Abstract
Background
Long-term outcomes of children with nephrotic syndrome have not been well described in the literature.
Methods
Cross-sectional study data analysis of n = 43 patients with steroid-sensitive (SSNS) and n = 7 patients with steroid-resistant (SRNS) nephrotic syndrome were retrospectively collected; patients were clinically examined at a follow-up visit (FUV), on average 30 years after onset, there was the longest follow-up period to date.
Results
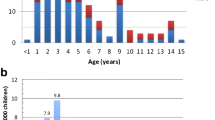
The mean age at FUV was 33.6 years (14.4–50.8 years, n = 41). The mean age of patients with SSNS at onset was 4.7 years (median 3.8 years (1.2–14.5 years), the mean number of relapses was 5.8 (0 to 29 relapses). Seven patients (16.3%) had no relapses. Eleven patients were “frequent relapsers” (25.6%) and four patients still had relapses beyond the age of 18 years. Except of cataracts and arterial hypertension, there were no negative long-term outcomes and only one patient was using immunosuppressant therapy at FUV. 55% of patients suffered from allergies and 47.5% had hypercholesterolemia. Two patients suffered a heart attack in adulthood. A younger age at onset (< 4 years) was a risk factor for frequent relapses. An early relapse (within 6 months after onset) was a risk factor and a low birth weight was not a significant risk factor for a complicated NS course. The mean age of patients with SRNS at onset was 4.6 ± 4.4 years and 27.5 ± 9.9 years at FUV. Three patients received kidney transplantations.
Conclusions
The positive long-term prognosis of SSNS can reduce the concern of parents about the probability of the child developing a chronic renal disease during the clinical course after onset.


Similar content being viewed by others
Availability of data and material
The data sets used and/or analyzed during the current study are available from Dr. I. Franke/ Dr. R. Hagemann on reasonable request at Department of General Pediatrics, University Children’s Hospital Bonn, Germany, and will be shared with scientists/researcher upon request to Dr. I. Franke or Dr. R. Hagemann.
Abbreviations
- AH:
-
Arterial hypertension
- AP:
-
Alkaline phosphatase
- BMI:
-
Body mass index
- DPD:
-
Deoxypyridinoline
- ESPED:
-
Erhebungseinheit für seltene pädiatrische Erkrankungen in Deutschland
- FSGS:
-
Focal segmental glomerulosclerosis
- FUV:
-
Follow-up visit
- M:
-
Mean
- MCNS:
-
Minimal change nephrotic syndrome
- MG:
-
Membranous glomerulonephritis
- NS:
-
Nephrotic syndrome
- SSNS:
-
Steroid-sensitive nephrotic syndrome
- SRNS:
-
Steroid-resistant nephrotic syndrome.
References
International Study of Kidney Disease in Children/ISKDC. The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. J Pediatr. 1981;98:561–4.
Nash MA, Edelmann CM Jr, Bernstein J, Barnett HL. Minimal change nephrotic syndrome, diffuse mesangial hypercellularity and focal glomerulosclerosis. In: Edelmann CM Jr, editor. Pediatric kidney disease. 2nd ed. Boston: Little, Brown; 1992. pp. 1267–90.
Hussain N, Zello JA, Vasilevska-Ritovska J, Banh TM, Patel VP, Patel P, et al. The rationale and design of Insight into Nephrotic Syndrome: Investigating Genes, Health and Therapeutics (INSIGHT): a prospective cohort study of childhood nephrotic syndrome. BMC Nephrology. 2013;14:25. https://doi.org/10.1186/1471-2369-14-25.
Franke I, Aydin M, Llamas Lopez CE, Kurylowicz L, Ganschow R, et al. The incidence of the nephrotic syndrome in childhood in Germany. Clin Exp Nephrol. 2018;22(1):126–32. https://doi.org/10.1007/s10157-017-1433-6.
Bagga A, Mantan M. Nephrotic syndrome in children. Indian J Med Res. 2005;122:13–28.
International Study of Kidney Disease in Children/ISKDC. Early identification of frequent relapsers among children with minimal change nephrotic syndrome. J Pediatr. 1982;101:514–8.
Tarshish P, Tobin JN, Bernstein J, Edelmann CM Jr. Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol. 1997;8:769–76.
Broyer M, Meyrier A, Niaudet P, Habib R. Minimal changes and focal segmental glomerular sclerosis. In: Davison AM, editor. Oxford textbook of clinical nephrology. 2nd ed. Vol. 1. Oxford: Oxford university Press; 1998. pp. 493–535.
Gipson DS, Chin H, Presler TP, et al. Differential risk of remission and ESRD in childhood FSGS. Pediatr Nephrol. 2006;21:344–9.
Siegel NJ, Goldberg B, Krassner LS, Hayslett JP. Long-term follow-up of children with steroid-responsive nephrotic syndrome. J Pediatr. 1972;81:251–8.
