Abstract
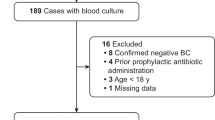
Staphylococcus aureus (SA) is the leading cause of bloodstream infection (BSI). The incidence of methicillin-resistant SA (MRSA) has decreased in France and Europe since one decade. Early and precise prediction of methicillin susceptibility is needed to improve probabilistic antibiotic therapy of MRSA-BSI. The aim of this study was to identify MRSA-BSI risk factors at admission and evaluate which patients need costly rapid diagnostic tests. A single-center retrospective descriptive study of all diagnosed SA-BSI was conducted in a French University Hospital between January 2015 and December 2016. All medical charts were reviewed. Univariate and multivariate analyses by a logistic regression model were performed on the data. We then build a prediction score of MRSA-BSI by assigning one point for each of the risk factor identified. During the study period, 151 SA-BSI were identified including 32 (21%) MRSA-BSI. In multivariate analysis, three factors were associated with MRSA-BSI: coming from long-term care facility, known previous MRSA colonization and/or infection, and chronic renal disease. Among our population, respectively, 5% and 100% had a MRSA-BSI when no or three risk factors were identified. Therefore, among the PCR performed, 43 (96%) could be avoided according to our clinical score. In our study, methicillin-susceptible SA and MRSA-BSI can be predictable by counting MRSA risk factors. This prediction rule could avoid the use of expensive rapid diagnostic tests. Prospective studies and prediction rules could help physicians to predict SA-BSI susceptibility to improve appropriate empiric therapy choice.

Similar content being viewed by others
References
Keynan Y, Rubinstein E (2013) Staphylococcus aureus bacteremia, risk factors, complications, and management. Crit Care Clin 29:547–562. https://doi.org/10.1016/j.ccc.2013.03.008
Lodise TP, McKinnon PS, Swiderski L, Rybak MJ (2003) Outcomes analysis of delayed antibiotic treatment for hospital-acquired Staphylococcus aureus bacteremia. Clin Infect Dis 36:1418–1423. https://doi.org/10.1086/375057
Gómez J, García-Vázquez E, Baños R, Canteras M, Ruiz J, Baños V et al (2007) Predictors of mortality in patients with methicillin-resistant Staphylococcus aureus (MRSA) bacteraemia: the role of empiric antibiotic therapy. Eur J Clin Microbiol Infect Dis 26:239–245. https://doi.org/10.1007/s10096-007-0272-x
Soriano A, Marco F, Martinez JA, Pisos E, Almela M, Dimova VP et al (2008) Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis 46:193–200. https://doi.org/10.1086/524667
Rodríguez-Baño J, Millán AB, Domínguez MA, Borraz C, González MP, Almirante B et al (2009) Impact of inappropriate empirical therapy for sepsis due to health care-associated methicillin-resistant Staphylococcus aureus. J Inf Secur 58:131–137. https://doi.org/10.1016/j.jinf.2008.11.003
Paul M, Kariv G, Goldberg E, Raskin M, Shaked H, Hazzan R et al (2010) Importance of appropriate empirical antibiotic therapy for methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother 65:2658–2665. https://doi.org/10.1093/jac/dkq373
Bassetti M, Trecarichi EM, Mesini A, Spanu T, Giacobbe DR, Rossi M et al (2012) Risk factors and mortality of healthcare-associated and community-acquired Staphylococcus aureus bacteraemia. Clin Microbiol Infect 18:862–869. https://doi.org/10.1111/j.1469-0691.2011.03679.x
Khatib R, Saeed S, Sharma M, Riederer K, Fakih MG, Johnson LB (2006) Impact of initial antibiotic choice and delayed appropriate treatment on the outcome of Staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis 25:181–185. https://doi.org/10.1007/s10096-006-0096-0
Stryjewski ME, Szczech LA, Benjamin DK, Inrig JK, Kanafani ZA, Engemann JJ et al (2007 Jan 15) Use of vancomycin or first-generation cephalosporins for the treatment of hemodialysis- dependent patients with methicillin-susceptible Staphylococcus aureus bacteremia 2018:7. Clin Infect Dis 44(2):190–196
