Abstract
Background
Transanal total mesorectal excision (TaTME) provides an excellent view of the resection margins for rectal cancer from below, but is challenging due to few anatomical landmarks. During implementation of this technique, patient safety and optimal outcomes need to be ensured. The aim of this study was to evaluate the learning curve of TaTME in patients with rectal cancer in order to optimize future training programs.
Methods
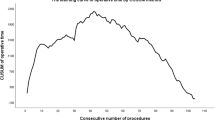
All consecutive patients after TaTME for rectal cancer between February 2012 and January 2017 were included in a single-center database. Influence of surgical experience on major postoperative complications, leakage rate and operating time was evaluated using cumulative sum charts and the splitting model. Correction for potential case-mix differences was performed.
Results
Over a period of 60 months, a total of 138 patients were included in this study. Adjusted for case-mix, improvement in postoperative outcomes was clearly seen after the first 40 patients, showing a decrease in major postoperative complications from 47.5 to 17.5% and leakage rate from 27.5 to 5%. Mean operating time (42 min) and conversion rate (from 10% to zero) was lower after transition to a two-team approach, but neither endpoint decreased with experience. Readmission and reoperation rates were not influenced by surgical experience.
Conclusions
The learning curve of TaTME affected major (surgical) postoperative complications for the first 40 patients. A two-team approach decreased operative time and conversion rate. When implementing this new technique, a thorough teaching and supervisory program is recommended to shorten the learning curve and improve the clinical outcomes of the first patients.


Similar content being viewed by others
References
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
Kapiteijn E, Marijnen CA, Nagtegaal ID et al (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345:638–646
MacFarlane JK, Ryall RD, Heald RJ (1993) Mesorectal excision for rectal cancer. Lancet 341:457–460
Bonjer HJ, Deijen CL, Abis GA et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer (COLOR II trial). N Engl J Med 372:1324–1332
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Green BL, Marshall HC, Collinson F et al (2013) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100:75–82
Van der Pas MHGM, Deijen CL, Abis GA et al (2017) Conversions in laparoscopic surgery for rectal cancer. Surg Endosc 31:2263–2270
Lacy AM, Rattner DW, Adelsdorfer C et al (2013) Transanal natural orifice transluminal endoscopic surgery (NOTES) rectal resection: “down-to up” total mesorectal excision (TME)—short-term outcomes in the first 20 cases. Surg Endosc 27:3165–3172
Lacy AM, Tasende MM, Delgado S et al (2015) Transanal total mesorectal excision for rectal cancer: outcomes after 140 patients. J Am Coll Surg 221:415–423
Veltcamp Helbach M, Deijen CL, Velthuis S et al (2016) Transanal total mesorectal excision for rectal carcinoma: short-term outcomes and experience after 80 cases. Surg Endosc 30(2):464–470
Deijen CL, Tsai A, Koedam TW et al (2016) Clinical outcomes and case volume effect of transanal total mesorectal excision for rectal cancer: a systematic review. Tech Coloproctol 20(12):811–824
Penna M, Hompes R, Arnold S et al (2017) Transanal total mesorectal excision: international registry results of the first 720 cases. Ann Surg 266(1):111–117
Francis N, Penna M, Mackenzie H et al (2017) Consensus on structured training curriculum for transanal total mesorectal excision (TaTME). Surg Endosc 31:2711–2719
Tekkis PP, Senagore AJ, Delaney CP et al (2005) Evaluation of the learning curve in laparoscopic colorectal surgery. Ann Surg 242:83–91
Bege T, Lelong B, Esterni B et al (2010) The learning curve for the laparoscopic approach to conservative mesorectal excision for rectal cancer. Ann Surg 251:249–253
McArdle CS, Hole D (1991) Impact of variability among surgeons on postoperative morbidity and mortality and ultimate survival. BMJ 302:1501–1505
Porter GA, Soskolne CL, Yakimets WW et al (1998) Surgeon-related factors and outcome in rectal cancer. Ann Surg 227:157–167
Martling A, Cedermark B, Johansson H et al (2002) The surgeon as a prognostic factor after the introduction of total mesorectal excision in the treatment of rectal cancer. Br J Surg 89(8):1008–1013
Dutch guidelines rectal carcinoma. Oncoline. http://www.oncoline.nl/index.php?pagina=/richtlijn/item/pagina.php&id=37086&richtlijn_id=933. Accessed 13 July 2017
Arroyave MC, DeLacy FB, Lacy AM (2016) Transanal total mesorectal excision (TaTME) for rectal cancer: step by step description of the surgical technique for a two-teams approach. Eur J Surg Oncol 2:502–505
Nagtegaal I, van de Veld CJH, van der Worp E et al (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20:1729–1734
Rahbari NN, Weitz J, Hohenberger W (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147(3):339–351
Park EJ, Kim CW, Cho MS et al (2014) Is the learning curve of robotic low anterior resection shorter than laparoscopic low anterior resection for rectal cancer? Medicine 93(25):109
Kim CH, Kim HJ, Huh JW et al (2014) Learning curve of laparoscopic low anterior resection in terms of local recurrence. J Surg Oncol 110:989–996
Khan N, Abboudi H, Khan MS et al (2014) Measuring the surgical ‘learning curve’: methods, variables and competency. BJU Int 113:504–508
Chen W, Sailhamer E, Berger DL et al (2007) Operative time is a poor surrogate for the learning curve in laparoscopic colorectal surgery. Surg Endosc 21:238–243
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest, directly related to this study. H.J. Bonjer has received research grants from Applied, Medtronic, Olympus and Ethicon. J.B. Tuynman has received a research grant from the Dutch Cancer Society and speaker honorarium from Applied Medical. C. Sietses received a speaker honorarium from Applied Medical. T.W.A. Koedam, M. Veltcamp Helbach, P.M. van de Ven, Ph.M. Kruyt, and N.T. van Heek have nothing to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Data availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Rights and permissions
About this article
Cite this article
Koedam, T.W.A., Veltcamp Helbach, M., van de Ven, P.M. et al. Transanal total mesorectal excision for rectal cancer: evaluation of the learning curve. Tech Coloproctol 22, 279–287 (2018). https://doi.org/10.1007/s10151-018-1771-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-018-1771-8