Abstract
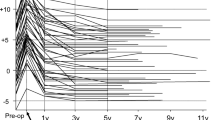
There are many satisfactory long-term outcomes after posterolateral fusion (PLF) for degenerative lumbar spondylolisthesis (DLS); nonunion cases have also achieved good clinical outcomes. Facet fusion (FF), a minimally invasive evolution of PLF, also resulted in good clinical outcomes. We aimed to assess the course of nonunion cases after FF and determine whether the nonunion cases achieved good clinical outcomes. We retrospectively reviewed the records of 136 patients who underwent FF for DLS. Range of motion (ROM) at the fused level was measured using a flexion-extension lateral radiograph preoperatively and 1 year postoperatively. Patients were classified into the Fusion or Unconfirmed Fusion group by computed tomography (CT) 1 year postoperatively. Furthermore, patients in the Unconfirmed Fusion group were classified into the Delayed Union or Nonunion group depending on the confirmation status of FF upon the following CT. The average preoperative ROM and clinical outcomes were compared between the three groups. The Fusion, Delayed Union, and Nonunion groups had 109, 14, and 13 patients, respectively. In the Nonunion group, the average ROM significantly decreased from 13.0° preoperatively to 4.9° postoperatively. There was a significant difference in the average preoperative ROM between the groups. The larger the preoperative ROM, the fewer facets fused. There was no significant difference in clinical outcomes between the groups. Five patients (3.7%) required revision surgery for adjacent segment disease 1–5.5 years after FF. Even nonunion cases after FF achieved good clinical outcomes, likely because the unstable spondylolisthesis was stabilized. FF did not require revision surgery for nonunion itself.






Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Agabegi SS, Majid K, Fischgrund JS, Vaccaro AR, Patel T (2011) Can preoperative radiographic parameters be used to predict fusion in non-instrumented posterolateral fusion for degenerative spondylolisthesis? Spine (Phila Pa 1976) 36(26):E1709–E1714. https://doi.org/10.1097/BRS.0b013e31821d289f
Andersen T, Videbæk TS, Hansen ES, Bünger C, Christensen FB (2008) The positive effect of posterolateral lumbar spinal fusion is preserved at long-term follow-up: a RCT with 11–13 year follow-up. Eur Spine J 17(2):272–280 Epub 2007 Sep 12
Blumenthal C, Curran J, Benzel EC, Potter R, Magge SN, Harrington JF Jr, Coumans JV, Ghogawala Z (2013) Radiographic predictors of delayed instability following decompression without fusion for degenerative grade I lumbar spondylolisthesis. J Neurosurg Spine 18(4):340–346. https://doi.org/10.3171/2013.1.SPINE12537
Challier V, Boissiere L, Obeid I, Vital JM, Castelain JE, Bénard A, Ong N, Ghailane S, Pointillart V, Mazas S, Mariey R, Gille O (2017) One-level lumbar degenerative spondylolisthesis and posterior approach: Is transforaminal lateral interbody fusion mandatory?: a randomized controlled trial with 2-year follow-up. Spine (Phila Pa 1976) 42(8):531–539. https://doi.org/10.1097/BRS.0000000000001857
Chrastil J, Patel AA (2012) Complications associated with posterior and transforaminal lumbar interbody fusion. J Am Acad Orthop Surg 20(5):283–291. https://doi.org/10.5435/JAAOS-20-05-283
Colman MW, Baronne LM 2nd, Brodke DS, Woodbury AM, Annis P, Lawrence BD (2019) Perioperative effects associated with the surgical treatment of degenerative spondylolisthesis: interbody versus no interbody. Clin Spine Surg 32(2):E71–E77. https://doi.org/10.1097/BSD.0000000000000729
Fay LY, Huang WC, Chang CC, Chang HK, Tsai TY, Tu TH, Wu CL, Cheng H, Wu JC (2018) Unintended facet fusions after Dynesys dynamic stabilization in patients with spondylolisthesis. J Neurosurg Spine 30(3):353–361
Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT (1997) Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine (Phila Pa 1976) 22(24):2807–2812
