Abstract
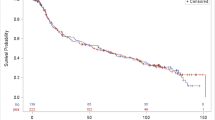
Low-level laser therapy (LLLT) is used in patients with head and neck cancer (HNC) for treatment-related mucositis. There is conflicting evidence as to whether LLLT leads to the proliferation of tumor cells and whether it interferes with the tumoricidal effect of radiotherapy or chemoradiotherapy, if the tumor lies within the LLLT field. Using fuzzy matching, 126 HNC patients who had received LLLT including the tumor region and 126 matching HNC patients without LLLT (controls) treated at the Department of Otorhinolaryngology, Head & Neck Surgery, Medical University of Innsbruck, were identified. The overall survival was compared using the Kaplan–Meier analysis. Fuzzy matching yielded 2 patient samples well comparable in terms of risk of death. The survival did not significantly differ between patients with and without LLLT (p = 0.18). An increased risk of death in HNC patients who received LLLT covering the tumor region was not observed in our study.
Similar content being viewed by others
References
Zecha JA, Raber-Durlacher JE, Nair RG, Epstein JB, Elad S, Hamblin MR, Barasch A, Migliorati CA, Milstein DM, Genot MT, Lansaat L, van der Brink R, Arnabat-Dominguez J, van der Molen L, Jacobi I, van Diessen J, de Lange J, Smeele LE, Schubert MM, Bensadoun RJ (2016) Low-level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: part 2: proposed applications and treatment protocols. Support Care Cancer 24(6):2793–2805. https://doi.org/10.1007/s00520-016-3153-y
Wu S, Zhou F, Wei Y, Chen WR, Chen Q, Xing D (2014) Cancer phototherapy via selective photoinactivation of respiratory chain oxidase to trigger a fatal superoxide anion burst. Antioxid Redox Signal 20(5):733–746. https://doi.org/10.1089/ars.2013.5229
de Freitas LF, Hamblin MR (2016) Proposed mechanisms of photobiomodulation or low-level light therapy. IEEE J Sel Top Quantum Electron 22(3). https://doi.org/10.1109/JSTQE.2016.2561201
Wang X, Tian F, Soni SS, Gonzalez-Lima F, Liu H (2016) Interplay between up-regulation of cytochrome-c-oxidase and hemoglobin oxygenation induced by near-infrared laser. Sci Rep 6:30540. https://doi.org/10.1038/srep30540
Wang X, Tian F, Reddy DD, Nalawade SS, Barrett DW, Gonzalez-Lima F, Liu H (2017) Up-regulation of cerebral cytochrome-c-oxidase and hemodynamics by transcranial infrared laser stimulation: a broadband near-infrared spectroscopy study. J Cereb Blood Flow Metab 37(12):3789–3802. https://doi.org/10.1177/0271678X17691783
Bensadoun RJ (2018) Photobiomodulation or low-level laser therapy in the management of cancer therapy-induced mucositis, dermatitis and lymphedema. Curr Opin Oncol 30(4):226–232. https://doi.org/10.1097/CCO.0000000000000452
Schartinger VH, Galvan O, Riechelmann H, Dudas J (2012) Differential responses of fibroblasts, non-neoplastic epithelial cells, and oral carcinoma cells to low-level laser therapy. Support Care Cancer 20(3):523–529. https://doi.org/10.1007/s00520-011-1113-0
Kreisler M, Christoffers AB, Willershausen B, d’Hoedt B (2003) Low-level 809 nm GaAlAs laser irradiation increases the proliferation rate of human laryngeal carcinoma cells in vitro. Lasers Med Sci 18(2):100–103. https://doi.org/10.1007/s10103-003-0265-7
Gomes Henriques AC, Ginani F, Oliveira RM, Keesen TS, Galvao Barboza CA, Oliveira Rocha HA, de Castro JF, Della Coletta R, de Almeida FR (2014) Low-level laser therapy promotes proliferation and invasion of oral squamous cell carcinoma cells. Lasers Med Sci 29(4):1385–1395. https://doi.org/10.1007/s10103-014-1535-2
de Castro JL, Pinheiro AL, Werneck CE, Soares CP (2005) The effect of laser therapy on the proliferation of oral KB carcinoma cells: an in vitro study. Photomed Laser Surg 23(6):586–589. https://doi.org/10.1089/pho.2005.23.586
Werneck CE, Pinheiro AL, Pacheco MT, Soares CP, de Castro JL (2005) Laser light is capable of inducing proliferation of carcinoma cells in culture: a spectroscopic in vitro study. Photomed Laser Surg 23(3):300–303. https://doi.org/10.1089/pho.2005.23.300
Sonis ST, Hashemi S, Epstein JB, Nair RG, Raber-Durlacher JE (2016) Could the biological robustness of low level laser therapy (photobiomodulation) impact its use in the management of mucositis in head and neck cancer patients. Oral Oncol 54:7–14. https://doi.org/10.1016/j.oraloncology.2016.01.005
Zecha JA, Raber-Durlacher JE, Nair RG, Epstein JB, Sonis ST, Elad S, Hamblin MR, Barasch A, Migliorati CA, Milstein DM, Genot MT, Lansaat L, van der Brink R, Arnabat-Dominguez J, van der Molen L, Jacobi I, van Diessen J, de Lange J, Smeele LE, Schubert MM, Bensadoun RJ (2016) Low level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: part 1: mechanisms of action, dosimetric, and safety considerations. Support Care Cancer 24(6):2781–2792. https://doi.org/10.1007/s00520-016-3152-z
