Abstract
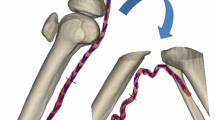
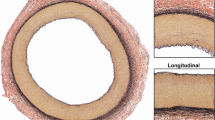
Femoropopliteal artery (FPA) reconstructions are notorious for poor clinical outcomes. Mechanical and flow conditions that occur in the FPA with limb flexion are thought to play a significant role, but are poorly characterized. FPA deformations due to acute limb flexion were quantified using a human cadaver model and used to build a finite element model that simulated surrounding tissue forces associated with limb flexion-induced deformations. Strains and intramural principal mechanical stresses were determined for seven age groups. Computational fluid dynamics analysis was performed to assess hemodynamic variables. FPA shape, stresses, and hemodynamics significantly changed with age. Younger arteries assumed straighter positions in the flexed limb with less pronounced bends and more uniform stress distribution along the length of the artery. Even in the flexed limb posture, FPAs younger than 50 years of age experienced tension, while older FPAs experienced compression. Aging resulted in localization of principal mechanical stresses to the adductor hiatus and popliteal artery below the knee that are typically prone to developing vascular pathology. Maximum principal stresses in these areas increased threefold to fivefold with age with largest increase observed at the adductor hiatus. Atheroprotective wall shear stress reduced after 35 years of age, and atheroprone and oscillatory shear stresses increased after the age of 50. These data can help better understand FPA pathophysiology and can inform the design of targeted materials and devices for peripheral arterial disease treatments.






Similar content being viewed by others
References
Adam DJ, Beard JD, Cleveland T et al (2005) Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet 366:1925–34. doi:10.1016/S0140-6736(05)67704-5
Ansari F, Pack LK, Brooks SS, Morrison TM (2013) Design considerations for studies of the biomechanical environment of the femoropopliteal arteries. J Vasc Surg 58:804–813. doi:10.1016/j.jvs.2013.03.052
Antiga L, Piccinelli M, Botti L et al (2008) An image-based modeling framework for patient-specific computational hemodynamics. Med Biol Eng Comput 46:1097–1112. doi:10.1007/s11517-008-0420-1
Birukov KG (2009) Cyclic stretch, reactive oxygen species, and vascular remodeling. Antioxid Redox Signal 11:1651–1667. doi:10.1089/ars.2008.2390
Cheng C, Wilson N, Hallett R (2006) In vivo MR angiographic quantification of axial and twisting deformations of the superficial femoral artery resulting from maximum hip and knee flexion. J Vasc Interv Radiol 17:979–987. doi:10.1097/01.RVI.0000220367.62137.E8
Cheng CP, Choi G, Herfkens RJ, Taylor C a et al (2010) The effect of aging on deformations of the superficial femoral artery resulting from hip and knee flexion: potential clinical implications. J Vasc Interv Radiol 21:195–202. doi:10.1016/j.jvir.2009.08.027
Clowes AW, Reidy MA, Clowes MM (1983) Mechanisms of stenosis after arterial injury. Lab Invest 49:208–215
Conte MS, Bandyk DF, Clowes AW et al (2006) Results of PREVENT III: a multicenter, randomized trial of edifoligide for the prevention of vein graft failure in lower extremity bypass surgery. J Vasc Surg 43:742–751. doi:10.1016/j.jvs.2005.12.058
Desyatova A, MacTaggart J, Poulson W et al (2017a) The choice of a constitutive formulation for modeling limb flexion-induced deformations and stresses in the human femoropopliteal arteries of different ages. Biomech Model Mechanobiol 16:775–785. doi:10.1007/s10237-016-0852-8
Desyatova A, Poulson W, Deegan P et al (2017b) Limb flexion-induced twist and associated intramural stresses in the human femoropopliteal artery. J R Soc Interface. doi:10.1098/rsif.2017.0025
Dunlop GR, Santos R (1957) Adductor-canal thrombosis. N Engl J Med 256:577–580. doi:10.1056/NEJM195703282561301
Greenwald S (2007) Ageing of the conduit arteries. J Pathol 211:157–172. doi:10.1002/path
Higashiura W, Kubota Y, Sakaguchi S et al (2009) Prevalence, factors, and clinical impact of self-expanding stent fractures following iliac artery stenting. J Vasc Surg 49:645–652. doi:10.1016/j.jvs.2008.10.019
Iida O, Nanto S, Uematsu M et al (2006) Effect of exercise on frequency of stent fracture in the superficial femoral artery. Am J Cardiol 98:272–274
Jani B, Rajkumar C (2006) Ageing and vascular ageing. Postgrad Med J 82:357–62. doi:10.1136/pgmj.2005.036053
Kamenskiy AV, Pipinos II, Dzenis Y a (2015) Effects of age on the physiological and mechanical characteristics of human femoropopliteal arteries. Acta Biomater 11:304–313. doi:10.1016/j.actbio.2014.09.050
Kamenskiy A, Seas A, Bowen G et al (2016) In situ longitudinal pre-stretch in the human femoropopliteal artery. Acta Biomater 32:231–237. doi:10.1016/j.actbio.2016.01.002