Fukui M, Chiba K, Kawakami M, Kikuchi S, Konno S, Miyamoto M, Seichi A, Shimamura T, Shirado O, Taguchi T, Takahashi K, Takeshita K, Tani T, Toyama Y, Yonenobu K, Wada E, Tanaka T, Hirota Y, Subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation (2009) JOA Back Pain Evaluation Questionnaire (JOABPEQ)/JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ). The report on the development of revised versions April 16, 2007. The Subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation. J Orthop Sci 14(3):348–365. https://doi.org/10.1007/s00776-009-1337-8
Greiner-Perth R, Boehm H, Allam Y, Elsaghir H, Franke J (2004) Reoperation rate after instrumented posterior lumbar interbody fusion: a report on 1680 cases. Spine (Phila Pa 1976) 29(22):2516–2520
Hoppe S, Schwarzenbach O, Aghayev E, Bonel H, Berlemann U (2016) Long-term outcome after monosegmental L4/5 stabilization for degenerative spondylolisthesis with the Dynesys device. Clin Spine Surg 29(2):72–77
Jiang SD, Wu QZ, Lan SH, Dai LY (2012) Reliability of the measurement of thoracolumbar burst fracture kyphosis with Cobb angle, Gardner angle, and sagittal index. Arch Orthop Trauma Surg 132(2):221–225. https://doi.org/10.1007/s00402-011-1394-2 Epub 2011 Sep 13
Kim KT, Lee SH, Lee YH, Bae SC, Suk KS (2006) Clinical outcomes of 3 fusion methods through the posterior approach in the lumbar spine. Spine (Phila Pa 1976) 31(12):1351–1357 discussion 1358
Kornblum MB, Fischgrund JS, Herkowitz HN, Abraham DA, Berkower DL, Ditkoff JS (2004) Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine 29(7):726–733 discussion 733-734
Kuraishi S, Takahashi J, Mukaiyama K, Shimizu M, Ikegami S, Futatsugi T, Hirabayashi H, Ogihara N, Hashidate H, Tateiwa Y, Kinoshita H, Kato H (2016) Comparison of clinical and radiological results of posterolateral fusion and posterior lumbar interbody fusion in the treatment of L4 degenerative lumbar spondylolisthesis. Asian Spine J 10(1):143–152
Kuroki H, Tajima N, Kubo S (2002) Clinical results of posterolateral fusion for degenerative lumbar spinal diseases: a follow-up study of more than 10 years. J Orthop Sci 7(3):317–324
Liu Z, Duan Y, Rong X, Wang B, Chen H, Liu H (2017) Variation of facet joint orientation and tropism in lumbar degenerative spondylolisthesis and disc herniation at L4-L5: a systematic review and meta-analysis. Clin Neurol Neurosurg 161:41–47. https://doi.org/10.1016/j.clineuro.2017.08.005
Lowe TG, Tahernia AD, O'Brien MF, Smith DA (2002) Unilateral transforaminal posterior lumbar interbody fusion (TLIF): indications, technique, and 2-year results. J Spinal Disord Tech 15(1):31–38
Makino T, Kaito T, Fujiwara H, Ishii T, Iwasaki M, Yoshikawa H, Yonenobu K (2014) Does fusion status after posterior lumbar interbody fusion affect patient-based QOL outcomes? An evaluation performed using a patient-based outcome measure. J Orthop Sci 19(5):707–712. https://doi.org/10.1007/s00776-014-0591-6
McAnany SJ, Baird EO, Qureshi SA, Hecht AC, Heller JG, Anderson PA (2016) Posterolateral fusion versus interbody fusion for degenerative spondylolisthesis: a systematic review and meta-analysis. Spine (Phila Pa 1976) 41(23):E1408–E1414
Minamide A, Yoshida M, Simpson AK, Nakagawa Y, Iwasaki H, Tsutsui S, Takami M, Hashizume H, Yukawa Y, Yamada H (2018) Minimally invasive spinal decompression for degenerative lumbar spondylolisthesis and stenosis maintains stability and may avoid the need for fusion. Bone Joint J 100-B(4):499–506. https://doi.org/10.1302/0301-620X.100B4.BJJ-2017-0917.R1
Miyashita T, Ataka H, Kato K, Tanno T (2015) Good clinical outcomes and fusion rate of facet fusion with a percutaneous pedicle screw system for degenerative lumbar spondylolisthesis: minimally invasive evolution of posterolateral fusion. Spine (Phila Pa 1976) 40(9):E552–E557. https://doi.org/10.1097/BRS.0000000000000842
