Abstract
To determine the combined therapeutic effect of fractional carbon dioxide laser and silicone gel on fresh traumatic scars using a rabbit ear hypertrophic scar (EHS) model, as well as on human subjects. The rabbit EHS model was established by punching four circular wounds in each ear and respectively treated with carbon dioxide laser, silicone gel, and the combination of both, while one wound was left untreated. In addition, a validation group of five rabbits was also included wherein the wounds were treated with triamcinolone, IFN-α, and normal saline, with one untreated control. The gross hyperplasic changes and the histological features were analyzed, and the scar elevation index (SEI) was calculated for each treatment group. In the rabbit model, the untreated control wounds showed hypertrophic growth, whereas triamcinolone or IFN-α showed an inhibitory effect, similar to that on hypertrophic scars in humans, thereby proving the feasibility of our animal model. The SEI peaked 2 months after treatment and was respectively 2.28 ± 0.56, 1.85 ± 0.33, 1.91 ± 0.34, and 1.45 ± 0.22 in the untreated control, and the silicone, laser, and combined treatment groups, clearly indicating a significant therapeutic effect of the combined treatment modality (p < 0.01). The fibroblast and microvascular counts also showed similar trends in each group. Early application of fractional carbon dioxide laser can prevent hypertrophic scars; the combined use of laser and silicone gel was more effective with less recovery time, thereby worthy of clinical promotion.
Similar content being viewed by others
Introduction
Scar formation is a normal physiological response to tissue trauma or injury and is seen on the skin, as well in the gastrointestinal tract and other visceral organs. However, surface scarring on the face and limbs often has physiological and psychological effects on the patients. Efforts have been made since the past decades to promote rapid and effective wound healing while reducing hyperplasia and scar formation. Traditional scar removal methods include the non-surgical treatments such as pressurization, drug, laser, radiotherapy, and chemotherapy, as well as surgical resection. Although these methods usually show satisfactory results, they are unable to meet the modern patient’s need to improve his/her appearance, in keeping with the improvements in living standards and the evolving esthetic concepts. Therefore, novel and more effective scar removal methods are urgently sought by dermatologists and esthetic surgeons. The non-invasive silicone gel has always been the first choice among the traditional methods and mainly used as a preventive measure in the early stages of scar hyperplasia. It is painless and convenient, and therefore highly popular among the patients. Laser is often used in the late stage of scar hyperplasia, but since its efficacy is offset by the pain and risk of infection, both clinicians and patients rarely select this option. In recent years, however, more clinicians have begun to use laser for the early preventive treatment of scars and achieved good results. Since its first published report in 2003, fractional photothermolysis (FP) has been increasingly used for various skin diseases, such as acne, pigmentation, and scarring [1,2,3]. Its unique penetration mechanism allows it to be used in combination with other drugs to treat scarring with the effect of “1 + 1 > 2”. In a recent study, carbon dioxide fractional laser was combined with 5-fluorouracil (5-FU) and the thermal decomposition effect of the former helped penetrate the pore channels of deep scar tissue, thereby improving the permeability and dispersion rate of 5-FU and achieving good therapeutic effect [4]. The possible mechanisms underlying the anti-scarring effects of silicone include hydration, electrostatic effect, and fibroblast inhibition. The aim of this study was to compare the effects of carbon dioxide fractional laser either alone or in combination with silicone gel for the early preventive scar treatment in animal models.
Methods
Rabbit ear hyperplasia scar (EHS) model establishment
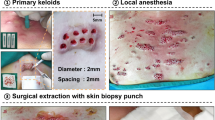
Thirty male adult New Zealand white rabbits weighing between 2.5 and 3 kg were obtained from the Anhui Medical University Laboratory Animal Center. After iodophor disinfection, the rabbit ears were locally anesthetized with 2% lidocaine plus 1:200,000 diluted epinephrine. Four circular wounds of 1-cm diameter and spaced 1 cm apart were punched on the ventral surface of each ear. An operating loupe was used to ensure removal of the epidermis, dermis, and perichondrium in each wound (Fig. 1), and hemostasis was achieved by applying pressure with cotton balls. A total of 240 wounds were created and disinfected every 2 days. After 7–10 days, the scab on the wound surface fell off naturally, forming fresh hypertrophic scars.
