Abstract
Purpose
Intragastric free cancer cells in patients with gastric cancer have rarely been studied. The purpose of this study was to investigate the detection rate of intragastric free cancer cells in gastric washes using two types of solutions during endoscopic examination. We further clarified risk factors affecting the presence of exfoliated free cancer cells.
Methods
A total of 175 patients with gastric cancer were enrolled. Lactated Ringer’s solution (N = 89) or distilled water (DW; N = 86) via endoscopic working channel was sprayed onto the tumor surface, and the resultant fluid was collected for cytological examination. We compared the cancer-cell positivity rate between the two (Ringer and DW) groups. We also tested the correlation between cancer-cell positivity and clinicopathological factors in the Ringer group to identify risk factors for the presence of exfoliated cancer cells.
Results
The cancer-cell positivity rate was significantly higher in the Ringer group than that in the DW group (58 vs 6%). Cytomorphology in the Ringer group was well maintained, but not in the DW group. The larger tumor size (≥ 20 mm) and positive lymphatic involvement were significant risk factors of exfoliated free cancer cells.
Conclusions
Cancer cells can be highly exfoliated from the tumor surface into the gastric lumen by endoscopic irrigation in large gastric cancer with lymphatic involvement. Gastric washing by DW can lead to cytoclasis of free cancer cells; therefore, it may minimize the possibility of cancer-cell seeding in procedures carrying potential risks of tumor-cell seeding upon transluminal communication, such as endoscopic full-thickness resection and laparoscopy–endoscopy cooperative surgery.
Similar content being viewed by others
Introduction
Endoscopic full-thickness resection (EFTR) with or without laparoscopic assistance is a potential minimally invasive approach to minimize a resection area according to the lesion size in patients with gastric submucosal tumor and early-stage gastric cancer (EGC) [1, 2]. It may obviate major gastrectomy without compromising curability in selected patients with these tumors. However, there is a major criticism of EFTR, particularly for EGC. During EFTR, an intentional perforation is essential; therefore, free cancer cells in the gastric content may spill into the peritoneal cavity, leading to iatrogenic tumor-cell seeding [1]. However, cytologic evidence of cancer-cell exfoliation from the lesion into the gastric lumen has rarely been studied [3,4,5]. Therefore, we conducted this study to examine the free cancer cells in the stomach having gastric cancer. To this end, we investigated the detection rate of free cancer cells in gastric washes using two types of solution (lactated Ringer’s solution and distilled water, DW) during endoscopic examination. We further clarified risk factors affecting the presence of exfoliated free cancer cells.
Materials and methods
Patients
We studied 175 patients who underwent EGD for preoperative examination of gastric cancer at the Department of Surgery, Kyorin university Hospital between February 2012 and November 2016. The patients were 126 men and 49 women with a mean age of 72 years (range 37–82 years).
All patients underwent either an endoscopic submucosal dissection (ESD; N = 66) or surgical gastrectomy (N = 109). In 131 patients, the maximum depth of tumor invasion remained at the mucosal or submucosal level, and was, therefore, classified as EGC. The remaining 44 patients had advanced gastric cancer with invasion deep into the gastric wall. Clinicopathological parameters of the patients were evaluated in accordance with the Japanese Classification of Gastric Carcinoma established by the Japanese Research Society for Gastric Cancer [6]. Written informed consent was obtained from each patient. This study was approved by the institutional review board of Kyorin University.
Sample collection and cytological examination
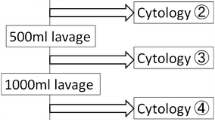
During EGD, intragastric irrigation was performed for improving visibility and diagnosability of gastric cancer. Later, 250 mL of distilled water (DW group; N = 86 in the first-half period of the study) or lactated Ringer’s solution (Ringer group; N = 89 in the second-half period of the study) was sprayed onto the tumor surface through the endoscopic working channel (Fig. 1), the resultant fluid was collected by endoscopic suction. The selection of the solutions was not randomized.
The fluid sample was immediately centrifuged for 5 min at 2000 rpm, and the cell layer was smeared onto a glass slide. The smears were stained with Papanicolaou and Giemsa stains. Normal glandular cells and squamous cells and exfoliated cancer cells were included. Exfoliated cancer cells had irregular nuclei and increased N/C ratio. A well-experienced cytologist assessed the smears, and cytological findings were graded into five classes (classes I to V), of which classes IV and V are defined as cancer-cell positive. The cytologist was blinded on study/clinical information.
