fibers on dissection properties of human ascending thoracic aorta. J Biomech 47:981–988. https://doi.org/10.1016/j.jbiomech.2014.01.005
Pasta S, Phillippi JA, Gleason TG, Vorp DA (2012) Effect of aneurysm on the mechanical dissection properties of the human ascending thoracic aorta. J Thorac Cardiovasc Surg 143:460–467. https://doi.org/10.1016/j.jtcvs.2011.07.058
Pasta S, Phillippi JA, Tsamis A, D’Amore A, Raffa GM, Pilato M, Scardulla C, Watkins SC, Wagner WR, Gleason TG, Vorp DA (2016) Constitutive modeling of ascending thoracic aortic aneurysms using microstructural parameters. Med Eng Phys 38:121–130. https://doi.org/10.1016/j.medengphy.2015.11.001
Rajagopal K, Bridges C, Rajagopal KR (2007) Towards an understanding of the mechanics underlying aortic dissection. Biomech Model Mechanobiol 6:345–359. https://doi.org/10.1007/s10237-006-0069-3
Rasmussen BL, Bruenger E, Sandberg LB (1975) A new method for purification of mature elastin. Anal Biochem 64:255–259. https://doi.org/10.1016/0003-2697(75)90426-1
Rinaudo A, D’Ancona G, Lee JJ, Pilato G, Amaducci A, Baglini R, Follis F, Pilato M, Pasta S (2014) Predicting outcome of aortic dissection with patent false lumen by computational flow analysis. Cardiovasc Eng Technol 5:176–188. https://doi.org/10.1007/s13239-014-0182-x
Roach MR, Song SH (1994) Variations in strength of the porcine aorta as a function of location. Clin Invest Med 17:308–318
Roccabianca S, Ateshian GA, Humphrey JD (2014a) Biomechanical roles of medial pooling of glycosaminoglycans in thoracic aortic dissection. Biomech Model Mechanobiol 13:13–25. https://doi.org/10.1007/s10237-013-0482-3
Roccabianca S, Bellini C, Humphrey JD (2014b) Computational modelling suggests good, bad and ugly roles of glycosaminoglycans in arterial wall mechanics and mechanobiology. J R Soc Interface 11:20140397. https://doi.org/10.1098/rsif.2014.0397
Schellekens JCJ, De Borst R (1993) On the numerical integration of interface elements. Int J Numer Methods Eng 36:43–66. https://doi.org/10.1002/nme.1620360104
Shen ZL, Dodge MR, Kahn H, Ballarini R, Eppell SJ (2008) Stress–strain experiments on individual collagen fibrils. Biophys J 95:3956–3963. https://doi.org/10.1529/biophysj.107.124602
Sherifova S, Holzapfel GA (2019) Biomechanics of aortic wall failure with a focus on dissection and aneurysm: a review. Acta Biomater 99:1–17. https://doi.org/10.1016/j.actbio.2019.08.017
Sommer G, Gasser TC, Auer M, Regitnig P, Holzapfel GA (2008) Dissection properties of the human aortic media: an experimental study. J Biomech Eng 130:021007. https://doi.org/10.1115/1.2898733
Spittell PC, Spittell JA, Joyce JW, Tajik AJ, Edwards WD, Schaff HV, Stanson AW (1993) Clinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990). Mayo Clin Proc 68:642–651. https://doi.org/10.1016/S0025-6196(12)60599-0
Sugita S, Matsumoto T (2018) Local distribution of collagen fibers determines crack initiation site and its propagation direction during aortic rupture. Biomech Model Mechanobiol 17:577–587. https://doi.org/10.1007/s10237-017-0979-2
Tam ASM, Sapp MC, Roach MR (1998) The effect of tear depth on the propagation of aortic dissections in isolated porcine thoracic aorta. J Biomech 31:673–676. https://doi.org/10.1016/S0021-9290(98)00058-X
Tang Y, Ballarini R, Buehler MJ, Eppell SJ (2010) Deformation micromechanisms of collagen fibrils under uniaxial tension. J R Soc Interface 7:839–850. https://doi.org/10.1098/rsif.2009.0390
Thubrikar MJ, Agali P, Robicsek F (1999) Wall stress as a possible mechanism for the development of transverse intimal tears in aortic dissections. J Med Eng Technol 23:127–134. https://doi.org/10.1080/030919099294177
Thunes JR, Phillippi JA, Gleason TG, Vorp DA, Maiti S (2018) Structural modeling reveals microstructure-strength relationship for human ascending thoracic aorta. J Biomech 71:84–93. https://doi.org/10.1016/j.jbiomech.2018.01.037
Tiessen IM, Roach MR (1993) Factors in the initiation and propagation of aortic dissections in human autopsy aortas. J Biomech Eng 115:123–125. https://doi.org/10.1115/1.2895461
Tong J, Sommer G, Regitnig P, Holzapfel GA (2011) Dissection properties and mechanical strength of tissue components in human carotid bifurcations. Ann Biomed Eng 39:1703–1719. https://doi.org/10.1007/s10439-011-0264-y
