Abstract
Background
Manifestations of ischemic stroke vary widely, and serum biomarkers may be useful for stratification of risk of severe stroke. This study evaluated the association of lipoprotein-associated phospholipase A2 (Lp-PLA2) mass and initial severity.
Methods
We employed a retrospective analysis on our hospital-based registry and recruited 488 first-onset ischemic stroke patients admitted within 24 h after onset and with Lp-PLA2 mass measured. Stroke severities evaluated by National Institutes of Health Stroke Scale (NIHSS) were compared between Lp-PLA2 categories dichotomized by median. Multivariate logistic regression was used to detect the independent risk factors of severe stroke (NIHSS ≥ 7) and receiver operator curve (ROC) was constructed to detect the value of addition of Lp-PLA2 to the model of other risk factors for predicting severe stroke.
Results
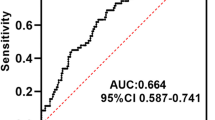
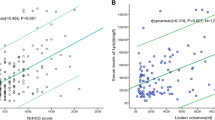
Of the overall patients, the median admission NIHSS scores was 3 and 28.1% had severe manifestation. Admission NIHSS scores were different between patients of Lp-PLA2 above and under the median (median NIHSS 4 vs. 3, P < 0.001). Lp-PLA2 levels was correlated with admission NIHSS (r = 0.268, P < 0.001). Logistic regression showed Lp-PLA2 category (OR 2.37, 95%CI 1.44–3.90, P < 0.001) and levels per 100 ng/ml (OR 1.69, 95%CI 1.35–2.11, P < 0.001) were both independently associated with severe stroke. Addition of Lp-PLA2 category and levels to other independent risk factors both increased the area under curves (from 0.676 to 0.718 with category and 0.734 with levels).
Conclusion
Lp-PLA2 was independently related to admission severity in ischemic stroke patients, implying a potential predictive value of Lp-PLA2 for severe stroke in prevention.

Similar content being viewed by others
References
Adams HP Jr, Davis PH, Leira EC et al (1999) Baseline NIH stroke scale score strongly predicts outcome after stroke: a report of the Trial of Org 10172 in acute stroke treatment (TOAST). Neurology 53:126–131
Phan TG, Clissold B, Ly J, Ma H, Moran C, Srikanth V (2016) Stroke severity and comorbidity index for prediction of mortality after ischemic stroke from the virtual international stroke trials archive-acute collaboration. J Stroke Cerebrovasc Dis 25:835–842
Katz BS, McMullan JT, Sucharew H, Adeoye O, Broderick JP (2015) Design and validation of a prehospital scale to predict stroke severity: Cincinnati Prehospital Stroke Severity Scale. Stroke 46:1508–1512
Gorelick PB (2008) Lipoprotein-associated phospholipase A2 and risk of stroke. Am J Cardiol 101:34f–40f
Esenwa CC, Elkind MS (2016) Inflammatory risk factors, biomarkers and associated therapy in ischaemic stroke. Nat Rev Neurol 12:594–604
Oei HH, van der Meer IM, Hofman A, Koudstaal PJ, Stijnen T, Breteler MM, Witteman JC (2005) Lipoprotein-associated phospholipase A2 activity is associated with risk of coronary heart disease and ischemic stroke: the Rotterdam Study. Circulation 111:570–575
Elkind MS, Tai W, Coates K, Paik MC, Sacco RL (2006) High-sensitivity C-reactive protein, lipoprotein-associated phospholipase A2, and outcome after ischemic stroke. Arch Intern Med 166:2073–2080
Thompson A, Gao P, Orfei L et al (2010) Lipoprotein-associated phospholipase A(2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet (London, England) 375:1536–1544
Stroke--1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke 1989;20:1407–31
Heldner MR, Zubler C, Mattle HP, Schroth G, Weck A, Mono ML, Gralla J, Jung S, el-Koussy M, Ludi R, Yan X, Arnold M, Ozdoba C, Mordasini P, Fischer U (2013) National Institutes of Health stroke scale score and vessel occlusion in 2152 patients with acute ischemic stroke. Stroke 44:1153–1157
Greenland P, O’Malley PG (2005) When is a new prediction marker useful? A consideration of lipoprotein-associated phospholipase A2 and C-reactive protein for stroke risk. Arch Intern Med 165:2454–2456
Delgado P, Chacon P, Penalba A et al (2012) Temporal profile and prognostic value of Lp-PLA2 mass and activity in the acute stroke setting. Atherosclerosis 220:532–536
Kara H, Akinci M, Degirmenci S, Bayir A, Ak A, Nayman A, Unlu A, Akyurek F, Sivri M (2014) High-sensitivity C-reactive protein, lipoprotein-related phospholipase A2, and acute ischemic stroke. Neuropsychiatr Dis Treat 10:1451–1457
Cai A, Zheng D, Qiu R, Mai W, Zhou Y (2013) Lipoprotein-associated phospholipase A2 (Lp-PLA(2)): a novel and promising biomarker for cardiovascular risks assessment. Dis Markers 34:323–331
Liu X, Zhu RX, Tian YL, Li Q, Li L, Deng SM, He ZY (2014) Association of PLA2G7 gene polymorphisms with ischemic stroke in northern Chinese Han population. Clin Biochem 47:404–408
Mannheim D, Herrmann J, Versari D, Gossl M, Meyer FB, McConnell JP, Lerman LO, Lerman A (2008) Enhanced expression of Lp-PLA2 and lysophosphatidylcholine in symptomatic carotid atherosclerotic plaques. Stroke 39:1448–1455
Burchardt P, Zurawski J, Zuchowski B, Kubacki T, Murawa D, Wiktorowicz K, Wysocki H (2013) Low-density lipoprotein, its susceptibility to oxidation and the role of lipoprotein-associated phospholipase A2 and carboxyl ester lipase lipases in atherosclerotic plaque formation. Arch Med Sci 9:151–158
Delgado P, Chacon P, Penalba A et al (2012) Lipoprotein-associated phospholipase a(2) activity is associated with large-artery atherosclerotic etiology and recurrent stroke in TIA patients. Cerebrovasc Dis (Basel, Switzerland) 33:150–158
Elkind MS, Leon V, Moon YP, Paik MC, Sacco RL (2009) High-sensitivity C-reactive protein and lipoprotein-associated phospholipase A2 stability before and after stroke and myocardial infarction. Stroke 40:3233–3237
Persson M, Berglund G, Nelson JJ, Hedblad B (2008) Lp-PLA2 activity and mass are associated with increased incidence of ischemic stroke: a population-based cohort study from Malmo, Sweden. Atherosclerosis 200:191–198
Elkind MS, Tai W, Coates K, Paik MC, Sacco RL (2009) Lipoprotein-associated phospholipase A2 activity and risk of recurrent stroke. Cerebrovasc Dis (Basel, Switzerland) 27:42–50
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, F., Liu, Y., Shi, H. et al. Relation between lipoprotein-associated phospholipase A2 mass and incident ischemic stroke severity. Neurol Sci 39, 1591–1596 (2018). https://doi.org/10.1007/s10072-018-3474-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-018-3474-3