Abstract
Objective
To report two cases of cranial multineuritis after severe acute respiratory syndrome caused by coronavirus-2.
Methods
Patients’ data were obtained from medical records of the clinical chart of dell’Angelo Hospital, Venice, Italy.
Results
The first patient is a 42-year-old male patient who developed, 10 days after the resolution of coronavirus-2 pneumonia and intensive care unit hospitalization with hyperactive delirium, a cranial multineuritis with asymmetric distribution (bilateral hypoglossus involvement and right Claude Bernard Horner syndrome). No albumin-cytologic dissociation was found in cerebrospinal fluid; severe bilateral denervation was detected in hypoglossus nerve, with normal EMG of other cranial muscles, blink reflex, and cerebral magnetic resonance with gadolinium. He presented a striking improvement after intravenous human immunoglobulin therapy.
The second case is a 67-year-old male patient who developed a cranial neuritis (left hypoglossus paresis), with dyslalia and deglutition difficulties. He had cerebrospinal fluid abnormalities (albumin-cytologic dissociation), no involvement of ninth and 10th cranial nerves, diffuse hyporeflexia, and brachial diparesis.
Discussion
Cranial neuritis is a possible neurological manifestation of coronavirus-2 pneumonia. Etiology is not clear: it is possible a direct injury of the nervous structures by the virus through olfactory nasopharyngeal terminations. However, the presence of albumin-cytological dissociation in one patient, the sparing of the sense of smell, and the response to human immunoglobulin therapy suggests an immune-mediated genesis of the disorder.
Similar content being viewed by others
Introduction
Novel outbreak with coronavirus began since December 2019. Different types of coronaviruses cause many syndromes, such as respiratory infections or systemic involvement. A new coronavirus, SARS CoV-2, has rapidly spread throughout China and other countries, representing a global, still ongoing, public health crisis. In February 2020, World Health Organization named the disease related to this novel virus “coronavirus disease 2019 (COVID-19).”
This virus is largely pathogenous, causes respiratory involvement and fever (cough, shortness of breath, sore throat until severe respiratory failure), myalgias/arthralgias and fatigue due to muscle involvement, and gastrointestinal symptoms (e.g., diarrhea, nausea, and vomiting). Since the first papers, it became evident that anosmia and ageusia were common in SARS CoV-2 patients, despite the gravity of the infection (mild or severe indifferently) underlying a certain neuroinvasive potential of the new virus [1].
Neurological involvement is very common in COVID infection (30% in non-severe and 45.5% in severe patients) [2, 3] and can be characterized by central nervous system manifestation (dizziness, headache, impaired consciousness, stroke, ataxia, pyramidal signs, and seizures) or peripheral nervous system involvement (taste impairment, smell impairment, vision impairment, and polyneuropathy, polyradiculoneuritis), and skeletal muscular injury (myositis, myalgias, fatigue) [4].
Pathogenesis of neurological symptoms is not completely defined, but there are more than one hypothesis. Neuroinvasion of central nervous system (CNS) through olfactory nerve via the cribriform plate with secondary medulla and fronto-temporal spreading is the main possible mechanism in patients with rhombencephalitis, SARS CoV-2 hemorrhagic encephalitis, pyramidal signs, and ataxia or epileptic seizures, also for the presence, in CNS and PNS neurons, of ACE2 receptors, for which the virus has a great tropism [5]. Olfactory and gustatory dysfunctions are very common in SARS CoV-2 infection, with or without nasal obstruction or rhinorrhea, often as the initial clinical presentation. A multicentre European study clarified that anosmia and ageusia are prevalent symptoms of COVID-19 infection [6]; direct invasion through ACE 2 receptor can justify spreading of the virus to cranial nerves without blood–brain barrier damage in sporadic cases of cranial neuritis. The hypothesis of a neuroinvasion was supposed also by previous anatomopathological studies in multiple sclerosis patients, with the detection of viruses in central nervous system, showing a certain neurotropism [7].
The presence of SARS CoV-2 in the general circulation, with greater viremia in more severe patients, can suggest also that, when virus arrives in the small brain vessel endothelium, it can interact, through its spike protein, with ACE2 receptors expressed in the capillary endothelium damaging the blood–brain barrier.
An immune-mediated genesis appears to be responsible for acute polyradiculoneuritis quite similar to the classic Guillain–Barré syndrome, which is common in patients during or immediately after infection with SARS CoV-2 virus.
Therefore, the virus could enter the SNC promoting a cytokine cascade whose immunologic pathways are not yet completely known.
In this report, we describe two post infectious cranial neuritis with mild or no blood–brain barrier damage in predischarged patient after a severe COVID-19 pneumonia.
