Abstract
Background
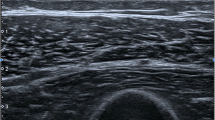
Rigidity is one of the major manifestations of Parkinson’s disease (PD), but no quantitative and objective imaging method has been developed to measure rigidity. Ultrasound shear wave elastography (SWE) can reflect the stiffness of tissue by providing a quantitative index. Thus, we conducted this study to evaluate the potential clinical value of SWE in assessing rigidity in PD.
Methods
A total of 63 subjects (44 patients with rigidity-dominant PD and 19 right-dominant-hand normal controls with matched age) were enrolled, and each underwent ultrasound SWE testing. The tests were conducted on the brachioradialis (BR) and biceps brachii (BB) on the more affected side in patients with PD and on the right side in normal controls. Differences in quantitative shear wave velocity (SWV) between patients with PD and normal controls were determined. The relationship of muscle SWV with joint rigidity, UPDRSIII, disease duration, sex, and age in patients with PD was analyzed. The intraclass correlation coefficient (ICC) was used to evaluate the reliability of SWE in assessing muscle stiffness in patients with PD.
Results
The mean SWVs of the BB and BR were higher in the PD group (3.65±0.46 and 4.62±0.89 m/s, respectively) than in normal controls (2.79±0.37 and 3.26±0.40 m/s, respectively). Stiffness in BR and BB was correlated with the upper-limb joint rigidity, UPDRSIII, and disease duration but not with sex or age in the PD group. The intraobserver correlation coefficients (ICCs) for interobserver and intraobserver variations in measuring SWV were 0.85 (95% confidence interval 0.56–0.95) and 0.85 (95% confidence interval 0.58–0.95), respectively, for BR and 0.90 (95% confidence interval 0.73–0.97) and 0.86 (95% confidence interval 0.61–0.95), respectively, for BB.
Conclusions
SWV is associated with joint rigidity and disease duration, indicating that SWE can be potentially used as an objective and quantitative tool for evaluating rigidity.




Similar content being viewed by others
Change history
02 March 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10072-021-05150-0
References
Yu HX, Guo MR, Li G, Zhang B (2020) Association between fatigue and motor progression in Parkinson’s disease in southern Chinese. Neurol Sci 41(1):161–164. https://doi.org/10.1007/s10072-019-04059-z
Shimo Y, Hatano T, Sakurai M, Sekimoto S, Marisdina S, Hattori N (2020) Freezing of gait in Parkinson’s disease may share the mechanisms of dystonia. Neurol Sci 41(5):1285–1286. https://doi.org/10.1007/s10072-019-04155-0
Liu G, Chen H, Su D, Wang D, Zhang M, Wang X, Wang Z, Yang Y, Jiang Y, Feng T (2020) Risk thresholds of levodopa dose for dyskinesia in Chinese patients with Parkinson’s disease: a pilot study. Neurol Sci 41(10):111–118. https://doi.org/10.1007/s10072-019-04043-7
Richards M, Marder K, Cote L, Mayeux R (1994) Interrater reliability of the Unified Parkinson’s Disease Rating Scale motor examination. Mov Disord 9(1):89–91. https://doi.org/10.1002/mds.870090114
Teshuva I, Hillel I, Gazit E, Giladi N, Mirelman A, Hausdorff JM (2019) Using wearables to assess bradykinesia and rigidity in patients with Parkinson's disease: a focused, narrative review of the literature. J Neural Transm (Vienna) 126(6):699–710. https://doi.org/10.1007/s00702-019-02017-9
Teravainen H, Tsui JK, Mak E, Calne DB (1989) Optimal indices for testing parkinsonian rigidity. Can J Neurol Sci 16(2):180–183. https://doi.org/10.1017/s0317167100028857
Lee HM, Huang YZ, Chen JJ, Hwang IS (2002) Quantitative analysis of the velocity related pathophysiology of spasticity and rigidity in the elbow flexors. J Neurol Neurosurg Psychiatry 72:621–629. https://doi.org/10.1136/jnnp.72.5.621
Nuyens G, De Weerdt W, Dom R, Nieuwboer A (2000) Torque variations during repeated passive isokinetic movements of the knee in subjects with Parkinson’s disease and healthy control subjects. Parkinsonism Relat Disord 6:87–93. https://doi.org/10.1016/S1353-8020(99)00055-3
