Abstract
Background and aims
Monitoring the quality of acute ischemic stroke (AIS) management is increasingly important since patient outcome could be improved with better access to evidence-based treatments. In this scenario, the aim of our study was to identify thrombolysis rate, reasons for undertreatment, and factors associated with better outcome.
Methods
From January to December 2016, individuals diagnosed with AIS at the Policlinic San Martino Hospital in Genoa, Italy, were prospectively included. Severity of stroke, site of occlusion, rate and time related in-hospital management of systemic thrombolysis, and mechanical thrombectomy were recorded. Safety and clinical outcomes were compared between different subgroups.
Results
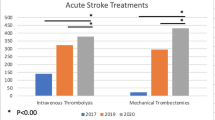
Of 459 AIS patients (57.3% females, mean age 78.1), 111 received i.v. thrombolysis (24.4%) and 50 received mechanical thrombectomy (10.9%). Apart from arrival behind the therapeutic window, which was the first limitation to thrombolysis, the main reason of undertreatment was minor stroke or stroke in rapid improvement. Baseline NIHSS ≥ 8 was associated with unfavorable clinical outcome (mRS > 2) (OR 20.1; 95% CI, 1.1–387.4, p = 0.047). Age older than 80 years (OR 5.0; 95% CI, 1.4–64.1, p = 0.01), baseline NIHSS ≥ 7 (OR 20.1; 95% CI, 1.1–387.4, p = 0.047), and symptomatic intracranial hemorrhage (OR 22.9; 95% CI, 2.0–254.2, p = 0.01) proved independently associated with mortality.
Conclusions
i.v. thrombolysis and mechanical thrombectomy rate was higher than that of previous reports. Minor stroke or stroke in rapid improvement was a major reason for exclusion from thrombolysis of eligible patients. Higher NIHSS proved an independent predictor of unfavorable clinical outcome and death. Strategies to avoid in-hospital delays need to be enforced.

Similar content being viewed by others
References
Donnan GA, Fisher M, Macleod M, Davis SM (2008) Stroke. Lancet 371:1612–1623
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ (2006) Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 367:1747–1757
ISO-SPREAD – Linee Guida Italiane per la prevenzione e cura dell’ictus (2015) Capitolo “Terapia dell’ictus ischemico acuto”. Coordinatore Danilo Toni
Liu Q, Ranta AA, Abernethy G, Barber PA (2017) Trends in New Zealand stroke thrombolysis treatment rate. N Z Med J 130:50–56
McElwaine P, McCormack J, Brennan C, Coetzee H, Cotter P, Doyle R, Hickey A, Horgan F, Loughnane C, Macey C, Marsden P, McCabe D, Mulcahy R, Noone I, Shelley E, Stapleton T, Williams D, Kelly P, Harbison J (2017) Thrombolysis for stroke in Ireland: increasing access and maintaining safety in a challenging environment. Ir J Med Sci 171:661–665
Scherf S, Limburg M, Wimmers R, Middelkoop I, Lingsma H (2016) Increase in national intravenous thrombolysis rates for ischaemic stroke between 2005 and 2012: is bigger better? BMC Neurol 16:53
Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, Albers GW, Kaste M, Marler JR, Hamilton SA, Tilley BC, Davis SM, Donnan GA, Hacke W, ECASS, ATLANTIS, NINDS and EPITHET rt-PA Study Group, Allen K, Mau J, Meier D, del Zoppo G, De Silva DA (2010) Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 375:1695–1603
Saver JL, Smith EE, Fonarow GC, Reeves MJ, Zhao X, Olson DM, Schwamm LH, GWTG-Stroke Steering Committee and Investigators (2010) The “golden hour” and acute brain ischemia: presenting features and lytic therapy in >30,000 patients arriving within 60 minutes of stroke onset. Stroke 41:1431–1439
Barber PA, Zhang J, Demchuk AM, Schlaug G (2001) Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology 56:1015–1020
Eissa A, KrassI LC, Sturm J, Ibrahim R, Bajorek B (2013) Understanding the reasons behind the low utilisation of thrombolysis in stroke. Australas Med J 6:152–167
Reiff T, Michel P (2017) Reasons and evolution of non-thrombolysis. Emerg Med J 34:219–226