ES treatment regimen
The 30 rabbits were first randomized into the experimental (n = 25, 50 ears) and the validation (n = 5) groups. In the experimental group, one wound per ear was untreated (control), and the remaining three wounds were randomly treated as follows: (1) silicone gel—the appropriate size of the gel (Wanmei, Shanghai Winner Plastic Surgery Products) was cut to completely cover the scars for 6 months and was replaced every 3 days; (2) carbon dioxide fractional laser—the wounds were treated with three pulses of the laser once a month (wavelength 10,600 nm, energy 80 MJ/MTZ, spot size 2 mm, density 25%, round scan area, and pulse duration 1 ms)(carbon dioxide laser device of KL type, Kinglaser, China), and the wounds were then swabbed with iodide to prevent infection; (3) laser and gel combination—the wounds of the right ear were pulsed thrice with the carbon dioxide fractional laser once a month and covered with the silicone gel for the remainder of the duration. The four wounds of each ear of the validation group rabbits (40 wounds in total) were treated as follows: (1) 0.25 ml triamcinolone acetonide (5 mg/kg), (2) 0.25 ml IFN-α (500 U/ml), (3) 0.25 ml normal saline, and (4) untreated control. The respective drugs were intra-dermally injected once a month for 3 months. The scars of both groups were photographed and excised on 1, 2, 3, 4, and 5 months after starting the different treatment modalities. In the experimental group, we randomly grabbed five rabbits every time and excised a total of 40 scars from them. The removed tissues included the whole scarred layer, the lower part of the cartilage layer, and some surrounding normal tissue. Each scar tissue sample was fixed in 4% neutral buffered formaldehyde, dehydrated, embedded in paraffin, cut into 4-mm sections, and stained with hematoxylin and eosin (H&E) according to standard protocols.
Tissue repair indicators
Gross observation
The wounds were visually examined for external signs of healing, color change, softening, and flattening time of the hypertrophic scars. The degree of dermal hypertrophy was measured in terms of the scar elevation index (SEI), which is defined as the ratio of the area of newly formed dermis of the scar to the area of the surrounding normal dermis (Fig.2). An SEI value greater than 1 indicates a hypertrophic dermis. The SEIs were measured twice by a blinded examiner, and the average of the two values was calculated.
Histological examination
The morphology and density of fibroblasts, arrangement of collagen fibers, and hyperplasia of the capillaries in the scar tissues were examined at different stages by two pathologists blinded to the experimental grouping. The number of fibroblasts was counted in three randomly chosen fields of 1-mm2 area per sample at × 400 magnification, and the capillaries were counted per field under × 100 magnification. The fibroblastic density (FD) and capillary density (CD) were accordingly calculated.
Statistical analysis
SPSS Version 19.0 for Windows was used for all statistical analyses. The variables were expressed as the medians and ranges, and the four treatment groups were compared using the Kruskal-Wallis test and post hoc Wilcoxon rank sum test. A p value < 0.05 was considered statistical significance.
Results
Gross observations in the rabbit EHS model
No rabbits died during the experimental period. The overall healing time of the ventral ear wound was 12 to 14 days in all the treated rabbits. After the scab on the wound surface fell off, the center rose like a nipple and the base was reddish and pliable. In the untreated control, the thickness of the wound was twice as that of the full thickness of the skin 30 days after molding. Some hyperplasic tissues stopped growing and began to soften starting 60 days after modeling. However, more than half of the hyperplasic scars remained and the longest hyperplasia period lasted for 100 days. In the treated animals, the hyperplasic area stopped growing after 2 weeks to 1 month of treatment and the texture began to soften and the color started fading. In addition, the scars flattened completely within 10 weeks of treatment. In the validation group, the growth of the untreated and the saline-injected scar tissues were similar and significantly inhibited following triamcinolone or IFN-α treatment (Fig. 3).
Histopathological evaluation of the EHS tissues
The normal skin structure of rabbit ears is similar to that of humans, with neatly arranged fibroblasts and microvessels clearly visible after H&E staining. After 7 days of HS modeling, the fibroblasts in the untreated control began to proliferate and the microvascular diameter increased considerably, and 1 month later, the fibroblasts, blood vessels, and collagen fibers were completely disordered. The scar tissues in each treatment group showed fibroblast and vascular hyperplasia of varying degrees within the first 3 months after treatment but were lower than those in the control group. The degree of hyperplasia in the silicone and laser-treated groups were similar, and that of the combination group was minimal (Fig. 4). The SEI peaked 2 months after treatment and was 2.28 ± 0.56, 1.85 ± 0.33, 1.91 ± 0.34, and 1.45 ± 0.22 in the control, silicone, laser, and combined treated groups, respectively. Although the SEI of each group decreased over time, it was fastest in the combined group and similar between the silicone and laser-treated groups (Fig. 5; p < 0.05). The fibroblasts and microvascular counts also followed similar trends (Figs. 6 and 7).
