Abstract
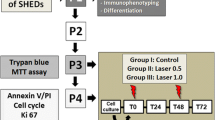
The aim of this preliminary study was to compare the effects of different energy densities from red and infrared low-level laser (LLL) on viability and proliferation of stem cells from human exfoliated deciduous teeth (SHED). SHED were irradiated with red laser (R) or infrared laser (IR) set with the following dosimetry: 1.2 J/cm2 (0.05 J), 2.5 J/cm2 (0.1 J), 5.0 J/cm2 (0.2 J), and 7.5 J/cm2 (0.3 J). Positive (C+) and negative (C−) control groups comprised non-irradiated cells. Data were analyzed by two-way ANOVA followed by Tukey’s test (P < 0.05). At 24- and 48-h period, group R5.0 showed significantly higher cell viability rates than R1.2 and R2.5. At 48 h, R2.5 also revealed lower proliferation than R5.0. Comparing to the C+ group, R2.5 exhibited lower viability at 72 h, and proliferation at 24 and 48 h. Groups R1.2, IR1.2, and IR5.0 were less viable at 24 h, while R1.2, IR2.5, and IR5.0 revealed lower proliferative capacity at 48 h. Overall, our results showed that LLL can favor viability and proliferation of SHED, especially when cells receive red laser irradiation at 5.0 J/cm2. Therefore, according to this preliminary investigation, 5 J/cm2 applied by red LLL induced high rates of cell viability and proliferation, while the same irradiation dose using infrared laser led to negative effects. LLL irradiation with 1.2 and 2.5 J/cm2 was deleterious to metabolic activity and proliferation of SHED regardless of the type of laser. Further studies are necessary to gain in-depth knowledge about the effects of different wavelengths of LLL on SHED viability and proliferation.



Similar content being viewed by others
References
Edwards PC, Mason JM (2006) Gene-enhanced tissue engineering for dental hard tissue regeneration: (2) dentin-pulp and periodontal regeneration. Head Face Med 2:16. https://doi.org/10.1186/1746-160X-2-16
Miura M, Gronthos S, Zhao M, Lu B, Fisher LW, Robey PG, Shi S (2003) SHED: stem cells from human exfoliated deciduous teeth. Proc Natl Acad Sci U S A 100:5807–5812
Nör JE (2006) Tooth regeneration in operative dentistry. Oper Dent 31:633–642
Cordeiro MM, Dong Z, Kaneko T, Zhang Z, Miyazawa M, Shi S, Nör JE (2008) Dental pulp tissue engineering with stem cells from exfoliated deciduous teeth. J Endod 34:962–969
Sakai VT, Zhang Z, Dong Z, Neiva KG, Machado MAAM, Shi S, Nör JE (2010) SHED differentiate into functional odontoblasts and endothelium. J Dent Res 89:791–796. https://doi.org/10.1177/0022034510368647
Telles PD, Machado MADAM, Sakai VT, Nör JE (2011) Pulp tissue from primary teeth: new source of stem cells. J Appl Oral Sci 19:89–194
Sakai VT, Cordeiro MM, Dong Z, Zhang Z, Zeitlin BD, Nör JE (2011) Tooth slice/scaffold model of dental pulp tissue engineering. Adv Dent Res 23:325–332. https://doi.org/10.1177/0022034511405325
Kerkis I, Caplan AI (2011) Stem cells in dental pulp of deciduous teeth. Tissue Eng Rev 18:129–138
Arora V, Arora P, Munshi AK (2009) Banking stem cells from human exfoliated deciduous teeth (SHED): saving for the future. J Clin Pediatr Dent 33:289–294
Oliveira TM, Moretti ABS, Sakai VT, Neto NL, Santos CFD, Machado MADAM, Abdo RCC (2013) Clinical, radiographic and histologic analysis of the effects of pulp capping materials used in pulpotomies of human primary teeth. Eur Arch Paediatr Dent 14:65–71. https://doi.org/10.1007/s40368-013-0015-x
Marques NCT, Neto NL, de Oliveira Rodini C, Fernandes AP, Sakai VT, Machado MAAM, Oliveira TM (2015) Low-level laser therapy as an alternative for pulpotomy in human primary teeth. Lasers Med Sci 30:1815–1822. https://doi.org/10.1007/s10103-014-1656-1657
Karu TI (1989) Photobiology of low-power laser effects. Health Phys 56:691–704
Almeida-Lopes L, Rigau J, Amaro Zângaro R, Guidugli-Neto J, Marques Jaeger MM (2001) Comparison of the low level laser therapy effects on cultured human gingival fibroblasts proliferation using different irradiance and same fluence. Lasers Surg Med 29:179–184
Olivi G, Genovese MD, Caprioglio C (2009) Evidence-based dentistry on laser paediatric dentistry: review and outlook. Eur J Paediatr Dent 10:29
Basso FG, Pansani TN, Turrioni APS, Bagnato VS, Hebling J, de Souza Costa CA (2012) In vitro wound healing improvement by low-level laser therapy application in cultured gingival fibroblasts. Int J Dent 2012:719452. https://doi.org/10.1155/2012/719452
Marques NCT, Neto NL, Prado MTO, Vitor LLR, Oliveira RC, Sakai VT, Santos CF, Machado MAAM, Oliveira TM (2017) Effects of PBM in different energy densities and irradiance on maintaining cell viability and proliferation of pulp fibroblasts from human primary teeth. Lasers Med Sci 32:1621–1628. https://doi.org/10.1007/s10103-017-2301-z