Sperandio FF, Giudice FS, Correa L, Pinto DS Jr, Hamblin MR, de Sousa SC (2013) Low-level laser therapy can produce increased aggressiveness of dysplastic and oral cancer cell lines by modulation of Akt/mTOR signaling pathway. J Biophotonics 6(10):839–847. https://doi.org/10.1002/jbio.201300015
Crous A, Abrahamse H (2016) Low-intensity laser irradiation at 636 nm induces increased viability and proliferation in isolated lung cancer stem cells. Photomed Laser Surg 34(11):525–532. https://doi.org/10.1089/pho.2015.3979
Rhee YH, Moon JH, Choi SH, Ahn JC (2016) Low-level laser therapy promoted aggressive proliferation and angiogenesis through decreasing of transforming growth factor-beta1 and increasing of Akt/hypoxia inducible factor-1alpha in anaplastic thyroid cancer. Photomed Laser Surg 34(6):229–235. https://doi.org/10.1089/pho.2015.3968
Bamps M, Dok R, Nuyts S (2018) Low-level laser therapy stimulates proliferation in head and neck squamous cell carcinoma cells. Front Oncol 8:343. https://doi.org/10.3389/fonc.2018.00343
Austin PC, Stuart EA (2015) Optimal full matching for survival outcomes: a method that merits more widespread use. Stat Med 34(30):3949–3967. https://doi.org/10.1002/sim.6602
Riechelmann H, Neagos A, Netzer-Yilmaz U, Gronau S, Scheithauer M, Rockemann MG (2006) The ASA-score as a comorbidity index in patients with cancer of the oral cavity and oropharynx. Laryngo- rhino- otologie 85(2):99–104. https://doi.org/10.1055/s-2005-870291
Smith AH, Bates MN (1992) Confidence limit analyses should replace power calculations in the interpretation of epidemiologic studies. Epidemiology 3(5):449–452. https://doi.org/10.1097/00001648-199209000-00011
Schemper M, Smith TL (1996) A note on quantifying follow-up in studies of failure time. Control Clin Trials 17(4):343–346
Oberoi S, Zamperlini-Netto G, Beyene J, Treister NS, Sung L (2014) Effect of prophylactic low level laser therapy on oral mucositis: a systematic review and meta-analysis. PLoS One 9 (9):e107418. doi:https://doi.org/10.1371/journal.pone.0107418
Simpson MC, Challapalli SD, Cass LM, Zahirsha ZS, Adjei Boakye E, Massa ST, Osazuwa-Peters N (2019) Impact of gender on the association between marital status and head and neck cancer outcomes. Oral Oncol 89:48–55. https://doi.org/10.1016/j.oraloncology.2018.12.009
Schlichting JA, Pagedar NA, Chioreso C, Lynch CF, Charlton ME (2019) Treatment trends in head and neck cancer: Surveillance, Epidemiology, and End Results (SEER) patterns of care analysis. Cancer Causes Control 30(7):721–732. https://doi.org/10.1007/s10552-019-01185-z
Antunes HS, Herchenhorn D, Small IA, Araujo CMM, Viegas CMP, de Assis RG, Dias FL, Ferreira CG (2017) Long-term survival of a randomized phase III trial of head and neck cancer patients receiving concurrent chemoradiation therapy with or without low-level laser therapy (LLLT) to prevent oral mucositis. Oral Oncol 71:11–15. https://doi.org/10.1016/j.oraloncology.2017.05.018
Oton-Leite AF, Elias LS, Morais MO, Pinezi JC, Leles CR, Silva MA, Mendonca EF (2013) Effect of low level laser therapy in the reduction of oral complications in patients with cancer of the head and neck submitted to radiotherapy. Spec Care Dentist 33(6):294–300. https://doi.org/10.1111/j.1754-4505.2012.00303.x
de Lima VHS, de Oliveira-Neto OB, da Hora Sales PH, da Silva TT, de Lima FJC (2020) Effectiveness of low-level laser therapy for oral mucositis prevention in patients undergoing chemoradiotherapy for the treatment of head and neck cancer: a systematic review and meta-analysis. Oral Oncol 102:104524. https://doi.org/10.1016/j.oraloncology.2019.104524
Basso FG, Soares DG, Pansani TN, Cardoso LM, Scheffel DL, de Souza Costa CA, Hebling J (2016) Proliferation, migration, and expression of oral-mucosal-healing-related genes by oral fibroblasts receiving low-level laser therapy after inflammatory cytokines challenge. Lasers Surg Med 48(10):1006–1014. https://doi.org/10.1002/lsm.22553
Silva GB, Sacono NT, Othon-Leite AF, Mendonca EF, Arantes AM, Bariani C, Duarte LG, Abreu MH, Queiroz-Junior CM, Silva TA, Batista AC (2015) Effect of low-level laser therapy on inflammatory mediator release during chemotherapy-induced oral mucositis: a randomized preliminary study. Lasers Med Sci 30(1):117–126. https://doi.org/10.1007/s10103-014-1624-2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
This paper fulfills the ethical criteria of Lasers in Medical Science.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This is an original work, not submitted elsewhere.
Rights and permissions
About this article
Cite this article
Fischlechner, R., Kofler, B., Schartinger, V. et al. Does low-level laser therapy affect the survival of patients with head and neck cancer?. Lasers Med Sci 36, 599–604 (2021). https://doi.org/10.1007/s10103-020-03073-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03073-4