Schweizer ML, Furuno JP, Harris AD, Johnson JK, Shardell MD, McGregor JC et al (2011) Comparative effectiveness of nafcillin or cefazolin versus vancomycin in methicillin-susceptible Staphylococcus aureus bacteremia. BMC Infect Dis 11. https://doi.org/10.1186/1471-2334-11-279
Horino T, Sato F, Hosaka Y, Hoshina T, Tamura K, Nakaharai K et al (2015) Predictive factors for metastatic infection in patients with bacteremia caused by methicillin-sensitive Staphylococcus aureus. Am J Med Sci 349:24–28. https://doi.org/10.1097/MAJ.0000000000000350
McDanel JS, Perencevich EN, Diekema DJ, Herwaldt LA, Smith TC, Chrischilles EA et al (2015) Comparative effectiveness of beta-lactams versus vancomycin for treatment of methicillin-susceptible Staphylococcus aureus bloodstream infections among 122 hospitals. Clin Infect Dis 61:361–367. https://doi.org/10.1093/cid/civ308
Wong D, Wong T, Romney M, Leung V. Comparative effectiveness of β-lactam versus vancomycin empiric therapy in patients with methicillin-susceptible Staphylococcus aureus (MSSA) bacteremia. Ann Clin Microbiol Antimicrob 2016;15:27. https://doi.org/10.1186/s12941-016-0143-3
Jarlier V, Arnaud I. (2017) Surveillance des bactéries multirésistantes dans les établissements de santé. Réseau BMR-Raisin, France. Résultats 2015. Saint-Maurice : Santé publique France, 112 p
Daniau C, Léon L, Blanchard H, Bernet C, Caillet-Vallet E et al. (2018) Enquête nationale de prévalence des infections nosocomiales et des traitements anti-infectieux en établissements de santé, France, mai-juin 2017. Saint-Maurice : Santé Publique France ; 12 p
Meyer E, Schwab F, Schroeren-Boersch B, Gastmeier P (2011) Increasing consumption of MRSA-active drugs without increasing MRSA in German ICUs. Intensive Care Med 37:1628–1632. https://doi.org/10.1007/s00134-011-2335-9
Delport JA, Mohorovic I, Burn S, McCormick JK, Schaus D, Lannigan R et al (2016) Rapid detection of meticillin-resistant Staphylococcus aureus bacteraemia using combined three-hour short-incubation matrix-assisted laser desorption/ionization time-of-flight MS identification and Alere culture colony PBP2a detection test. J Med Microbiol 65(7):626–631. https://doi.org/10.1099/jmm.0.000285
Heraud S, Freydiere A-M, Doleans-Jordheim A, Bes M, Tristan A, Vandenesch F et al (2015) Direct identification of Staphylococcus aureus and determination of methicillin susceptibility from positive blood-culture bottles in a Bact/ALERT system using Binax Now S. aureus and PBP2a tests. Ann Lab Med 35:454. https://doi.org/10.3343/alm.2015.35.4.454
Wolk DM, Struelens MJ, Pancholi P, Davis T, Della-Latta P, Fuller D et al (2009) Rapid detection of Staphylococcus aureus and methicillin-resistant S. aureus (MRSA) in wound specimens and blood cultures: multicenter preclinical evaluation of the Cepheid Xpert MRSA/SA skin and soft tissue and blood culture assays. J Clin Microbiol 47:823–826. https://doi.org/10.1128/JCM.01884-08
Brown J, Paladino JA (2010) Impact of rapid methicillin-resistant Staphylococcus aureus polymerase chain reaction testing on mortality and cost effectiveness in hospitalized patients with bacteraemia: a decision model. PharmacoEconomics 28:567–575. https://doi.org/10.2165/11533020-000000000-00000
Page A, O’Rourke S, Brennan M, Clooney L, Le Blanc D, Griffin J et al (2017 Nov 1) Impact of Xpert MRSA/SA blood culture PCR assay on management of positive blood cultures in obstetric patients: a retrospective audit. Ir J Med Sci 186(4):995–998. https://doi.org/10.1007/s11845-017-1581-4
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP et al (2002) Health care--associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 137:791–797
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332. https://doi.org/10.1016/j.ajic.2008.03.002
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA et al (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 101:1644–1655. https://doi.org/10.1378/chest.101.6.1644
Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S et al (2007) Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 298:1763–1771. https://doi.org/10.1001/jama.298.15.1763
Burkey M, Wilson L, Moore R, Lucas G, Francis J, Gebo K (2008) The incidence of and risk factors for MRSA bacteraemia in an HIV-infected cohort in the HAART era. HIV Med. https://doi.org/10.1111/j.1468-1293.2008.00629.x
Callejo-Torre F, Eiros Bouza JM, Olaechea Astigarraga P, Coma Del Corral MJ, Palomar Martínez M, Alvarez-Lerma F et al (2016 Sep 1) Risk factors for methicillin-resistant Staphylococcus aureus colonisation or infection in intensive care units and their reliability for predicting MRSA on ICU admission. Infez Med 24(3):201–209
Kao K-C, Chen C-B, Hu H-C, Chang H-C, Huang C-C, Huang Y-C. Risk factors of methicillin-resistant Staphylococcus aureus infection and correlation with nasal colonization based on molecular genotyping in medical intensive care units: a prospective observational study. Medicine (Baltimore) 2015;94:e1100. https://doi.org/10.1097/MD.0000000000001100
Bouchiat C, Curtis S, Spiliopoulou I, Bes M, Cocuzza C, Codita I et al (2017) MRSA infections among patients in the emergency department: a European multicentre study. J Antimicrob Chemother 72:372–375. https://doi.org/10.1093/jac/dkw431
Conterno LO, Shymanski J, Ramotar K, Toye B, van Walraven C, Coyle D et al (2007) Real-time polymerase chain reaction detection of methicillin-resistant Staphylococcus aureus: impact on nosocomial transmission and costs. Infect Control Hosp Epidemiol 28:1134–1141. https://doi.org/10.1086/520099
Stürenburg E (2009) Rapid detection of methicillin-resistant Staphylococcus aureus directly from clinical samples: methods, effectiveness and cost considerations. GMS Ger Med Sci 7. https://doi.org/10.3205/000065
Davis TE, Fuller DD, Aeschleman EC (1992) Rapid, direct identification of Staphylococcus aureus and Streptococcus pneumoniae from blood cultures using commercial immunologic kits and modified conventional tests. Diagn Microbiol Infect Dis 15:295–300. https://doi.org/10.1016/0732-8893(92)90014-K
Thirunavukkarasu S, Rathish K.C. Evaluation of direct tube coagulase test in staphylococcal bacteremia. J Clin Diagn Res 2014 May; 8(5): DC19–DC21. https://doi.org/10.7860/JCDR/2014/6687.4371
Walter J, Noll I, Feig M, Weiss B, Claus H, Werner G et al (2017) Decline in the proportion of methicillin resistance among Staphylococcus aureus isolates from non-invasive samples and in outpatient settings, and changes in the co-resistance profiles: an analysis of data collected within the Antimicrobial Resistance Surveillance Network, Germany 2010 to 2015. BMC Infect Dis 17. https://doi.org/10.1186/s12879-017-2271-6
Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y (2003) Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 36:53–59. https://doi.org/10.1086/345476
Nolan CM, Beaty HN (1976) Staphylococcus aureus bacteremia. Current clinical patterns. Am J Med 60:495–500
Finkelstein R, Sobel JD, Nagler A, Merzbach D (1984) Staphylococcus aureus bacteremia and endocarditis: comparison of nosocomial and community-acquired infection. J Med 15:193–211
Author information
Authors and Affiliations
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
Ethical approval was not required as all procedures were part of our routine care. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki Declaration and its later amendments. This article does not contain any studies with animals performed by any of the authors.
Informed consent
All data of this retrospective study were fully anonymized before the study authors accessed them.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Delerue, T., Cordel, H., Delerue, T. et al. Prediction of methicillin-resistant Staphylococcus aureus bloodstream infection: do we need rapid diagnostic tests?. Eur J Clin Microbiol Infect Dis 38, 1319–1326 (2019). https://doi.org/10.1007/s10096-019-03556-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03556-5