Tong J, Cohnert T, Regitnig P, Kohlbacher J, Birner-Gruenberger R, Schriefl AJ, Sommer G, Holzapfel GA (2014) Variations of dissection properties and mass fractions with thrombus age in human abdominal aortic aneurysms. J Biomech 47:14–23. https://doi.org/10.1016/j.jbiomech.2013.10.027
Tong J, Cheng Y, Holzapfel GA (2016) Mechanical assessment of arterial dissection in health and disease: advancements and challenges. J Biomech 49:2366–2373. https://doi.org/10.1016/j.jbiomech.2016.02.009
Tsamis A, Phillippi JA, Koch RG, Pasta S, D’Amore A, Watkins SC, Wagner WR, Gleason TG, Vorp DA (2013) Fiber micro-architecture in the longitudinal-radial and circumferential-radial planes of ascending thoracic aortic aneurysm media. J Biomech 46:2787–2794. https://doi.org/10.1016/j.jbiomech.2013.09.003
Turon A, Dávila CG, Camanho PP, Costa J (2007) An engineering solution for mesh size effects in the simulation of delamination using cohesive zone models. Eng Fract Mech 74:1665–1682. https://doi.org/10.1016/j.engfracmech.2006.08.025
Valiaev A, Dong WL, Schmidler S, Clark RL, Chilkoti A, Zauscher S (2008) Hydration and conformational mechanics of single, end-tethered elastin-like polypeptides. J Am Chem Soc 130:10939–10946. https://doi.org/10.1021/ja800502h
Wang Y, Ning J, Johnson JA, Sutton MA, Lessner SM (2011) Development of a quantitative mechanical test of atherosclerotic plaque stability. J Biomech 44:2439–2445. https://doi.org/10.1016/j.jbiomech.2011.06.026
Wang Y, Johnson JA, Spinale FG, Sutton MA, Lessner SM (2014) Quantitative measurement of dissection resistance in intimal and medial layers of human coronary arteries. Exp Mech 54:677–683. https://doi.org/10.1007/s11340-013-9836-0
Wang Y, Zeinali-Davarani S, Davis EC, Zhang Y (2015) Effect of glucose on the biomechanical function of arterial elastin. J Mech Behav Biomed Mater 49:244–254. https://doi.org/10.1016/j.jmbbm.2015.04.025
Wang L, Roper SM, Hill NA, Luo X (2017) Propagation of dissection in a residually-stressed artery model. Biomech Model Mechanobiol 16:139–149. https://doi.org/10.1007/s10237-016-0806-1
Wenger MPE, Bozec L, Horton MA, Mesquidaz P (2007) Mechanical properties of collagen fibrils. Biophys J 93:1255–1263. https://doi.org/10.1529/biophysj.106.103192
Wolinsky H, Glagov S (1964) Structural basis for the static mechanical properties of the aortic media. Circ Res 14:400–413. https://doi.org/10.1161/01.RES.14.5.400
Wolinsky H, Glagov S (1967) A lamellar unit of aortic medial structure and function in mammals. Circ Res 20:99–111. https://doi.org/10.1161/01.RES.20.1.99
Yu X, Turcotte R, Seta F, Zhang Y (2018a) Micromechanics of elastic lamellae: unravelling the role of structural inhomogeneity in multi-scale arterial mechanics. J R Soc Interface 15:20180492. https://doi.org/10.1098/rsif.2018.0492
Yu X, Wang Y, Zhang Y (2018b) Transmural variation in elastin fiber orientation distribution in the arterial wall. J Mech Behav Biomed Mater 77:745–753. https://doi.org/10.1016/j.jmbbm.2017.08.002
Yu X, Suki B, Zhang Y (2020) Avalanches and power law behavior in aortic dissection propagation. Sci Adv 6:eaaz1173. https://doi.org/10.1126/sciadv.aaz1173
Zeinali-Davarani S, Chow MJ, Turcotte R, Zhang Y (2013) Characterization of biaxial mechanical behavior of porcine aorta under gradual elastin degradation. Ann Biomed Eng 41:1528–1538. https://doi.org/10.1007/s10439-012-0733-y
Zhang Y, Lu Q, Feng J, Yu P, Zhang S, Teng Z, Gillard JH, Song R, Jing Z (2014) A pilot study exploring the mechanisms involved in the longitudinal propagation of acute aortic dissection through computational fluid dynamic analysis. Cardiology 128:220–225. https://doi.org/10.1159/000358041
Zou Y, Zhang Y (2009) An experimental and theoretical study on the anisotropy of elastin network. Ann Biomed Eng 37:1572–1583. https://doi.org/10.1007/s10439-009-9724-z
Acknowledgements
This study was supported by a Grant from the National Heart, Lung, and Blood Institute, National Institute of Health (2R01HL098028).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, R., Yu, X. & Zhang, Y. Mechanical and structural contributions of elastin and collagen fibers to interlamellar bonding in the arterial wall. Biomech Model Mechanobiol 20, 93–106 (2021). https://doi.org/10.1007/s10237-020-01370-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-020-01370-z