Fakhouri F, Bocquet N, Taupin P, Presne C, Gagnadoux MF, Landais P, Lesavre P, Chauveau D, Knebelmann B, Broyer M, Grünfeld JP, Niaudet P. Steroid-sensitive nephrotic syndrome: from childhood to adulthood. Am J Kidney Dis. 2003;41:550–7.
Rüth EM, Kemper MJ, Leumann EP, Laube GF, Neuhaus TJ. Children with steroid-sensitive nephrotic syndrome come of age: long-term outcome. J Pediatr. 2005;147:202–7.
Trompeter RS, Lloyd BW, Hicks J, White RH, Cameron JS. Long-term outcome for children with minimal-change nephrotic syndrome. Lancet. 1985;1:368–70.
Lewis MA, Baildom EM, Davis N, Houston IB, Postlethwaite RJ. Nephrotic syndrome: From toddlers to twenties. Lancet. 1989;1:255–9.
Schwartz MW, Schwartz GJ, Cornfeld D. A 16 year follow up study of 163 children with nephrotic syndrome. Pediatrics. 1974;54:548–52.
Zidar N, Cavic MA, Kenda RB, Ferluga D. Unfavorable course of minimal change nephrotic syndrome in children with intrauterine growth retardation. Kidney Int. 1998;54:1320–3.
Sheu JN, Jeun-Horng C. Minimal Change Nephrotic Syndrome in Children with Intrauterine Growth Retardation. Am J Kidney Dis. 2001;37:909–14.
Barker DJP, Bull AR, Osmond C, Simmonds SJ. Fetal and placental size and risk of hypertension in adult life. BMJ. 1990;301:259–62.
Barker DJP, Winter PD, Osmond C, Simmons SJ. Weight in infancy and death from ischemic heart disease. Lancet. 1989;2:577–80.
Hales CN, Barker DJP, Clark PMS, Cox LJ, Fall C, Osmond C, Winter PD. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ. 1991;303:1019–22.
Hinchliffe SA, Lynch MR, Sargent PH, Howard CV, Van Velzen D. The effect of intrauterine growth retardation on the development of renal nephrons. Br J Obstet Gynaecol. 1992;99:296–301.
Hughson M, Farris AB 3rd, Douglas-Denton R, Hoy WE, Bertram JF. Glomerular number and size in autopsy kidneys: the relationship to birth weight. Kidney Int. 2003;63:2113–22.
Manalich R, Reyes L, Herrera M, Melendi C, Fundora I. Relationship between weight at birth and the number and size of renal glomeruli in humans: a histomorphometric study. Kidney Int. 2000;58:770–3.
Matsukura H, Inaba S, Shinozaki K, Yanagihara T, Hara M, Higuchi A, Takada T, Tanizawa T, Miyawaki T. Influence of prolonged corticosteroid therapy on the outcome of steroid-responsive nephrotic syndrome. Am J Nephrol. 2001;21:362–7.
Motoyama O, Iitaka K. Final height in children with steroid-sensitive nephrotic syndrome. Pediatrics Int. 2007;49:623–5.
Koskimies O, Vilska J, Rapola J, Hallmann N. Long-term outcome of primary nephrotic syndrome. Arch Dis Child. 1982;57:544–8.
Calderon-Margalit R, Golan E, Twig G, Leiba A, Tzur D, Afek A, et al. History of childhood kidney disease and risk of adult end-stage renal disease. N Engl J Med. 2018;378(5):428–38.
Leonard MB, Feldman HI, Shults J, Zemel BS, Foster BJ, Stallings VA. Long-term, high-dose glucocorticoids and bone mineral content in childhood glucocorticoid sensitive nephrotic syndrome. N Engl J Med. 2004;351:868–75.
Weng FL, Shults J, Herskovitz RM, Zemel BS, Leonard MB. Vitamin D insufficiency in steroid-sensitive nephrotic syndrome in remission. Pediatr Nephrol. 2005;20:56–63.
Truthmann J, Mensink GBM, Bosy-Westphal A, Scheidt-Nave C, Schienkiewitz A. Metabolic Health in Relation to Body Size: Changes in Prevalence over Time between 1997-99 and 2008-11 in Germany. PLoS One. 2016;11(11):e0167159.
Agrawal S, Zaritsky JJ, Fornoni A, Smoyer WE. Dyslipidaemia in nephrotic syndrome: mechanisms and treatment. Nat Rev Nephrol. 2018;14(1):57–70. https://doi.org/10.1038/nrneph.2017.155.
Elmaoğulları S, Tepe D, Uçaktürk SA, Karaca Kara F, Demirel F. Prevalence of dyslipidemia and associated factors in obese children and adolescents. J Clin Res Pediatr Endocrinol. 2015;7(3):228–34.
Korsten-Reck U, Kromeyer-Hauschild K, Korsten K, Baumstark MW, Dickhuth HH, Berg A. Frequency of secondary dyslipidemia in obese children. Vasc Health Risk Manag. 2008;4(5):1089–94.