Methods
Clinical data were obtained from electronic records of the pneumology center and the intensive care unit of dell’Angelo Hospital (Venice, Italy). Data from neurophysiological evaluation, magnetic resonance, and CSF analysis were collected by neurologist trained for COVID-19 neurological complications who is directly involved in visiting all COVID-19 patients with neurological complication since the beginning of the pandemic.
Written informed consent was obtained from the two patients.
Case presentation
On February 24, 2020 a 42-year-old male patient presented in emergency room for persisting dyspnea, diarrhea, and fever (38–39 °C) in the previous 6 days. He had a past mild allergic asthma history, with sporadic salbutamol use, a recent tight contact with a Chinese asymptomatic woman, and a recent travel by train to Milan (the week before the symptoms started). From February 16, 2020, he had cough without mucus production, described as dry and snappy: general practitioner started amoxicillin 2 days after the cough onset. On February 21, he started suffering from dyspnea and went to hospital.
In the emergency room, he underwent a blood sample (emergency checklist) showing increasing PCR without increasing of procalcitonin and normal white blood cell count. Arterial gas analysis showed an oxygen desaturation with mild hypoxemia; chest radiography was negative. D-Dimer, creatine phosphokinase, blood glucose, and hepatic and renal function were normal. After 3 h, he had been tested positive for SARS CoV-2 RNA on polymerase chain reaction (RT-PCR) with a nasopharyngeal swab. The day after repletion test confirmed positivity. General examination showed harsh vesicular murmur with bilateral basal crackles, high respiratory frequency, and no other signs. Neurological examination was negative. Chest CT scan showed patchy ground glass opacities, which tend to be predominantly peripheral and basal widespread areas, with initial consolidation aspects, recognizable to both lungs, especially in the cranial sectors of the upper and lower lobes, with preserved patency of the trachea and its bronchial branches. Patient was transferred to infectious disease department and started azithromycin and chlorochin therapy. He initially underwent not invasive ventilation with 60% inspired fraction (FiO2), with normal blood oxygenation. After 24 h, he had an important decreased saturation (O2 saturation 89–90%, low blood oxygen pressure pO2 = 57 mmHg at gas analysis) and was transferred to intensive care unit (ICU) after oral tracheal intubation. In the early days, he was pronated and had a strong sedation with propofol, midazolam, remifentanil, and a neuromuscular block with curare. From the beginning, he was treated with remdesivir without side effects. On March 11, blood oxygenation improved and anesthetics were reduced gradually; he was extubated and transferred to pneumology department on March 20. He was gradually mobilized, started eating independently with semiliquid food, and started physiotherapy.
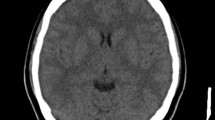
On March 30 and April 2, he had been tested negative for SARS CoV-2 RNA (nasopharyngeal swab). Since the first days after extubation, he developed dysarthria with slowness of articulation and low speech speed, with no sure swallowing difficulties (he complained of difficulty in bringing the food bolus down), and tongue movements difficulty, especially in sticking it out of the mouth. A neurological examination showed normal cognitive performance, normal language, and no symbolic function involvement. The cranial nerve examination showed miosis, ptosis, and enophthalmia limited to the right eye (Claude Bernard Horner syndrome); his pupils reacted briskly to light; ocular movements had no limitation nor was diplopia present; there were normal and symmetric mandibular and facial movements and normal cranic sensibility. The lower cranial nerves were normally functioning (no velum palatinum deviation, nor swallowing problems) except for global tongue hypotrophy with sporadic bilateral fasciculation, slow and incomplete extrusion movement both outwards and sideways, slow speech rate with impaired pitch control (Fig. 1). He had diffuse muscle hypotrophy, but strength and muscle tone were normal in all extremities, and no sensory deficits were detected for all modalities. There was no dysmetria on finger-to-nose and heel-to-shin tests. Muscle stretch was normal, but he had hyporeflexia in the upper and in the lower limbs. The plantar responses were flexor bilaterally.
A complete neurophysiological examination showed normal blink reflex and masseteric reflex study, normal electromyography (EMG) findings in masseter, orbicularis oris and oculi, and sternocleidomastoideus and trapezius muscles. In the genioglossus muscle, we found bilateral abundant spontaneous activity (fibrillation potentials, positive sharp waves); after tongue activation, we bilaterally registered a few motor unit action potentials (MUAPs) with low recruitment activity polyphasic morphology, normal amplitude, and mild increase of duration.
