Abstract
Background
The accumulation of p-cresol, a metabolic product of aromatic amino acids generated by intestinal microbiome, increases the cardiovascular risk in chronic kidney disease (CKD) patients. Therefore, therapeutic strategies to reduce plasma p-cresol levels are highly demanded. It has been reported that the phosphate binder sevelamer (SEV) sequesters p-cresol in vitro, while in vivo studies on dialysis patients showed controversial results. Aim of our study was to evaluate the effect of SEV on p-cresol levels in non-dialysis CKD patients.
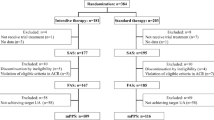
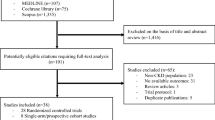
Methods
This was a single-blind, randomized placebo-controlled trial (Registration number NCT02199444) carried on 69 CKD patients (stage 3–5, not on dialysis), randomly assigned (1:1) to receive either SEV or placebo for 3 months. Total p-cresol serum levels were evaluated at baseline (T0), and 1 (T1) and 3 months (T3) after treatment start. The primary end-point was to evaluate the effect of SEV on p-cresol levels.
Results
Compared to baseline (T0, 7.4 ± 2.7 mg/mL), p-cresol mean concentration was significantly reduced in SEV patients after one (− 2.06 mg/mL, 95% CI − 2.62 to − 1.50 mg/mL; p < 0.001) and 3 months of treatment (− 3.97 mg/mL, 95% CI − 4.53 to − 3.41 mg/mL; p < 0.001); no change of plasma p-cresol concentration was recorded in placebo-treated patients. Moreover, P and LDL values were reduced after 3 months of treatment by SEV but not placebo.
Conclusions
In conclusion, our study represents the first evidence that SEV is effective in reducing p-cresol levels in CKD patients in conservative treatment, and confirms its beneficial effects on inflammation and lipid pattern.




Similar content being viewed by others
References
El Nahas AM, Bello AK. Chronic kidney disease: the global challenge. Lancet. 2005;365(9456):331e40.
Kaysen GA. The microinflammatory state in uremia: causes and potential consequences. J Am Soc Nephrol. 2001;12:1549–57.
Cozzolino M, Brancaccio D, Gallieni M, Slatopolsky E. Pathogenesis of vascular calcification in chronic kidney disease. Kidney Int. 2005;68:429–36.
Levin A. Anemia and left ventricular hypertrophy in chronic kidney disease populations: a review of the current state of knowledge. Kidney Int. 2002;61(Suppl. 80):S35–8.
Lee JH, O’Keefe JH, Bell D, Hensrud DD, Holick MF. Vitamin D deficiency, an important, common, and easily treatable cardiovascular risk factor? J Am Coll Cardiol. 2008;52:1949–56.
Cummings JH. Fermentation in the human large intestine: evidence and implications for health. Lancet. 1983;1:1206–9.
Evenepoel P, Meijers BKI, Bammens BRM, Verbeke K. Uremic toxins originating from colonic microbial metabolism. Kidney Int. 2009;76(Suppl 114):S12–9.
Vanholder R, Bammens B, de Loor H, Glorieux G, Meijers B, et al. Warning: the unfortunate end of p-cresol as a uraemic toxin. Nephrol Dial Transplant. 2011;26:1464–7.
Ramezani A, Raj DS. The gut microbiome, kidney disease, and target interventions. J Am Soc Nephrol. 2014;25:657–70.
Lin CJ, Wu CJ, Pan CF, Chen YC, Sun FJ, et al. Serum protein-bound uraemic toxins and clinical outcomes in haemodialysis patients. Nephrol Dial Transplant. 2010;25:3693–700.
Meijers BK, Bammens B, De Moor B, Verbeke K, Vanrenterghem Y, et al. Free p-cresol is associated with cardiovascular disease in hemodialysis patients. Kidney Int. 2008;73:1174–80.
Meijers BK, Claes K, Bammens B, de Loor H, Viaene L, et al. p-cresol and cardiovascular risk in mild-to-moderate kidney disease. Clin J Am Soc Nephrol. 2010;5:1182–9.
Liabeuf S, Barreto DV, Barreto FC, Meert N, Glorieux G, et al. Free pcresylsulphate is a predictor of mortality in patients at different stages of chronic kidney disease. Nephrol Dial Transplant. 2010;25:1183–91.
Cerini C, Dou L, Anfosso F, Sabatier F, Moal V, et al. p-cresol, a uremic retention solute, alters the endothelial barrier function in vitro. Thromb Haemost. 2004;92:140–50.