Mérouani A, Lévy E, Mongeau J-J, Robitaille P, Lambert M, Delvin EE. Hyperlipidemic profiles during remission in childhood idiopathic nephrotic syndrome. Clin Biochem. 2003;36:571–4.
Kniazewska MH, Obuchowics AK, Wielkoszyński T, Zmudzińska-Kitczak J, Urban K, Marek M, Witanowska J, Sieroń-Stołtny K. Atherosclerosis risk factors in young patients formerly treated for idiopathic nephrotic syndrome. Pediatr Nephrol. 2009;24:549–54.
Emma F, Sesto A, Rizzoni G. Long-term linear growth of children with severe steroid responsive nephrotic syndrome. Pediatr Nephrol. 2003;18:783–8.
Foote KD, Brocklebank JT, Meadow SR. Height attainment in children with steroid responsive nephrotic syndrome. Lancet. 1985;2:917–9.
Foster BJ, Shults J, Zemel BS, Leonard MB. Risk factors for glucocorticoid-induced obesity in children with steroid-sensitive nephrotic syndrome. Pediatr Nephrol. 2006;21:973–80.
Salsano ME, Graziano L, Luongo I, Pilla P, Giordano M, Lama G. Atopy in childhood idiopathic nephrotic syndrome. Acta paediatrica. 2007;96:561–6.
Meadow SR, Sarsfield JK, Scott DG, Rajah SM. Steroid-responsive nephrotic syndrome and allergy: immunological studies. Arch Dis Child. 1981;56:517–24.
Hu JF, Liu YZ. Elevated serum IgE levels in children with nephrotic syndrome, a steroid-resistant sign? Nephron. 1990;54:275.
Abdel-Havez M, Shimada M, Lee PY, Johnson RJ, Garin EH. Idiopathic nephrotic syndrome and atopy. Is there a common link? Am J Kidney Dis. 2009;54(5):945–53.
Mundy K, Nichols E, Lindsey J. Socioeconomic disparities in cataract prevalence, characteristics, and management. Semin Ophthalmol. 2016;31(4):358–63.
Brocklebank JT, Harcourt RB, Meadow SR. Corticosteroid-induced cataracts in idiopathic nephrotic syndrome. Arch Dis Childhood. 1982;53:30–4.
Bogdanovic R, Banicevic M, Cvoric A. Testicular function following cyclophosphamide treatment for childhood nephrotic syndrome: long-term follow-up study. Pediatr Nephrol. 1990;4:451–4.
Callis L, Nieto J, Vila A, Rende J. Chlorambucil treatment in minimal lesion nephrotic syndrome: a reappraisal of its gonadal toxicity. J Pediatr. 1980;97:653–6.
Guesry P, Lenoir G, Broyer M. Gonadal effects of chlorambucil given to prepubertal and pubertal boys for nephrotic syndrome. J Pediatr. 1978;92:299–303.
Penso J, Lippe B, Ehrlich R, Smith FG. Testicular function in prepubertal and pubertal male patients treated with cyclophosphamide for nephrotic syndrome. J Pediatr. 1974;84:831–6.
Rapola J, Koskimies O, Huttunen NP, Floman P, Vilska J, Hallmann N. Cyclophoshamide and the pubertal testis. Lancet. 1973;1:98–9.
Basu B, Babu BG, Mahapatra TK. Long-term efficacy and safety of common steroid-sparing agents in idiopathic nephrotic syndrome. Clin Exp Nephrol. 2017;21(1):143–51.
Acknowledgements
***Ingo Franke †*** We thank our first author, colleague, and friend Ingo Franke for his excellent work in the field of Pediatric Nephrology in Germany. He taught us very enthusiastically, and he was a great pediatrician and researcher. Rest in Peace, dear Ingo! This publication should confirm your effort, your invested time, and energy. We all miss you!
Funding
This study was not funded by any private or institutional organizations/firms.
Author information
Authors and Affiliations
Contributions
IF and RH designed and performed the study. MA, MB, LK, RH, and IF performed the literature search, extracted data, and drafted the manuscript. ML and RG participated in manuscript writing and revision. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that they have no competing interests. This work has not been published before and it is not under consideration for publication anywhere else. Its publication has been approved by all co-authors.
Ethics approval and consent to participate
All retrospectively and prospectively analyzed data involving human participants were in accordance with the ethical standards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was obtained by the Ethics Committee of the Faculty of Medicine, Rheinische Friedrich-Wilhelms-University, Bonn, Germany, and the study was assigned the human study registration number 081/05. The data extraction and analyses were performed pseudonymously; an additional participant informed consent was obtained from all individual participants included in the study. This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

About this article
Cite this article
Aydin, M., Franke, I., Kurylowicz, L. et al. The long-term outcome of childhood nephrotic syndrome in Germany: a cross-sectional study. Clin Exp Nephrol 23, 676–688 (2019). https://doi.org/10.1007/s10157-019-01696-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-019-01696-8