We compared the positivity rate of free cancer cells between the Ringer group and the DW group. We also tested the correlation between cancer-cell positivity and clinicopathological factors in the Ringer group to identify risk factors for the presence of exfoliated cancer cells. Multivariate stepwise logistic regression analysis was performed to identify the variables that were considered to affect cancer-cell positivity.
Statistical analyses
Statistical analysis was performed using Fisher’s exact probability test, the Chi-square test, or Student’s t test, where appropriate. Differences were considered significant at P < 0.05.
Results
There were no significant differences in the clinicopathological characteristics between the Ringer and DW groups (Table 1). Side effects due to intragastric irrigation did not occur. On examination of the fluid sample after washing, the cytomorphology of exfoliated cancer cells was well-maintained in the Ringer group (Fig. 2); however, exfoliated cells often showed cytoplasmic swelling and/or bare nucleus and viable cancer cells were rarely observed in the DW group (Fig. 3). In addition, non-viable cells called ghost cells were detected in DW group. Overall, the cancer-cell positivity rate was significantly higher in the Ringer group than that in the DW group (58 vs 6%).
In the Ringer group, the cancer-cell positivity rate in patients with advanced stage was significantly higher than in those with EGC (78 vs 50%). We could not find significant differences in the number and/or size of exfoliated tumor cells between early and advanced gastric cancer. There was no significant difference in the rate according to cancer stage in the DW group (7% for advanced and 0% for early cancer) (Table 2).
Next, in the Ringer group, we analyzed the correlation between cancer-cell positivity rate and various clinicopathological factors listed in Table 3. By univariate analysis, tumor size ≥ 20 mm, deeper invasion to the gastric wall (≥ T2), and positive lymphovascular invasion were significantly associated with a higher detection rate of free cancer cells.
Among these three factors, tumor size and lymphatic invasion were identified as independent predictors for free cancer cells by the multivariate analysis (Table 3). In fact, eight out of the ten (80%) patients with both factors (a tumor size ≥ 20 mm and positive lymphatic invasion) had positive free cancer cells.
Discussion
In this study, we revealed that cancer cells are highly (50% in EGCs and 78% in advanced cancers) exfoliated from the tumor surface into the gastric lumen by endoscopic spraying of lactated Ringer’s solution. The multivariate analysis also revealed that cancer cells of a tumor with a size of ≥ 20 mm and positive lymphatic invasion were easily exfoliated from the primary lesion. It was reported that there was a significant correlation between gastric cancer size and presence/absence of lymphatic invasion. The results in this study may reflect such relationship between tumor size and lymphatic invasion [7]. Han et al. [8] reported cancer cells floating in approximately 15% of resected stomachs with EGCs. A recent study showed that cancer cells in EGCs are easily detached via contact with the tumor surface based on the stamp cytologic examination [3]. These findings support the hypothesis that EFTR as well as laparoscopy and endoscopy cooperative surgery (LECS) [9], which require opening of the stomach during the procedures, may carry a potential risk of peritoneal seeding of cancer cells upon transluminal communication. It is reported that peritoneal dissemination can occur even in differentiated type of early gastric cancer although the incidence of peritoneal dissemination from early gastric cancer is quite low (ranging from 0.4 to 1.2%) [10]. Therefore, EFTR and LECS may not be preferable in treating early gastric cancers with a size of ≥ 20 mm and suspected positive lymphatic invasion irrespective of histological types.
Murata et al. [4] reported that viable cancer cells were highly (23.2%) detected by lavage cytology in the remnant stomach before anastomosis. However, an anastomotic recurrence resulting from the implantation of such viable cancer cells after gastric cancer surgery is extremely rare [11,12,13,14]. Surgeons empirically know these findings and do not routinely perform some preventive procedures against the implantation of free cancer cells, such as gastric irrigation before resection/anastomosis. Theoretically, inadvertent seeding of free cancer cells in the peritoneum could occur after endoscopic resection-related perforation in patients with gastric cancer; however, the endoscopic resection-related perforation does not reportedly lead to peritoneal dissemination, as shown by long-term observation [15].
The presence of intraluminal tumor cells in colorectal cancer patients has been well known [16]. The viability of these exfoliated cancer cells has also been shown. Many studies have indicated the ability of intraluminal tumor cells to implant in colorectal anastomoses. Implantation of intraluminal exfoliated rectal cancer cells is known to be one of the mechanisms of anastomotic recurrence after rectal surgery [17]. Therefore, the routine use of an intraoperative rectal washing before anastomosis has been advised for rectal cancers.
