Abstract
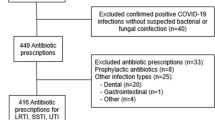
The purpose of this investigation was to describe the impact of an early review of antibiotic prescriptions in a hospital using unsolicited infectious disease physician (IDP) counselling, identify areas for improvement and examine factors associated with physicians’ non-compliance. The prescriptions of 15 selected antibiotics from surgical or medical wards were screened daily and reviewed between days 3 and 5 by a single IDP during an 8-month period to identify those likely needing counselling. Improved antibiotic use was sought by encouraging ward physicians to withdraw or de-escalate therapy, promoting oral switch or reducing the duration of therapy whenever appropriate. Variables potentially associated with IDP counselling and physicians’ non-compliance were tested using bivariate analysis and then entered in a logistic regression model. Among 857 prescriptions analysed, 54.6 % prompted unsolicited counselling, mostly for stopping therapy (18.8 %), reducing its duration (18.0 %) or de-escalation (13.0 %). Variables independently associated with IDP counselling included antibiotic combination (adjusted odds ratio [aOR], 5.27 [95 % confidence interval (CI), 1.80–15.45]; p = 0.002), non-clinically documented infection (aOR, 4.98 [95 % CI, 2.81–8.82]; p < 0.001) and microbiologically documented infection (aOR, 2.04 [95 % CI, 1.51–2.75]; p < 0.001). The physicians’ compliance rate was 77.3 %. Variables independently associated with physicians’ non-compliance to the IDP recommendation were the surgical speciality of the ward physician (aOR, 1.91 [95 % CI, 1.17–3.12]; p = 0.009) and advice to reduce the duration of therapy (aOR, 1.88 [95 % CI, 1.12–3.15]; p = 0.017). An unsolicited post-prescription antibiotic review can be successfully implemented with a high rate of physicians’ compliance. Areas for targeting improvement measures include prescriptions in surgical wards and shortening the duration of therapy.

Similar content being viewed by others
References
Dellit TH, Owens RC, McGowan JE Jr et al (2007) Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 44:159–177
MacDougall C, Polk RE (2005) Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev 18:638–656
Owens RC Jr (2008) Antimicrobial stewardship: concepts and strategies in the 21st century. Diagn Microbiol Infect Dis 61:110–128
Lesprit P, Duong T, Girou E, Hemery F, Brun-Buisson C (2009) Impact of a computer-generated alert system prompting review of antibiotic use in hospitals. J Antimicrob Chemother 63:1058–1063
Lesprit P, Landelle C, Girou E, Brun-Buisson C (2010) Reassessment of intravenous antibiotic therapy using a reminder or direct counselling. J Antimicrob Chemother 65:789–795
Sellier E, Pavese P, Gennai S, Stahl JP, Labarère J, François P (2010) Factors and outcomes associated with physicians’ adherence to recommendations of infectious disease consultations for inpatients. J Antimicrob Chemother 65:156–162
Pulcini C, Pradier C, Samat-Long C et al (2006) Factors associated with adherence to infectious diseases advice in two intensive care units. J Antimicrob Chemother 57:546–550
Carling P, Fung T, Killion A, Terrin N, Barza M (2003) Favorable impact of a multidisciplinary antibiotic management program conducted during 7 years. Infect Control Hosp Epidemiol 24:699–706
Camins BC, King MD, Wells JB et al (2009) Impact of an antimicrobial utilization program on antimicrobial use at a large teaching hospital: a randomized controlled trial. Infect Control Hosp Epidemiol 30:931–938
Kim BN (2005) Compliance with an infectious disease specialist’s advisory consultations on targeted antibiotic usage. J Infect Chemother 11:84–88
Cosgrove SE, Patel A, Song X et al (2007) Impact of different methods of feedback to clinicians after postprescription antimicrobial review based on the Centers for Disease Control and Prevention’s 12 Steps to Prevent Antimicrobial Resistance Among Hospitalized Adults. Infect Control Hosp Epidemiol 28:641–646