Kamenskiy A, Seas A, Deegan P et al (2017) Constitutive description of human femoropopliteal artery aging. Biomech Model Mechanobiol 16:681–692. doi:10.1007/s10237-016-0845-7
Klein AJ, Chen SJ, Messenger JC et al (2009) Quantitative assessment of the conformational change in the femoropopliteal artery with leg movement. Catheter Cardiovasc Interv 74:787–798
Lakatta EG, Wang M, Najjar SS (2009) Arterial aging and subclinical arterial disease are fundamentally intertwined at macroscopic and molecular levels. Med Clin North Am 93:583–604. doi:10.1016/j.mcna.2009.02.008
Learoyd BM, Taylor MG (1966) Alterations with age in the viscoelastic properties of human arterial walls. Circ Res 18:278–292. doi:10.1161/01.RES.18.3.278
Lee H-Y, Oh B-H (2010) Aging and arterial stiffness. Circ J 74:2257–2262. doi:10.1253/circj.CJ-10-0910
MacTaggart J, Phillips N, Lomneth C et al (2014) Three-dimensional bending, torsion and axial compression of the femoropopliteal artery during limb flexion. J Biomech 47:2249–2256
Mahoney EM, Wang K, Cohen DJ et al (2008) One-year costs in patients with a history of or at risk for atherothrombosis in the United States. Circ Cardiovasc Qual Outcomes 1:38–45. doi:10.1161/CIRCOUTCOMES.108.775247
Malek AM, Alper SL, Izumo S (1999) Hemodynamics shear stress and its role in atherosclerosis. JAMA 282(21):2035–2042
Mantella LE, Quan A, Verma S (2015) Variability in vascular smooth muscle cell stretch-induced responses in 2D culture. Vasc Cell 7:7. doi:10.1186/s13221-015-0032-0
Newcomer SC, Sauder CL, Kuipers NT et al (2008) Effects of posture on shear rates in human brachial and superficial femoral arteries. Am J Physiol Heart Circ Physiol 294:H1833–9. doi:10.1152/ajpheart.01108.2007
Ní Ghriallais R, Bruzzi M (2013) Effects of knee flexion on the femoropopliteal artery: a computational study. Med Eng Phys 35:1620–8. doi:10.1016/j.medengphy.2013.05.015
Nikanorov A, Smouse HB, Osman K et al (2008) Fracture of self-expanding nitinol stents stressed in vitro under simulated intravascular conditions. J Vasc Surg 48:435–440. doi:10.1016/j.jvs.2008.02.029
Nolan DR, Gower a L, Destrad e M et al (2014) A robust anisotropic hyperelastic formulation for the modelling of soft tissue. J Mech Behav Biomed Mater 39:48–60. doi:10.1016/j.jmbbm.2014.06.016
O’Rourke MF (2007) Arterial aging: pathophysiological principles. Vasc Med 12:329–41. doi:10.1177/1358863X07083392
Palma EC (1959) Hemodynamic arteriopathy. Angiology 10:134–43
Passerini T, Quaini A, Villa U et al (2013) Validation of an open source framework for the simulation of blood flow in rigid and deformable vessels. Int J Numer Methods Biomed Eng 29:1192–1213. doi:10.1002/cnm.2568
Patel DJ, Greenfield JC, Austen WG et al (1965) Pressure-flow relationships in the ascending aorta and femoral artery of man. J Appl Physiol 20:459–463
Poulson W, Kamenskiy A, Seas A et al (2017) Limb flexion-induced axial compression and bending in human femoropopliteal artery segments. J Vasc Surg. doi:10.1016/j.jvs.2017.01.071
Schillinger M, Sabeti S, Loewe C (2006) Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med 354:1879–1888
Schillinger M, Sabeti S, Dick P et al (2007) Sustained benefit at 2 years of primary femoropopliteal stenting compared with balloon angioplasty with optional stenting. Circulation 115:2745–9. doi:10.1161/CIRCULATIONAHA.107.688341
Smouse BHB, Nikanorov A, Laflash D (2005) Biomechanical forces in the femoropopliteal arterial segment. Endovasc Today 4:60–66
Watt J (1965) Origin of femoro-popliteal occlusions. Br Med J 2:1455–1459
Wensing PJW, Meiss L, Mali WPTM, Hillen B (1998) Early atherosclerotic lesions spiraling through the femoral artery. Arterioscler Thromb Vasc Biol 18:1554–1558. doi:10.1161/01.ATV.18.10.1554
Acknowledgements
The authors wish to acknowledge the Charles and Mary Heider Fund for Excellence in Vascular Surgery for their help and support. Computational fluid dynamics simulations were carried out within the joint initiative of CINECA and the Lombardy region LISA under the project B-BeST (bringing biomedical simulations to clinical target).
Funding Research reported in this publication was supported in part by National Heart, Lung, and Blood Institute of the National Institutes of Health (Grant Nos. R01 HL125736 and F32 HL124905).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Desyatova, A., MacTaggart, J., Romarowski, R. et al. Effect of aging on mechanical stresses, deformations, and hemodynamics in human femoropopliteal artery due to limb flexion. Biomech Model Mechanobiol 17, 181–189 (2018). https://doi.org/10.1007/s10237-017-0953-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-017-0953-z