Noshchenko A, Lindley EM, Burger EL, Cain CM, Patel VV (2016) What is the clinical relevance of radiographic nonunion after single-level lumbar interbody arthrodesis in degenerative disc disease?: a meta-analysis of the YODA project database. Spine (Phila Pa 1976) 41(1):9–17. https://doi.org/10.1097/BRS.0000000000001113
Ogura Y, Ogura K, Kobayashi Y, Kitagawa T, Yonezawa Y, Takahashi Y, Yoshida K, Yasuda A, Shinozaki Y, Ogawa J (2020) Minimum clinically important difference of major patient-reported outcome measures in patients undergoing decompression surgery for lumbar spinal stenosis. Clin Neurol Neurosurg 196:105966. https://doi.org/10.1016/j.clineuro.2020.105966
Ohtori S, Suzuki M, Koshi T, Takaso M, Yamashita M, Yamauchi K, Inoue G, Suzuki M, Orita S, Eguchi Y, Ochiai N, Kishida S, Kuniyoshi K, Nakamura J, Aoki Y, Ishikawa T, Arai G, Miyagi M, Kamoda H, Toyone T, Takahashi K (2011) Single-level instrumented posterolateral fusion of the lumbar spine with a local bone graft versus an iliac crest bone graft: a prospective, randomized study with a 2-year follow-up. Eur Spine J 20(4):635–639. https://doi.org/10.1007/s00586-010-1656-7
Park Y, Ha JW, Lee YT, Sung NY (2014) Minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis and degenerative spondylosis: 5-year results. Clin Orthop Relat Res 472(6):1813–1823. https://doi.org/10.1007/s11999-013-3241-y
Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, McGirt MJ (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 14(5):598–604. https://doi.org/10.3171/2010.12.SPINE10472
Potter BK, Freedman BA, Verwiebe EG, Hall JM, Polly DW Jr, Kuklo TR (2005) Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord Tech 18(4):337–346
Santos ER, Goss DG, Morcom RK, Fraser RD (2003) Radiologic assessment of interbody fusion using carbon fiber cages. Spine (Phila Pa 1976) 28(10):997–1001
Simmonds AM, Rampersaud YR, Dvorak MF, Dea N, Melnyk AD, Fisher CG (2015) Defining the inherent stability of degenerative spondylolisthesis: a systematic review. J Neurosurg Spine 23(2):178–189. https://doi.org/10.3171/2014.11.SPINE1426 Epub 2015 May 15
Tokuhashi Y, Ajiro Y, Umezawa N (2008) Follow-up of patients with delayed union after posterior fusion with pedicle screw fixation. Spine (Phila Pa 1976) 33(7):786–791. https://doi.org/10.1097/BRS.0b013e31816956f7
Turunen V, Nyyssönen T, Miettinen H, Airaksinen O, Aalto T, Hakumäki J, Kröger H (2012) Lumbar instrumented posterolateral fusion in spondylolisthetic and failed back patients: a long-term follow-up study spanning 11–13 years. Eur Spine J 21(11):2140–2148. https://doi.org/10.1007/s00586-012-2320-1
Acknowledgments
The authors wish to thank Dr. Takeo Ishii for advice on statistics.
Author information
Authors and Affiliations
Contributions
TM and TT contributed to the study conception and design. Data collection was performed by all the authors. TM conducted the analysis and interpretation of data. The first draft of the manuscript was written by TM, and all the authors commented on previous versions of the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declare that they have no conflicts of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Medical Ethics Committee of our hospital (#25-13).
Informed consent
For this type of study formal consent is not required.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Informed consent for publication was obtained.
Code availability
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyashita, T., Ataka, H., Kato, K. et al. Good clinical outcomes in nonunion cases after facet fusion with a percutaneous pedicle screw system for degenerative lumbar spondylolisthesis. Neurosurg Rev 44, 2847–2855 (2021). https://doi.org/10.1007/s10143-021-01479-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01479-4