Discussion
Surgical suturing has become increasingly sophisticated, and with the improvement in the patients’ awareness of post-operative care, the frequency of scar formation in trauma patients has lessened. However, the incidence of post-traumatic scars is still high in the Asian skin type due to various reasons [5] and with more specific requirements of the patients in terms of appearance, the prevention and treatment of post-operative scars is receiving more attention from esthetic surgeons. The main methods include silicone gel, steroid hormones, calcium blockers, radiotherapy, laser, and surgical excision. Scar formation is a complex process, and the aforementioned treatments are mainly targeted at the mature stage of scar formation.
Fractional laser has gained popularity in recent years for the “stubborn scars”. It causes selective thermal damage to various water-containing structures [6] and can inhibit the proliferation of skin fibroblasts by regulating growth factors such as TGF-β, MMPs, and HSPs, thereby reducing the collagen deposition [7,8,9]. The theory of fractional photothermolysis (FP) was first proposed in 2003 [1] and first tested successfully by Manstein et al. in 2004 to treat skin wrinkles in the forearm and orbit [2]. FP forms microscopic thermal zones (MTZ) on the skin, and the normal tissue in the intact region is able to repair the epidermis rapidly through keratinocyte migration and extrusion of damaged epidermal components to the border of the column of thermal damage [3]. Since it does not have the full coverage of traditional laser, FP can reduce the pain during treatment and shorten the time needed for tissue repair.
Hypertrophic scars form when the skin trauma reaches the dermis, and a simple wound can lead to hypertrophic scars or keloid due to factors such as race, age, location, and infection. Wound healing is divided into three overlapping phases: inflammation phase, proliferation with the formation of granulation tissue, and the maturation phase constituting remodeling [10, 11]. The capillaries and fibroblasts are instrumental to massive collagen deposition during wound healing, and disordered decomposition and synthesis of collagen fibers in the proliferation phase is the main pathological process of scar formation. Thus, modulating this phase could minimize scar tissue formation. Laser exposure within 3 months after wounding targets the early wound healing process and upregulates HSP47, HSP70, and HSP72 expression within the first hour following AFP, peaking 3–14 days post-intervention [12]. Hantash et al. detected increased levels of HSP47 7 days post-treatment, which persisted over 3 months [13]. In contrast, TGF-β expression was weak at all time points but highest in the spino-cellular layer 1 h to 3 days post-intervention with steadily declining levels over 14 days. These changes promote fibroblast chemotaxis to the extracellular matrix (ECM) to form collagen, resulting in dermal remodeling or scar formation [14, 15]. In our animal model, the capillaries and fibroblasts proliferated rapidly till 3 months post-treatment, especially during the first month. Since collagen fibers emerge at the end of the proliferation phase of wound healing, it is reasonable to start the laser treatment during the inflammation or the proliferation phase in order to regulate the distribution of collagen fibers. Histologically, increased capillary and fibroblast counts at 3 months post-treatment, especially the first month, were significantly lower than those in the control group, which also confirmed the feasibility of early intervention.
Silicone gel dressing has been used as an early preventive scar treatment since more than three decades and showed visible effects both in the rabbit EHS model in our study. In the early stages of wound healing, significant inhibition of fibroblasts and capillaries was seen after silicone coating of the wounds compared to the control group. When used in combination with laser, its therapeutic effects were further enhanced. The possible mechanisms of silicone gel action include closed hydration, oxygen tension, and electrostatic effect [16,17,18,19], which inhibit fibroblast proliferation and VEGF expression, although the specific pathway is not clear. Some researchers proposed the pressure and silicone osmosis hypothesis, which was however rejected by subsequent experiments [20, 21].
Our hypothesis is that when used in combination, FP opens the channels of the corneum and epithelium, and enhances the permeation and retention of the silicone gel, thus enhancing its therapeutic effect. The MTZs extend from the epidermis into the dermis to varying depths, which is determined by the energy of the pulse and the spot size [2]. Thermal damage induced by the MTZs occurs at the depth of up to 1600 μm in the dermis. Despite this, re-epithelialization can occur within a day after treatment [2, 22], which reduces infection and other risks. The wavelength of carbon dioxide lasers has a much lower absorption coefficient for water, which results in significant collateral thermal injury such as charring and scar formation but also improves hemostasis [23]. The energy of the laser was controlled in our study, and the minimum energy and density were selected. In addition, although FP can be used safely and effectively in Asian skin types (IV, V, VI), due to its long wavelength and low absorption rate of melanin, hypopigmentation cannot be ignored in future clinical trial.
Conclusion
Early application of fractional carbon dioxide laser can prevent hypertrophic scars, although the type of laser, the exact time point of early application, and the frequency and duration of laser need to be further validated.