Meijers BK, Van Kerckhoven S, Verbeke K, Dehaen W, Vanrenterghem Y, et al. The uremic retention solute p-cresyl sulfate and markers of endothelial damage. Am J Kidney Dis. 2009;54:891–901.
Ying Y, Yang K, Liu Y, Chen QJ, Shen WF, et al. A uremic solute, Pcresol, inhibits the proliferation of endothelial progenitor cells via the p38 pathway. Circ J. 2011;75:2252–9.
Davenport A. Role of dialysis technology in the removal of uremic toxins. Hemodial Int. 2011;15:S49–53.
Krieter DH, Hackl A, Rodriguez A, Chenine L, Moragues HL, et al. Protein-bound uraemic toxin removal in haemodialysis and post-dilution haemodiafiltration. Nephrol Dial Transplant. 2010;25:212–8.
Goto S, Yoshiya K, Kita T, Fujii H, Fukagawa M. Uremic toxins and oral adsorbents. Ther Apher Dial. 2011;15:132–4.
Goldsmith DR, Scott LJ, Cvetković RS, Plosker GL. Sevelamer hydrochloride: a review of its use for hyperphosphataemia in patients with end-stage renal disease on haemodialysis. Drugs. 2008;68:85–104.
Evenepoel P, Selgas R, Caputo F, Foggensteiner L, Heaf JG, et al. Efficacy and safety of sevelamer hydrochloride and calcium acetate in patients on peritoneal dialysis. Nephrol Dial Transplant. 2009;24:278–85.
Riccio E, Cataldi M, Minco M, et al. Evidence that p-cresol and IL-6 are adsorbed by the HFR cartridge: towards a new strategy to decrease systemic inflammation in dialyzed patients? PLoS One. 2014;9(4):e95811.
Evenpoel P, Bammens B, Verbeke K, Vanrenterghem Y. Acarbose treatment lowers generation and serum concentration of protein-bound solute p-cresol: a pilot study. Kidney Int. 2006;70:192–8.
Niwa T, Ise M, Miyazaki T, Meada K. Suppressive effect of an oral sorbent on the accumulation of p-cresol in the serum of experimental uremic rats. Nephron. 1993;65:82–7.
De Smet R, Thermote F, Lameire N, Vanholder R. Sevelamer hydrochloride (Renagel) adsorbs the uremic compound indoxyl sulfate, indole and p-cresol. J Am Soc Nephrol. 2004;15:505A.
Brandenburg VM, Schlieper G, Heussen N, Holzmann S, Busch B, et al. Serological cardiovascular and mortality risk predictors in dialysis patients receiving sevelamer: a prospective study. Nephrol Dial Transplant. 2010;25:2672–9.
Guida B, Cataldi M, Riccio E, et al. Plasma p-cresol lowering effect of sevelamer in peritoneal dialysis patients: evidence from a cross-sectional observational study. PLoS One. 2013;8(8):e73558.
Vlassara H, Uribarri J, Cai W, et al. Effects of sevelamer on HbA1c, inflammation, and advanced glycation end products in diabetic kidney disease. Clin J Am Soc Nephrol. 2012;7(6):934–42.
Yuberro-Serrano EM, Woodward M, Poretsky L, et al. Effects of sevelamer carnonate on advanced glycation end products and antioxidant/pro-oxidant status in patients with diabetic kidney disease. Clin J Am Soc Nephrol. 2015;10(5):759–66.
National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42(4, Suppl 3):S1–201.
Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Int Med. 1999;130:461–70.
Maroni BJ, Steinman TI, Mitch WE. A method for estimating nitrogen intake in patients with chronic renal failure. Kidney Int. 1985;27:58–65.
Lin CJ, Chen HH, Pan CF, Chuang CK, Wang TJ, et al. P-cresylsulfate and indoxyl sulfate level at different stages of chronic kidney disease. J Clin Lab Anal. 2011;25:191e7.
Ritz E. Intestinal-renal syndrome: mirage or reality? Blood Purif. 2011;31:70–6.
Bammens B, Evenepoel P, Keuleers H, Verbeke K, Vanrenterghem Y. Free serum concentrations of the protein-bound retention solute p-cresol predict mortality in hemodialysis patients. Kidney Int. 2006;69:1081–7.
Vaziri ND, Wong J, Pahl M, et al. Chronic kidney disease alters intestinal microbial flora. Kidney Int. 2013;83(2):308–15.
Anders HJ, Andersen K, Stecher B. The intestinal microbiota, a leaky gut, and abnormal immunity in kidney disease. Kidney Int. 2013;83(6):1010–6.
Ohno I, Yamaguchi Y, Saikawa H, Uetake D, Hikita M, et al. Sevelamer decreases serum uric acid concentration through adsorption of uric acid in maintenance hemodialysis patients. Int Med. 2009;48:415–20.