The mechanisms underlying these contrasting findings of colorectal and gastric cancer are unknown. One possible explanation would be the difference in the ability of peritoneal seeding and/or viability of each cancer cell. However, the viability of intragastric exfoliated cancer cells has not been examined and there is no study on the ability of these cells to seed in the peritoneum. Further study will be needed to clarify these issues.
The low cancer-cell positivity rate in the DW group (7% in EGC and 0% in advanced cancer) observed in this study may simply reflect the cytocidal effect of hypotonic stress induced by DW on the free cancer cells. In fact, the cytoplasmic swelling or bareness nucleus (cell rupture) of the cancer cells was observed in the DW group. In contrast, these cytological alterations were not observed in the Ringer group. Ringer’s solution was reportedly less cytopathic and accordingly the most common solution for cytological diagnosis [18].
Experimentally, DW exposure can rapidly increase cancer-cell volume, followed by cell rupture. The cytocidal effect of hypotonic stress on tumor cells has been demonstrated in various malignancies [19, 20]. DW has been shown to be able to induce osmotic lysis in colorectal cancer cells [21, 22], and more effectively kill cells than cytotoxic chemicals via disassociation with the resistant system of cancer cells. Mercill et al. [23] reported that 10 min exposure to DW reduced the number of surviving gastric cancer cells. Intra-abdominal irrigation using DW has been shown to improve the survival rate in patients with ruptured hepatocellular carcinoma [24]. These findings may support the potentially preventive efficacy of pre- and/or intra-procedure gastric irrigation with DW against peritoneal seeding of cancer cells upon transluminal communication during EFTR or LECS for gastric cancer. Gastric irrigation with DW can lead to the cytoclasis of exfoliated free cancer cells; therefore, it may minimize the peritoneal seeding of cancer cells in any type of gastric cancer surgery, which require the opening of the stomach during procedures. In fact, Han et al. [6] indicated that gastric irrigation even with saline solution through a nasogastric tube may prevent or minimize the spillage of gastric cancer cells during gastric cancer surgery.
In conclusion, cancer cells can be highly exfoliated from the tumor surface into the gastric lumen by endoscopic irrigation in large gastric cancer with lymphatic involvement. There still remains an inevitable concern with regard to iatrogenic tumor seeding in EFTR and LECS, which require the opening of the stomach during these procedures, in gastric cancer patients. However, the intraoperative gastric irrigation with DW may minimize the possibility of tumor seeding via cytoclasis of exfoliated free cancer cells.
References
Abe N, Mori T, Takeuchi H, Ueki H, Yanagida O, Masaki T, et al. Successful treatment of early stage gastric cancer by laparoscopy-assisted endoscopic full-thickness resection with lymphadenectomy. Gastrointest Endosc. 2008;68:1220–4.
Nunobe S, Hiki N, Gotoda T, Murao T, Haruma K, Matsumoto H, et al. Successful application of laparoscopic and endoscopic cooperative surgery (LECS) for a lateral-spreading mucosal gastric cancer. Gastric Cancer. 2012;15:338–42.
Goto O, Shimoda M, Sasaki M, Kiguchi Y, Mitsunaga Y, Akimoto T, et al. Potential for peritoneal cancer cell seeding in endoscopic full-thickness resection for early gastric cancer. Gastrointest Endosc. 2017;87(2):450–6.
Murata S, Yamamoto H, Yamaguchi T, Kaida S, Ishida M, Kodama H, et al. Viable cancer cells in the remnant stomach are a potential source of peritoneal metastasis after curative distal gastrectomy for gastric cancer. Ann Surg Oncol. 2016;23:2920–7.
Virgilio E, Giarnieri E, Giovagnoli MR, Montagnini M, Proietti A, D’Urso R, et al. Presence of cancer cells in gastric lavage of gastric cancer patients as an indicator of advanced disease, predictor of tumour aggressive phenotype and independent prognostic factor for poor survival: the endoluminal metastatic pathway of gastric cancer and GL0/GL1 classification. Cytopathology. 2018;29(1):41–8.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric cancer. 2011; 14:101–12.
Sekiguchi M, Sekine S, Oda I, Nonaka S, Suzuki H, Yoshinaga S, et al. Risk factors for lymphatic and venous involvement in endoscopically resected gastric cancer. J Gastroenterol. 2012;48(6):706–12.
