Abstract
Background
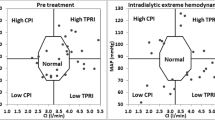
Patients with end-stage renal disease undergoing hemodialysis (HD) have an elevated risk of cardiovascular disease-related morbidity and mortality. To prevent from such a life-threatening event, the continuous blood pressure (BP) monitoring system may contribute to detect BP decline in early stages and may help to do appropriate disposal. Our research team has introduced an electronic stethoscope (Asahi Kasei Co, Ltd., Tokyo, Japan), which translates sound intensity of Arteriovenous Fistula (AVF) to BP data using the technique of Fourier transformation that can predict continuous BP non-invasively. This study, we investigated whether electronic stethoscope-guided estimated BP (e-BP) would actually reflect systolic BP measured by sphygmomanometer (s-BP), and whether e-BP could predict fall of BP during HD.
Methods
Twenty-six patients who underwent HD treatment in our hospital were evaluated prospectively. We obtained sound intensity data from the electronic stethoscope which was equipped with the return line of HD. Then, the data were translated into e-BP data to be compared with s-BP. Correlation of total of 315 data sets obtained from each method was examined. An accuracy of diagnosis of intra-dialytic hypotension (IDH) was evaluated.
Results
Total of 315 data sets were obtained. A close correlation was observed between e-BP and s-BP (r = 0.887, p < 0.0001). Sensitivity and positive predictive value of predicted-BP for detection of IDH was 90 and 81.3%, respectively.
Conclusions
Electronic stethoscope-guided BP measurement would be helpful for real-time diagnosis of BP fall in HD patients. Further investigations are needed.







Similar content being viewed by others
References
Masakane I, Nakai S, Ogata S, Kimata N, Hanafusa N, Hamano T, et al. An overview of regular dialysis treatment in Japan (as of 31 December 2013). Ther Apher Dial. 2015;19:540–74.
Flythe JE, Kimmel SE, Brunelli SM. Rapid fluid removal during dialysis is associated with cardiovascular morbidity and mortality. Kidney Int. 2011;79:250–7.
KDOQI: K/doqi clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis. 2005; 45:S1–S153.
Heinrich WL. Hemodynamic instability during hemodialysis. Kidney Int. 1986;30:605–12.
Bos WJ, Bruin S, van Olden RW, Keur I, Wesseling KH, Westerhof N, et al. Cardiac and hemodynamic effects of hemodialysis and ultrafiltration. Am J Kidney Dis. 2000;35:819–26.
Palmer BF, Henrich WL. Recent advances in the prevention and management of intradialytic hypotension. J Am Soc Nephrol. 2008;19:8–11.
Stefánsson BV, Brunelli SM, Cabrera C, Rosenbaum D, Anum E, Ramakrishnan K, et al. Intradialytic hypotension and risk of cardiovascular disease. Clin J Am Soc Nephrol. 2014;9:2124–32.
Peng RC, Yan WR, Zhang NL, Lin WH, Zhou XL, Zhang YT. Cuffless and continuous blood pressure estimation from the heart sound signals. Sensors (Basel). 2015;15:23653–66.
Owen PJ, Priestman WS, Sigrist MK, Lambie SH, John SG, Chesterton LJ, et al. Myocardial contractile function and intradialytic hypotension. Hemodial Int. 2009;13:293–300.
Mizumasa T, Hirakata H, Yoshimitsu T, Hirakata E, Kubo M, Kashiwagi M, et al. Dialysis-related hypotension as a cause of progressive frontal lobe atrophy in chronic hemodialysis patients: a 3-year prospective study. Nephron Clin Pract. 2004;97:c23–30.
Kersh ES, Kronfield SJ, Unger A, Popper RW, Cantor S, Cohn K. Autonomic insufficiency in uremia as a cause of hemodialysis-induced hypotension. N Engl J Med. 1974;290:650–3.
Poldermans D, Man in ‘t Veld AJ, Rambaldi R, Van Den Meiracker AH, Van Den Dorpel MA, Rocchi G, Boersma E, et al. Cardiac evaluation in hypotension-prone and hypotension-resistant hemodialysis patients. Kidney Int. 1999;56:1905–11.
Kooman JP, Gladziwa U, Böcker G, van Bortel LM, van Hooff JP, Leunissen KM. System in hemodynamics during ultrafiltration and bicarbonate dialysis. Kidney Int. 1992;42:718–26.
Song JH, Park GH, Lee SY, Lee SW, Lee SW, Kim MJ. Effect of sodium balance and the combination of ultrafiltration profile during sodium profiling hemodialysis on the maintenance of the quality of dialysis and sodium and fluid balances. J Am Soc Nephrol. 2005;16:237–46.
Depner TA. Assessing adequacy of hemodialysis: urea modeling. Kidney Int. 1994;45:1522–35.
Sego S. Crit line: instrument to aid fluid removal during hemodialysis. Anna J. 1997;24:347–8.
Hinchliffe RJ, Kirk B, Bhattacharjee D, Roe S, Jeffcoate W, Game F. The effect of haemodialysis on transcutaneous oxygen tension in patients with diabetes-a pilot study. Nephrol Dial Transplant. 2006;21:1981–3.
Agishi T, Sakauchi M, Hoshino T, Akamatsu M, Sato T, Kawashima N. Shift in tissue oxygen pressure possibly preceding abrupt blood pressure drop. Jpn J Clin Dial. 2006;22:573–8.
Munguia M M, Vasquez P, Mattsson E, Mandersson B. Acoustical detection of venous stenosis in hemodialysis patients using principal component analysis. Conf Proc IEEE Eng Med Biol Soc. 2010;3654–7.
Bartels A, Harder D. Noninvasive determination of systolic blood-pressure by heart-sound pattern-analysis. Clin Phys Physiol Meas. 1992;13:249–56.
Acknowledgements
The authors gratefully acknowledge the work of past and present members of our department of our hospital. We also wish to thank the timely technically help given by Elekio, Asahi Kasei Co., Ltd., Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest associated with this manuscript.
Human and animal rights (with IRB approval number)
All procedures performed in studies involving human participants were in accordance with the ethical standards of our institutional research committee at which the studies were conducted (IRB approval number 380) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
About this article
Cite this article
Kamijo, Y., Kanda, E., Horiuchi, H. et al. Continuous monitoring of blood pressure by analyzing the blood flow sound of arteriovenous fistula in hemodialysis patients. Clin Exp Nephrol 22, 677–683 (2018). https://doi.org/10.1007/s10157-017-1499-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-017-1499-1