Electrophysiology study of the limb nerves showed low amplitude sensitive and motor action potentials with normal morphology and conduction velocity with disto-proximal distribution and F waves with normal latency, indicating a mild axonal polyneuropathy. EMG of proximal and distal limb muscles was normal. Motor and somatosensorial evoked potentials ruled out central pathway injuries showed. Brain magnetic resonance imaging was negative.
The blood workup revealed G-immunoglobulin with mild M-immunoglobulin positivity for CoV-2 virus (IgG anti-SARS CoV-2 15.06 AU/ml, IgM anti-SARS CoV-2 1.21 AU/ml). Anti-gangliosides (GM1, GM2, GM3, GD1a, GD1b, GD3, GT1a, GT1b, GQ1b) and anti-sulfatide antibodies in the serum were examined without any positivity. The cerebrospinal fluid (CSF) examination revealed a normal opening pressure, white blood cell count in the normal range (3 cells/mmc), normal CSF proteins (34 mg/dl), glucose (50 mg/dl, with 82 mg/dl blood level), with normal cytology, sterile cultures, and negative serologies, including RT-PCR for COVID-19 in CSF.
He then was treated with intravenously human immunoglobulin (2 g/kg in 5 days) starting 7 days after his neurological symptom’s onset. The cranial neuropathies improved significantly over the succeeding days, since after the third administration, and he started moving the tongue with more agility, reporting less sialorrhea and less dysarthria.
The control EMG, after 15 days since the last immunoglobulin infusion, showed a reduction of denervation in the tongue with ameliorated inference recruitment pattern, and abundant reinnervation. Patient was discharged at home: he had no swallowing nor salivation problems but only residual mild speech articulation problems (slow speech rate and modestly impaired pitch control).
The second patient, a 67-year-old male patient was admitted to hospital on March 17, 2020, with dry cough since the previous week and rest dyspnea. There was no smoking history nor significant disease in remote anamnesis. In emergency room, chest X-ray showed accentuation of the lung interstitial space at lung bases with ground glass aspects in the lower peri-hilar zone; SARS CoV-2 RNA (through nasopharyngeal swab) was detected. He was hospitalized in the infectious diseases department for an attempt of non-invasive ventilation with continue positive pressure (cPAP) but after 24 h was transferred to intensive care unit for acute respiratory failure (ARDS) after orotracheal intubation. He was treated with Ceftazidime and Avibactam, and he also developed a Klebsiella pneumoniae sepsis. During ICU staying, especially in the pronation phases during ventilation, he was treated with anesthetics (Propofol, Remifentanil, Midazolam, Ketamine) and noradrenalin for hemodynamic sustain. After tracheostomy, on April 14, he was extubated and transferred to pneumology department: he had weakness, especially in superior limbs, and he was scarcely reactive to the surrounding ambient. He had dysphagia for liquid without inhalation and difficulty moving the food bolus in the mouth, slow word articulation. The neurological examination showed hypotrophic tongue in the left side, with right deviation at rest and left deviation during protrusion. No other signs were present at cranic examination (normal pupils, ocular movement, other motor and sensitive function of cranic nerves). At segmentary level, there were mild hyposthenia, greater in proximal superior limbs, without sensibility involvement. Tendon reflexes were everywhere hypo-valid but not absent. Indifferent cutaneo-planctar response was detected bilaterally. A complete neurophysiological examination showed denervation in the left hypoglossus nerve, without other nerves involvement (Fig. 2). Electroneuromyography at 4 limbs showed mild amplitude reduction of sensitive and motor action potentials in all examined nerves (symmetrical and disto-proximal distribution) with mild denervation EMG pattern in arm proximal muscles. CSF analysis showed albumin-cytologic dissociation (52 mg/dl CSF protein, with 2 cells/mmc, normal glucose and cytology): negative was rRT-PCR for COVID-19 in CSF such as serum anti-ganglioside antibodies. Cerebral and cervical MRI was negative.
At the time of beginning of these neurological symptoms, SARS CoV-2 test through nasopharyngeal swab was negative (April 26). Intravenous human immunoglobulin treatment (2 g/kg in 5 days) was started, and since the beginning, there was a significative improvement, confirmed also with neurophysiological examination. The patient was subsequently transferred to rehabilitation hospital.