Basford JR, Jenkyn TR, An KN, Ehman RL, Heers G, Kaufman KR (2002) Evaluation of healthy and diseased muscle with magnetic resonance elastography. Arch Phys Med Rehabil 83(11):1530–1536. https://doi.org/10.1053/apmr.2002.35472
Jenkyn TR, Ehman RL, An KN (2003) Noninvasive muscle tension measurement using the novel technique of magnetic resonance elastography (MRE). J Biomech 36(12):1917–1921. https://doi.org/10.1016/s0021-9290(03)00005-8
Barr RG, Nakashima K, Amy D, Cosgrove D, Farrokh A, Schafer F, Bamber JC, Castera L, Choi BI, Chou YH, Dietrich CF, Ding H, Ferraioli G, Filice C, Friedrich-Rust M, Hall TJ, Nightingale KR, Palmeri ML, Shiina T, Suzuki S, Sporea I, Wilson S, Kudo M (2015) WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: breast. Ultrasound Med Biol 41(5):1148–1160. https://doi.org/10.1016/j.ultrasmedbio.2015.03.008
Cosgrove D, Barr R, Bojunga J, Cantisani V, Chammas MC, Dighe M, Vinayak S, Xu JM, Dietrich CF (2017) WFUMB guidelines and recommendations on the clinical use of ultrasound elastography: Part 4. Thyroid. Ultrasound Med Biol 43(1):4–26. https://doi.org/10.1016/j.ultrasmedbio.2016.06.022
Dietrich CF, Bamber J, Berzigotti A, Bota S, Cantisani V, Castera L, Cosgrove D, Ferraioli G, Friedrich-Rust M, Gilja OH, Goertz RS, Karlas T, de Knegt R, de Ledinghen V, Piscaglia F, Procopet B, Saftoiu A, Sidhu PS, Sporea I, Thiele M (2017) EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, Update 2017 (Short Version). Ultraschall Med 38(4):377–394. https://doi.org/10.1055/s-0043-103955
Yoshida K, Itoigawa Y, Maruyama Y, Saita Y, Takazawa Y, Ikeda H, Kaneko K, Sakai T, Okuwaki T (2017) Application of shear wave elastography for the gastrocnemius medial head to tennis leg. Clin Anat 30(1):114–119. https://doi.org/10.1002/ca.22788
Brandenburg JE, Eby SF, Song P, Zhao H, Brault JS, Chen S, An KN (2014) Ultrasound elastography: the new frontier in direct measurement of muscle stiffness. Arch Phys Med Rehabil 95(11):2207–2219. https://doi.org/10.1016/j.apmr.2014.07.007
Alfuraih AM, O'Connor P, Hensor E, Tan AL, Emery P, Wakefield RJ (2018) The effect of unit, depth, and probe load on the reliability of muscle shear wave elastography: variables affecting reliability of SWE. J Clin Ultrasound 46(2):108–115. https://doi.org/10.1002/jcu.22534
Du LJ, He W, Cheng LG, Li S, Pan YS, Gao J (2016) Ultrasound shear wave elastography in assessment of muscle stiffness in patients with Parkinson’s disease: a primary observation. Clin Imaging 40(6):1075–1080. https://doi.org/10.1016/j.clinimag.2015.12.008
Choo XY, Lim SY, Chinna K, Tan YJ, Yong VW, Lim JL, Lau KF, Chung JY, Em JM, Tan HT, Lim JH, Tan SB, Tan CT, Tan AH (2020) Understanding patients’ and caregivers’ perspectives and educational needs in Parkinson’s disease: a multi-ethnic Asian study. Neurol Sci 41(10):2831–2842. https://doi.org/10.1007/s10072-020-04396-4
Becker G, Seufert J, Bogdahn U, Reichmann H, Reiners K (1995) Degeneration of substantia nigra in chronic Parkinson's disease visualized by transcranial color-coded real-time sonography. Neurology 45(1):182–184. https://doi.org/10.1212/wnl.45.1.182
Luo WF, Zhang YC, Sheng YJ, Fang JC, Liu CF (2012) Transcranial sonography on Parkinson's disease and essential tremor in a Chinese population. Neurol Sci 33(5):1005–1009. https://doi.org/10.1007/s10072-011-0876-x
Dong ZF, Wang CS, Zhang YC, Zhang Y, Sheng YJ, Hu H, Luo WF, Liu CF (2017) Transcranial sonographic alterations of substantia nigra and third ventricle in Parkinson’s disease with or without dementia. Chin Med J 130(19):2291–2295. https://doi.org/10.4103/0366-6999.215329
Shi J, Xue ZY, Yk D, Peng B, Dong Y, Zhang YC (2018) Cascaded multi-column RVFL+ classifier for single-modal neuroimaging-based diagnosis of Parkinson’s disease. IEEE Trans Biomed Eng 66(8):2362–2371. https://doi.org/10.1109/TBME.2018.2889398
Shen L, Shi J, Dong Y, Ying S, Peng Y, Chen L, Zhang Q, An H, Zhang Y (2019) An improved deep polynomial network algorithm for transcranial sonography–based diagnosis of Parkinson’s disease. Cogn Comput 12:553–562. https://doi.org/10.1007/s12559-019-09691-7