Pandeshwar P, Roa MD, Das R, Shastry SP, Kaul R, Srinivasreddy MB (2016) Photobiomodulation in oral medicine: a review. J Investig Clin Dent 7:114–126. https://doi.org/10.1111/jicd.12148
Ginani F, Soares DM, Barboza CAG (2015) Effect of low-level laser therapy on mesenchymal stem cell proliferation: a systematic review. Lasers Med Sci 30:2189–2194. https://doi.org/10.1007/s10103-015-1730-9
Peplow PV, Chung TY, Baxter GD (2010) Laser photobiomodulation of proliferation of cells in culture: a review of human and animal studies. Photomed Laser Surg 29:285–304. https://doi.org/10.1089/pho.2010.2846
Ferreira MPP, Ferrari RAM, Gravalos ED, Martins MD, Bussadori SK, Gonzalez DAB, Fernandes KPS (2009) Effect of low-energy gallium-aluminum-arsenide and aluminium gallium indium phosphide laser irradiation on the viability of C2C12 myoblasts in a muscle injury model. Photomed Laser Surg 27:901–906. https://doi.org/10.1089/pho.2008.2427
Damante CA, De Micheli G, Miyagi SPH, Feist IS, Marques MM (2009) Effect of laser phototherapy on the release of fibroblast growth factors by human gingival fibroblasts. Lasers Med Sci 24:885. https://doi.org/10.1007/s10103-008-0582-y
Marques MM, Pereira AN, Fujihara NA, Nogueira FN, Eduardo CP (2004) Effect of low-power laser irradiation on protein synthesis and ultrastructure of human gingival fibroblasts. Lasers Surg Med 34:260–265. https://doi.org/10.1002/lsm.20008
Eduardo FDP, Bueno DF, de Freitas PM, Marques MM, Passos-Bueno MR, Eduardo CDP, Zatz M (2008) Stem cell proliferation under low intensity laser irradiation: a preliminary study. Lasers Surg Med 40:433–438. https://doi.org/10.1002/lsm.20646
Volpato LER, de Oliveira RC, Machado MAAM, Espinosa MM, Bagnato VS (2011) Viability of fibroblasts cultured under nutritional stress irradiated with red laser, infrared laser, and red light-emitting diode. J Biomed Opt 16:075004. https://doi.org/10.1117/1.3602850
Oliveira FA, Matos AA, Santesso MR, Tokuhara CK, Leite AL, Bagnato VS, Machado MA, Peres-Buzalaf C, Oliveira RC (2016) Low intensity lasers differently induce primary human osteoblast proliferation and differentiation. J Photochem Photobiol B 163:14–21. https://doi.org/10.1016/j.jphotobiol.2016.08.006
Fernandes MH (1998) Regulation mechanisms of bone metabolism. Acta Medica Port 11:41–52
Souza LM, Rinco UG, Aguiar DAC, de Almeida Junior LA, Silva LC, Oliveira TM, Sakai VT, Marques NCT (2018) Effect of low-level laser therapy on viability and proliferation of stem cells from exfoliated deciduous teeth under different nutritional conditions. Laser Phys 28:025603 (5pp)
Smith KC (1991) The photobiological basis of low level laser radiation therapy. Laser Therapy 3:19–24
Karu TI (1988) Molecular mechanism of the therapeutic effect of low-intensity laser radiation. Lasers Life Sci 2:53–74
Moura-Netto C, Ferreira LS, Maranduba CM, Mello-Moura ACV, Marques MM (2016) Low-intensity laser phototherapy enhances the proliferation of dental pulp stem cells under nutritional deficiency. Braz Oral Res 30:1. https://doi.org/10.1590/1807-3107BOR-2016.vol30.0080
Ginani F, Soares DM, de Oliveira Rocha HA, de Souza LB, Barboza CAG (2018) Low-level laser irradiation induces in vitro proliferation of stem cells from human exfoliated deciduous teeth. Lasers Med Sci 33:95–102. https://doi.org/10.1007/s10103-017-2355-y
Diniz IMA, Matos AB, Marques MM (2015) Laser phototherapy enhances mesenchymal stem cells survival in response to the dental adhesives. Sci World J 2015:671789. https://doi.org/10.1155/2015/671789
Tunér J, Jenkins PA (2016) Parameter reproducibility in photobiomodulation. Photomed Laser Surg 34:91–92. https://doi.org/10.1089/pho.2016.4105
Acknowledgments
The authors would like to thank the Minas Gerais Research Foundation (FAPEMIG) and Coordination for the Improvement of Higher Education Personnel (CAPES) for the financial support.
Funding
This study was financially supported by Minas Gerais Research Foundation (FAPEMIG, Brazil, no. APQ-04004-16) and Coordination for the Improvement of Higher Education Personnel (CAPES, Brazil, no. 88881.068437/2014-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Institutional Review Board regarding ethical aspects (protocol no. 46420), and the procedures were performed according to the Helsinki Declaration.
Rights and permissions
About this article
Cite this article
Marques, N.P., Lopes, C.S., Marques, N.C.T. et al. A preliminary comparison between the effects of red and infrared laser irradiation on viability and proliferation of SHED. Lasers Med Sci 34, 465–471 (2019). https://doi.org/10.1007/s10103-018-2615-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-018-2615-5