Discussion
The pathogenesis of cranial multineuropathy in the COVID-19 infection is not completely clear: it may be due to an immune mechanism or caused by direct viral nervous system invasion. Direct infection of nerve endings can be a possible mechanism of peripheral nervous system (PNS) involvement, with virus entering the PNS by binding to receptors on sensory and autonomic axon terminals of neurons, with a similar mechanism of Herpesviridae [8]. After axonal entry, virus particles must undergo retrograde transport to the cell body using motor proteins that move them along microtubules. By encoding several proteins using mRNA, the COVID-19 virus, like SARS CoV-2, uses a spike protein called S1 that enables the attachment of the virion to the cell membrane by interacting with host ACE2 receptor, which is ubiquitously exposed in central and peripheral nervous system [5, 9]. This hypothesis is lacking in the mechanism by which the virus can reach other cranial nerves after direct olfactory involvement without affecting the brainstem or the limbic system. In our cases, we have cranial neuritis (multiple and single consequently), in the first case without albumin cytological dissociation, in the second with mild CSF abnormalities (mild protein increase without oligoclonal bands): the first case suffered from hyperactive delirium even though there were no magnetic resonance alterations suggesting possible CNS involvement, and the second had no cognitive involvement or drowsiness nor other cranial nerves affected. No anosmia was reported for neither of them.
Another interesting pathogenetic hypothesis to explain cranial nerves involvement is the inflammatory hypothesis, such as in other case reports of post COVID-19 Guillain–Barré (GBS) or Miller Fisher syndrome (MFS) [7, 10,11,12]. For this hypothesis, researchers assume that after COVID infection, there is a late aberrant immune response, such as for other typical viruses or bacteria (campylobacter jejuni, flu viruses) frequently associated to MFS and GBS. Both our patients punctually developed neuropathic symptoms 1 month after contracting the infection: SARS CoV-2 test was almost negative at the clinical presentation of neurological signs and pneumonia was improving.
Many researchers have investigated before the etiology of cranial multineuropathy, hypothesizing a common genesis with GBS and MFS. GBS Classification Group outlined the latest diagnostic classification system for Guillain–Barré and Miller Fisher syndrome in 2014 [13], based on the clinical features of each disease. These neuropathies, in the majority of cases, could be classified into discrete subtypes or, in some instances, overlap between subtypes, based on phenotypic appearances. There remains, however, some ambiguity as to how best classify a small subset of patients, who develop multiple, often asymmetric, cranial neuropathies in the absence of ataxia or limb weakness nor drowsiness. Since the first descriptions of cases of GBS, ancient neurologists described sporadic cases of cranial multineuropathy, with mild albumin-cytologic dissociation and reduction of tendon reflexes [14, 15]. Our cases had weak reflexes at four limbs (achilleus absent) with a mild axonal sensory-motor symmetrical polyneuropathy, which not surely could be an overlapping critical area neuropathy. We did not find SARS CoV-2 in CSF but only mild albumin cytologic dissociation in the second case: CSF qualitative and quantitative analysis was almost normal (no oligoclonal bands were found). The anti-gangliosides, anti-sulfatide, and myelin-associated glycoprotein (anti-GT1a not tested) were negative for both the cases even if antibodies’ positivity is not mandatory for MFS diagnosis. At brain MRI, no nerve enhancement was detected, after gadolinium injection and thin-layer study of the medulla.
Nevertheless, there was a significant recovery of the neurological symptoms after administration of intravenous immunoglobulin in both patients with amelioration of tongue motility, deglutition, speech articulation, and speed. Difference between the first and the second electromyography in both of them, only 15 days later, was very impressive (see Fig. 2, with a drastic improvement of the activation EMG traces, suggesting a possible previous conduction block. We know that immunotherapy could be used to neutralize the SARS CoV-2 infection and its efficacy would be better if the immune IgG antibodies were collected from patients who had recovered from SARS CoV-2 infection in the surrounding area, in order to increase the chances of neutralizing the virus [16], as immunoglobulin therapy is a first choice therapy in GBS and MFS. The bilateral lesion of the hypoglossal without other brainstem structures involved and the selective damage of the sympathetic nervous system fibers directed to the right eye in the first patient reduce the validity of the neuroinvasiveness theory through receptors such as the immunomodulatory therapy response, because there is no continuity between the anatomical structures involved, suggesting an immuno-mediated COVID-19-related cranial multineuritis (first described case with selective sympathetic involvement).
Cranial mononeuropathy with brachial diparesis, albumin-cytologic dissociation, and areflexia in the second case can suggest an atypical MFS overlap [17].
Conclusion
Considering the high frequency of neurological complications, even after the most critical phase of COVID infection, we suggest to consider SARS CoV-2 infection in all cranial multineuropathy during COVID pandemic period.
An accurate neurological evaluation and neurophysiological study is useful in all COVID patients with prolonged sedation, to differentiate a critical area neuropathy from an inflammatory one arising in the critical area, given the absolutely different therapeutic perspectives.