Han TS, Kong SH, Lee HJ, Ahn HS, Hur K, Yu J, et al. Dissemination of free cancer cells from the gastric lumen and from perigastric lymphovascular pedicles during radical gastric cancer surgery. Ann Surg Oncol. 2011;18:2818–25.
Hiki N, Yamamoto Y, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, et al. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc. 2008;22:1729–35.
Yamamoto M, Taguchi K, Baba H, Endo K, Kohnoe S, Okamura T, et al. Peritoneal dissemination of early gastric cancer: report of a case. Surg Today. 2006;36(9):835–8.
Polychronidis A, Laftsidis P, Giatromanolaki A, Perente S, Bounovas A, Simopoulos C. Suture-line recurrence at a jejunojejunal anastomosis after gastrectomy for gastric cancer. Gastric Cancer. 2008;11:59–63.
Shinohara TKH, Nakada K, Nimura H, Mitsumori N, Ohmura Y, Yanaga K. Suture line recurrence in the jejunal pouch after curative proximal gastrectomy for gastric cancer: report of two cases. Hepatogastroenterology. 2007;54:1902–4.
Namikawa T, Kobayashi M, Okamoto K, Okabayashi T, Akimori T, Sugimoto T, et al. Recurrence of gastric cancer in the jejunal pouch after completion gastrectomy. Gastric Cancer. 2007;10:256–9.
Nishimura M, Honda I, Watanabe S, Nagata M, Souda H, Miyazaki M. Recurrence in jejunal pouch after proximal gastrectomy for early upper gastric cancer. Gastric Cancer. 2003;6:197–201.
Ikehara H, Gotoda T, Ono H, Oda I, Saito D. Gastric perforation during endoscopic resection for gastric carcinoma and the risk of peritoneal dissemination. Br J Surg. 2007;94:992–5.
Umpleby HC, Williamson RC. The efficacy of agents employed to prevent anastomotic recurrence in colorectal carcinoma. Ann R Coll Surg Engl. 1984;66:192–4.
Matsuda A, Kishi T, Musso G, Matsutani T, Yokoi K, Wang P, et al. The effect of intraoperative rectal washout on local recurrence after rectal cancer surgery: a meta-analysis. Ann Surg Oncol. 2013;20:856–63.
Ohno S, Watanabe Y, Tone K, Tokushige S, Watanabe R, Ito I. Low molecular weight dextran-containing lactate Ringer’s solution as a cytology medium. J Jpn Soc Clinical Cytol. 2009;48(5):274–9.
Iitaka D, Shiozaki A, Ichikawa D, Kosuga T, Komatsu S, Okamoto K, et al. Blockade of chloride ion transport enhances the cytocidal effect of hypotonic solution in gastric cancer cells. J Surg Res. 2012;176:524–34.
Shiozaki A, Ichikawa D, Takemoto K, Nako Y, Nakashima S, Shimizu H, et al. Efficacy of a hypotonic treatment for peritoneal dissemination from gastric cancer cells: an in vivo evaluation. Biomed Res Int. 2014;2014:707089.
Huguet EL, Keeling NJ. Distilled water peritoneal lavage after colorectal cancer surgery. Dis Colon Rectum. 2004;47:2114–9.
Takemoto K, Shiozaki A, Ichikawa D, Komatsu S, Konishi H, Nako Y, et al. Evaluation of the efficacy of peritoneal lavage with distilled water in colorectal cancer surgery: in vitro and in vivo study. J Gastroenterol. 2015;50:287–97.
Mercill DB, Jones NR, Harbell JW. Human tumor cell destruction by distilled water an in Vitro evaluation. Cancer. 1985;55:2779–82.
Lin CH, Hsieh HF, Yu JC, Chen TW, Yu CY, Hsieh CB. Peritoneal lavage with distilled water during liver resection in patients with spontaneously ruptured hepatocellular carcinomas. J Surg Oncol. 2006;94:255–6.
Acknowledgements
The authors would like to thank Ms. Michiru Umino and Ms. Kazumi Ohshima of Kyorin University for excellent help with the cytology of samples.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent to be included in the study was obtained from all patients.
Rights and permissions
About this article
Cite this article
Ohki, A., Abe, N., Yoshimoto, E. et al. Gastric washing by distilled water can reduce free gastric cancer cells exfoliated into the stomach lumen. Gastric Cancer 21, 998–1003 (2018). https://doi.org/10.1007/s10120-018-0824-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-018-0824-z