Watts RL, Wiegner AW, Young RR (1986) Elastic properties of muscles measured at the elbow in man: II. Patients with Parkinsonian rigidity. Neurol Neurosurg Psychiatry 49:1177–1181. https://doi.org/10.1136/jnnp.49.10.1177
Marusiak J, Kisiel-Sajewicz K, Jaskólska A, Jaskólski A (2010) Higher muscle passive stiffness in Parkinson’s disease patients than in controls measured by myotonometry. Arch Phys Med Rehabil 91(5):800–802. https://doi.org/10.1016/j.apmr.2010.01.012
Gao J, He W, Du LJ, Li S, Cheng LG, Shih G, Rubin J (2016) Ultrasound strain elastography in assessment of resting biceps brachii muscle stiffness in patients with Parkinson’s disease: a primary observation. Clin Imaging 40(3):440–444. https://doi.org/10.1016/j.clinimag.2015.12.008
Meara R, Cody F (1992) Relationship between electromyographic activity and clinically assessed rigidity studied at the wrist joint in Parkinson's disease. Brain J Neurol 115(Pt 4):1167–1180. https://doi.org/10.1093/brain/115.4.1167
Pollock L, Davis L (1931) Muscle tone in Parkinsonian states. J Nerv Ment Dis 74:669. https://doi.org/10.1001/archneurpsyc.1930.02220080087006
Fung VS, Burne JA, Morris JG (2000) Objective quantification of resting and activated parkinsonian rigidity:a comparison of angular impulse and work scores. Mov Disord 15:48–55. https://doi.org/10.1002/1531-8257(200001)15:1<48:aid-mds1009>3.0.co;2-e
Rossi B, Siciliano G, Carboncini MC, Manca ML, Massetani R, Viacava P, Muratorio A (1996) Muscle modifications in Parkinson’s disease: myoelectric manifestations. Electroencephalogr Clin Neurophysiol 101:211–218. https://doi.org/10.1016/0924-980X(96)94672-X
Eiling E, Bryant AL, Petersen W, Murphy A, Hohmann E (2007) Effects of menstrual-cycle hormone fluctuations on musculotendinous stiffness and knee joint laxity. Knee Surg Sports Traumatol Arthrosc 15(2):126–132. https://doi.org/10.1007/s00167-006-0143-5
Eby SF, Cloud BA, Brandenburg JE, Giambini H, Song P, Chen S, Le Brasseur NK, An KN (2015) Shear wave elastography of passive skeletal muscle stiffness: influences of sex and age throughout adulthood. Clin Biomech (Bristol, Avon) 30(1):22–27. https://doi.org/10.1016/j.clinbiomech.2014.11.011
Alfuraih A, Tan AL, O'Connor P, Emery P, Wakefield R (2019) The effect of ageing on shear wave elastography muscle stiffness in adults. Aging Clin Exp Res 31(12):1755–1763. https://doi.org/10.1007/s40520-019-01139-0
Creze M, Nordez A, Soubeyrand M, Rocher L, Maitre X, Bellin MF (2018) Shear wave sonoelastography of skeletal muscle: basic principles, biomechanical concepts, clinical applications, and future perspectives. Skelet Radiol 47(4):457–471. https://doi.org/10.1007/s00256-017-2843-y
Acknowledgements
We thank all the volunteers (both PD patients and normal controls) for their contributions to this study.
Funding
This work was supported by the Development Center for Medical Science and Technology, National Health and Family Planning Commission of the People’s Republic of China (2017YFC0909100) and Jiangsu Commission of Health (Y2018105). This was also partly supported by the Second Affiliated Hospital of Soochow University Pre-research Project of the National Natural Science Foundation of China (SDFEYG1709).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This work has been approved by the ethical committees at Soochow University.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The original article contains an error. In Affiliation 2, “Psychiatry” should be change to “Neurology”. Author Affiliation should write as follows: 2Department of Neurology, The Second Affiliated Hospital of Soochow University, Suzhou, China.
Rights and permissions
About this article
Cite this article
Ding, C.W., Song, X., Fu, X.Y. et al. Shear wave elastography characteristics of upper limb muscle in rigidity-dominant Parkinson’s disease. Neurol Sci 42, 4155–4162 (2021). https://doi.org/10.1007/s10072-021-05088-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05088-3