The combined use of laser and silicone gel was more effective with less side effects, thereby worthy of clinical promotion. Further studies are needed to explore the underlying mechanisms of their therapeutic effects.
References
Huzaira M, Anderson RR, Sink K, Manstein D (2003) Intradermal focusing of near-infrared optical pulses: a new approach for non-ablative laser therapy. Lasers Surg Med 32(Suppl 15):17–38
Manstein D, Herron GS, Sink RK et al (2004) Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med 34:426–438
Tierney EP, Kouba DJ (2009) Review of fractional photothermolysis: treatment indications and efficacy. Dermatol Surg 35(10):1445–1461
Zhang Z, Chen J, Huang J et al (2018) Experimental study of 5-fluorouracil encapsulated ethosomes combined with CO2 fractional laser to treat hypertrophic scar. Nanoscale Res Lett 13(1):26
Visscher MO, Bailey JK (2014) Scar treatment variations by skin type. Facial Plast Surg Clin North Am 22(3):453–462. https://doi.org/10.1016/j.fsc.2014.04.010
Khan MH, Sink RK, Manstein D et al (2005) Intradermally focused infrared laser pulses: thermal effects at defined tissue depths. Lasers Surg Med 36(4):270–280
Singer AJ, Clark RA (1999) Cutaneous wound healing. N Engl J Med 341(10):738–746
Vidal Magalhaes W, Gouveia Nogueira MF, Kaneko TM (2012) Heat shock proteins (HSP): dermatological implications and perspectives. Eur J Dermatol 22(1):8–13
Baum CL, Arpey CJ (2005) Normal cutaneous wound healing: clinical correlation with cellular and molecular events. Dermatol Surg 31(6):674–686
Karmisholt KE, Haerskjold A, Karlsmark T et al (2018) Early laser intervention to reduce scar formation - a systematic review. J Eur Acad Dermatol Venereol. (JEADV) 32(7):1099–1110. https://doi.org/10.1111/jdv.14856
Profyris C, Tziotzios C, Do Vale I (2012) Cutaneous scarring: pathophysiology, molecular mechanisms, and scar reduction therapeutics part I. The molecular basis of scar formation. J Am Acad Dermatol 66(1):1–10
Helbig D, Bodendorf MO, Grunewald S et al (2009) Immunohistochemical investigation of wound healing in response to fractional photothermolysis. J Biomed Optics 14(6):064044
Hantash BM, Bedi VP, Kapadia B et al (2007) In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med 39(2):96–107
Shi Y (2003) Mechanisms of TGF-beta signaling from cell membrane to the nucleus. Cell 113(6):685–700
Vaughan MB, Howard EW (2000) Transforming growth factor-beta1 promotes the morphological and functional differentiation of the myofibroblast. Expt Cell Res 257(1):180–189. https://doi.org/10.1006/excr.2000.4869
Hanasono MM, Lum J, Carroll LA et al (2004) The effect of silicone gel on basic fibroblast growth factor levels in fibroblast cell culture. Arch Fac Plast Surg 6(2):88–93
Tandara AA (2008) The role of the epidermis in the control of scarring: evidence for mechanism of action for silicone gel. J Plas Recon Aesth Surg (JPRAS) 61(10):1219–1225
Gilman TH (2003) Silicone sheet for treatment and prevention of hypertrophic scar: a new proposal for the mechanism of efficacy. Wound Repair Regen 11(3):235–236
Van den Kerckhove E, Stappaes K, Boeckx W et al (2001) Silicones in the rehabilitation of burns: a review and overview. Burns 27(3):205–214
Amicucci G, Scbietroma M, Rossi M et al (2005) Silicone occlusive sheeting vs silicone cushion for the treatment of hypertrophic and keloid scars. A prospective randomized study. Ann Ital Chir 76(1):79–83
Wong TW, Chiu HC, Chang CH et al (1996) Silicone cream occlusive dressing - a novel noninvasive regimen in the treatment of keloid. Dermatology 192(4):329–333
Laubach H, Chan HH, Rius F et al (2006) Skin responses to fractional photothermolysis. Lasers Surg Med 38:142–149
Alexiades-Armenakas MR, Dover JS (2012) Fractional laser skin resurfacing. J Drugs Dermatol. (JDD) 11(11):1274–1287
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Yang, Z., Lv, Y., Yue, F. et al. Early intervention of fractional carbon dioxide laser on fresh traumatic scar. Lasers Med Sci 34, 1317–1324 (2019). https://doi.org/10.1007/s10103-019-02716-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-019-02716-5