Smith EE, Fonarow GC, Reeves MJ, Cox M, Olson DM, Hernandez AF, Schwamm LH (2011) Outcomes in mild or rapidly improving stroke not treated with intravenous recombinant tissue-type plasminogen activator findings from get with the guidelines–stroke. Stroke 42:3110–3115
Laurencin C, Philippeau F, Blanc-Lasserre K, Vallet AE, Cakmak S, Mechtouff L, Cho TH, Ritzenthaler T, Flocard E, Bischoff M, El Khoury C, Nighoghossian N, Derex L (2015) Thrombolysis for acute minor stroke: outcome and barriers to management. Results from the RESUVAL Stroke Network. Cerebrovasc Dis 40:3–9
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, Johnston KC, Johnston SC, Khalessi AA, Kidwell CS, Meschia JF, Ovbiagele B, Yavagal DR, American Heart Association Stroke Council (2015) 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:3020–3035
Kim JT, Park MS, Chang J, Lee JS, Choi KH, Cho KH (2013) Proximal arterial occlusion in acute ischemic stroke with low NIHSS scores should not be considered as mild stroke. PLoS One 8
Haussen DC, Bouslama M, Grossberg JA, Anderson A, Belagage S, Frankel M, Bianchi N, Rebello LC, Nogueira RG (2017) Too good to intervene? Thrombectomy for large vessel occlusion strokes with minimal symptoms: an intention-to-treat analysis. Neurointerv Surg 9:917–921
Adams HP Jr, Davis PH, Leira EC, Chang KC, Bendixen BH, Clarke WR, Woolson RF, Hansen MD (1999) Baseline NIH stroke scale score strongly predicts outcome after stroke: a report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology 53:126–131
Tu HT, Campbell BC, Christensen S, Desmond PM, De Silva DA, Parsons MW, Churilov L, Lansberg MG, Mlynash M, Olivot JM, Straka M, Bammer R, Albers GW, Donnan GA, Davis SM, EPITHET-DEFUSE Investigators (2015) Worse stroke outcome in atrial fibrillation is explained by more severe hypoperfusion, infarct growth, and hemorrhagic transformation. Int J Stroke 10:534–540
Kimura K, Minematsu K, Yamaguchi T, Japan Multicenter Stroke Investigators’ Collaboration (J-MUSIC) (2005) Atrial fibrillation as a predictive factor for severe stroke and early death in 15 831 patients with acute ischaemic stroke. J Neurol Neurosurg Psychiatry 76:679–683
Reutera B, Gumbingerc C, Sauera T, Wiethölter H, Bruder I, Rode S, Ringleb PA, Kern R, Hacke W, Hennerici MG, Stroke Working Group of Baden-Wuerttemberg (2016) Intravenous thrombolysis for acute ischaemic stroke in the elderly: data from the Baden-Wuerttemberg stroke registry. Eur J Neurol 23:13–20
Mishra NK, Diener HC, Lyden PD, Bluhmki E, Lees KR, VISTA Collaborators (2010) Influence of age on outcome from thrombolysis in acute stroke: a controlled comparison in patients from the Virtual International Stroke Trials Archive (VISTA). Stroke 41:2840–2848
IST-3 collaborative group, Sandercock P, Wardlaw JM, Lindley RI, Dennis M, Cohen G, Murray G, Innes K, Venables G, Czlonkowska A, Kobayashi A, Ricci S, Murray V, Berge E, Slot KB, Hankey GJ, Correia M, Peeters A, Matz K, Lyrer P (2012) The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet 379:2352–2363
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M (2015) Endovascular therapy for ischemic stroke with perfusion imaging selection. N Engl J Med 372:1009–1018
Santalucia P, Pezzella FR, Sessa M, Monaco S, Torgano G, Anticoli S, Zanoli E, Maimone Baronello M, Paciaroni M, Caso V, Women Stroke Association (WSA) (2013) Women Stroke Association (WSA). Sex differences in clinical presentation, severity and outcome of stroke: results from a hospital-based registry. Eur J Intern Med 24:167–171
Acknowledgments
We thank Kristi Beshiri, Emanuele Giacheri, Simona Priora, and Angela Zuppa for their assistance in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent was not required.
Rights and permissions
About this article
Cite this article
Bandettini di Poggio, M., Finocchi, C., Brizzo, F. et al. Management of acute ischemic stroke, thrombolysis rate, and predictors of clinical outcome. Neurol Sci 40, 319–326 (2019). https://doi.org/10.1007/s10072-018-3644-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-018-3644-3