Taking together our data, we think that an inflammatory etiological hypothesis and a possible attempt at immunoglobulin therapy could be considered in all COVID patients who develop neurological symptoms, even if concerns cranial mononeuropathies or multineuropathies without spontaneous improvement.
References
Paterson RW et al (2020) The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. 8:240–3120. https://doi.org/10.1093/brain/awaa240
Pleasure SJ, Green AJ, Josephson SA (2020) The spectrum of neurologic disease in the severe acute respiratory syndrome voronavirus 2 pandemic infection neurologists move to the frontlines. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2020.1065
Iroegbu JD, Ifenatuoha CW, Ijomone OM (2020) Potential neurological impact of coronaviruses: implications for the novel SARS-CoV-2. Neurol Sci 41:1329–1337. https://doi.org/10.1007/s10072-020-04469-4
Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Liu C, Yang C (2020) Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 30:S0889–1591(20)30357-3. https://doi.org/10.1016/j.bbi.2020.03.031
Yachou Y, Idrissi AE, Belapasov V, Benali SA (2020) Neuroinvasion, neurotropic, and neuroinflammatory events of SARS-CoV-2: understanding the neurological manifestations in COVID-19 patients. Neurol Sci 41:2657–2669. https://doi.org/10.1007/s10072-020-04575-3
Lechien JR, Chiesa-Estomba CM, De Siati DR et al (2020) Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study [published online ahead of print, 2020 Apr 6]. Eur Arch Otorhinolaryngol 1–11. https://doi.org/10.1007/s00405-020-05965-1
Murray RS, Brown B, Brian D, Cabirac GF (1992) Detection of coronavirus RNA and antigen in multiple sclerosis brain. Ann Neurol 31(5):525–533. https://doi.org/10.1002/ana.410310511
Koyuncu OO, Hogue IB, Enquist LW (2013) Virus infections in the nervous system. Cell Host Microbe 13(4):379–393. https://doi.org/10.1016/j.chom.2013.03.010
Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 10:e201127. https://doi.org/10.1001/jamaneurol.2020.1127
Padroni M, Mastrangelo V, Asioli GM, Pavolucci L, Abu-Rumeileh S, Piscaglia MG, Querzani P, Callegarini C (2020) Foschi M Guillain-Barré syndrome following COVID-19: new infection, old complication? J Neurol 267(7):1877–1879. https://doi.org/10.1007/s00415-020-09849-6
Willison HJ, Jacobs BC, van Doorn PA (2016) Guillain-Barré syndrome. Lancet. 388(10045):717–727. https://doi.org/10.1016/S0140-6736(16)00339-1
Zhao H, Shen D, Zhou H, Liu J, Chen S (2020) Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol 19(5):383–384. https://doi.org/10.1016/S1474-4422(20)30109-5
Wakerley BR, Uncini A (2014) Yuki N; GBS Classification Group; GBS Classification Group. Guillain-Barré and Miller Fisher syndromes—new diagnostic classification [published correction appears in Nat Rev Neurol. 2014 Nov;10(11):612]. Nat Rev Neurol 10(9):537–544. https://doi.org/10.1038/nrneurol.2014.138
Guillain G, Kreis B (1937) Sur deux cas de polyradiculo-neurité avec hyperalbuminose du liquid céphalo-rachidiens sans réaction cellulaire. Paris Med 2:224–247
Van Bogaert M, Maere M (1938) Les polyradiculonévrites crâniennes bilatérales avec dissociation albumino cytologique: forms crâniennes des polyradiculonévrites du type Guillain et Barré. J Belge Neurol Psychiat 38:275–281
Jawhara S (2020) Could intravenous immunoglobulin collected from recovered coronavirus patients protect against COVID-19 and strengthen the immune system of new patients? Int J Mol Sci 21(7):2272. Published 2020 Mar 25. https://doi.org/10.3390/ijms21072272
Jung JH, Oh EH, Shin J-H, Kim D-S, Choi S-Y, Choi K-D, Choi J-H (2019) Atypical clinical manifestations of Miller Fisher syndrome. Neurol Sci 40(1):67–73. https://doi.org/10.1007/s10072-018-3580-2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies involving human participants performed by any of the authors.
Consent for publication
Written informed consent was collected from the patient for the inclusion of deidentified clinical data in a scientific publication, in accordance with the Declaration of Helsinki.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
De Gennaro, R., Gastaldo, E., Tamborino, C. et al. Selective cranial multineuritis in severe COVID-19 pneumonia: two cases and literature review. Neurol Sci 42, 1643–1648 (2021). https://doi.org/10.1007/s10072-021-05087-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05087-4