Schlesinger Y, Paltiel O, Yinnon AM (1988) Analysis and impact of infectious disease consultations in a general hospital. J Hosp Infect 40:39–46
Lemmen SW, Häfner H, Kotterik S, Lütticken R, Töpper R (2000) Influence of an infectious disease service on antibiotic prescription behavior and selection of multiresistant pathogens. Infection 28:384–387
Gómez J, Conde Cavero SJ, Hernández Cardona JL et al (1996) The influence of the opinion of an infectious disease consultant on the appropriateness of antibiotic treatment in a general hospital. J Antimicrob Chemother 38:309–314
Fowler VG Jr, Sanders LL, Sexton DJ et al (1998) Outcome of Staphylococcus aureus bacteremia according to compliance with recommendations of infectious diseases specialists: experience with 244 patients. Clin Infect Dis 27:478–486
Byl B, Clevenbergh P, Jacobs F et al (1999) Impact of infectious diseases specialists and microbiological data on the appropriateness of antimicrobial therapy for bacteremia. Clin Infect Dis 29:60–66
Jenkins TC, Price CS, Sabel AL, Mehler PS, Burman WJ (2008) Impact of routine infectious diseases service consultation on the evaluation, management, and outcomes of Staphylococcus aureus bacteremia. Clin Infect Dis 46:1000–1008
Yinnon AM (2001) Whither infectious diseases consultations? Analysis of 14,005 consultations from a 5-year period. Clin Infect Dis 33:1661–1667
Mol PGM, Wieringa JE, NannanPanday PV et al (2005) Improving compliance with hospital antibiotic guidelines: a time-series intervention analysis. J Antimicrob Chemother 55:550–557
Lo E, Rezai K, Evans AT et al (2004) Why don’t they listen? Adherence to recommendations of infectious disease consultations. Clin Infect Dis 38:1212–1218
Glowacki RC, Schwartz DN, Itokazu GS, Wisniewski MF, Kieszkowski P, Weinstein RA (2003) Antibiotic combinations with redundant antimicrobial spectra: clinical epidemiology and pilot intervention of computer-assisted surveillance. Clin Infect Dis 37:59–64
Pulcini C, Cua E, Lieutier F, Landraud L, Dellamonica P, Roger PM (2007) Antibiotic misuse: a prospective clinical audit in a French university hospital. Eur J Clin Microbiol Infect Dis 26:277–280
Méan M, Pavese P, Tudela E, Dinh-Van KA, Mallaret MR, Stahl JP (2006) Consultations with infectious disease specialists for patients in a teaching hospital: adherence in 174 cases. Presse Med 35:1461–1466
Sipahi OR, Tasbakan M, Pullukcu H et al (2007) Accuracy of consultations performed by infectious diseases trainees and factors associated with adherence to them. Int J Infect Dis 11:518–523
Tenenbaum MJ (2004) Infectious diseases consultative recommendations: if heard, they can be listened to. Clin Infect Dis 38:1219–1221
Madariaga MG (2006) Non-adherence to infectious disease consultations: are surgeons to blame? J Antimicrob Chemother 57:1019–1020
Chastre J, Wolff M, Fagon JY et al (2003) Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA 290:2588–2598
Guillemot D, Carbon C, Balkau B et al (1998) Low dosage and long treatment duration of beta-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA 279:365–370
Hayashi Y, Paterson DL (2011) Strategies for reduction in duration of antibiotic use in hospitalized patients. Clin Infect Dis 52:1232–1240
Amadeo B, Dumartin C, Parneix P, Fourrier-Réglat A, Rogues AM (2011) Relationship between antibiotic consumption and antibiotic policy: an adjusted analysis in the French healthcare system. J Antimicrob Chemother 66:434–442
Davey P, Brown E, Fenelon L et al. (2005) Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev (4):1–116
Funding
None.
Transparency declarations
None to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lesprit, P., Landelle, C. & Brun-Buisson, C. Unsolicited post-prescription antibiotic review in surgical and medical wards: factors associated with counselling and physicians’ compliance. Eur J Clin Microbiol Infect Dis 32, 227–235 (2013). https://doi.org/10.1007/s10096-012-1734-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1734-3