Phan O, Ivanovski O, Nguyen-Khoa T, Mothu N, Angulo J, et al. Sevelamer prevents uremia-enhanced atherosclerosis progression in apolipoprotein E-deficient mice. Circulation. 2005;112:2875–82.
American Diabetes Association. Executive summary: standards of medical care in diabetes. Diabetes Care. 2009;32:S13–61.
Evenepoel P, Claus D, Geypens B, Hiele M, Geboes K, et al. Amount and fate of egg protein escaping assimilation in the small intestine of humans. Am J Physiol. 1999;277:G935–43.
Lin CJ, Wu CJ, Pan CF, Chen YC, Sun FJ, et al. Serum concentration of p-cresol and indoxyl sulfate in elderly hemodialysis patients. Int J Geront. 2011;5:80–3.
Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C. Inflammation enhances cardiovascular risk and mortality in hemodialysis patients. Kidney Int. 1999;55:648–58.
Sun W, Liu D, Gong P, et al. Predicting cardiovascular mortality in chronic kidney disease (CKD) patients. Ann Transplant. 2014;19:513–8.
Yamada K, Fujimoto S, Tokura T, et al. Effect of sevelamer on dyslipidemia and chronic inflammation in maintenance hemodialysis patients. Ren Fail. 2005;27(4):361–5.
Chennasamudram SP, Noor T, Vasylyeva TL. Comparison of sevelamer and calcium carbonate on endothelial function and inflammation in patients on peritoneal dialysis. J Ren Care. 2013;39(2):82–9.
Navarro-Gonzalez JF, Mora-Fernandez C, Muros de Fuentes M, Donate-Correa J, Cazaña-Pérez V, et al. Effect of phosphate binders on serum inflammatory profile, soluble CD14, and endotoxin levels in hemodialysis patients. Clin J Am Soc Nephrol. 2011;6:2272–9.
Ferramosca E, Burke S, Chasan-Taber S, Ratti C, Chertow GM, et al. Potential antiatherogenic and anti-inflammatory properties of sevelamer in maintenance hemodialysis patients. Am Heart J. 2005;149:820–5.
Sun PP, Perianayagam MC, Jaber BL. Sevelamer hydrochloride use and endotoxin in hemodialysis patients: a pilot cross-sectional study. J Ren Nutr. 2009;19:432–8.
Stinghen AE, Gonçalves SM, Bucharles S, Branco FS, Gruber B, et al. Sevelamer decreases systemic inflammation in parallel to a reduction in endotoxemia. Blood Purif. 2010;29:352–6.
Levin A, Rigatto C, Barrett B, et al. CanPREDDICT Investigators. Biomarkers of inflammation, fibrosis, cardiac stretch and injury predict death but not renal replacement therapy at 1 year in a Canadian chronic kidney disease cohort. Nephrol Dial Transplant. 2014;29:1037–47.
Burke SK, Dillon MA, Hemken DE, et al. Metaanalysis of the effect of sevelamer on phosphorus, calcium, PTH, and serum lipids in dialysis patients. Adv Ren Replace Ther. 2003;10:133–45.
Imori S, Mori Y, Akita W, et al. Effects of sevelamer hydrochloride on mortality, lipid abnormality and arterial stiffness in hemodialyzed patients: a propensity matched observational study. Clin Exp Nephrol. 2012;16(6):930–7.
Locatelli F, Del Vecchio L. Cardiovascular mortality in chronic kidney disease patients: potential mechanisms and possibilities of inhibition by resin-based phosphate binders. Expert Rev Cardiovasc Ther. 2015;13(5):489–99.
Kalaitzidis RG, Elisaf MS. Hyperphosphatemia and phosphate binders: effectiveness and safety. Curr Med Res Opin. 2014;30(1):109–12.
Frazão JM, Andragão T. Non-calcium-containing phosphate binders: comparing efficacy, safety and other clinical effects. Nephron Clin Pract. 2012;120(2):c108–19.
Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245–52.
Block GA, Spiegel DM, Ehrlich J, et al. Effects of sevelamer and calcium on coronary artery calcification in patients new to hemodialysis. Kidney Int. 2005;68:1815–24.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have declared that no conflict of interest exists.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee at which the studies were conducted (IRB approval number 15/12) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights statement
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
About this article
Cite this article
Riccio, E., Sabbatini, M., Bruzzese, D. et al. Plasma p-cresol lowering effect of sevelamer in non-dialysis CKD patients: evidence from a randomized controlled trial. Clin Exp Nephrol 22, 529–538 (2018). https://doi.org/10.1007/s10157-017-1504-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-017-1504-8