Abstract
Facet tropism and orientation are thought to be associated with lumbar disc herniation (LDH), but the relationship is not well established. Moreover, the effect of facet joint on LDH has not been outlined in young patients. The objective of this study was to investigate the associations of facet joint tropism and orientation with LDH in young patients (18–35 years) by computed tomography (CT). Fifty-three patients with LDH and 129 with neither LDH nor low back pain (18–35 years) were included in this study. The facet joint angles were measured for each facet joint by CT as per the method described by Noren et al. We defined facet tropism as a bilateral angle difference > 5°. Young cases with neither LDH nor low back pain were used as the control group. The results showed that LDH was significantly associated with more coronal facet joint orientation at L1–2 (p = 0.009), L2–3 (p = 0.004), and L3–4 (p = 0.004). No association was established between facet tropism and LDH. This study revealed that facet joint orientation was associated with LDH in young patients (18–35 years); they were more of coronal facing at upper levels. Also, the facet tropism was not associated with LDH.
Similar content being viewed by others
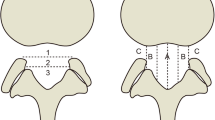
Lumbar disc herniation (LDH) is a common cause of low back pain and lower extremity radicular pain. Facet joint is an important structure in the lumbar spine, which transmits shear forces and helps the intervertebral discs to carry about 16% of the vertical load [1, 2]. Alteration of its orientation and symmetry can potentially alter the biomechanical nature of the lumbar movement. Facet orientation is the angle of the facet joint in the transverse plane relative to the sagittal plane (Fig. 1). Facet tropism is defined as asymmetry between left and right facet joints, wherein one joint has a more sagittal orientation than the other. Farfan et al. [3] first suggested a relationship between facet tropism and the development of LDH, but no final conclusion was made after clinical tests [4,5,6,7,8,9,10,11,12]. The purpose of this study was to investigate associations between LDH and facet tropism and orientation in young patients (aged 18–35 years).
The facet joint angle measurement. The facet line is drawn between the two peaks of each of the superior articular facets (D and E, F and G). The midline is drawn through the center of the lumbar vertebral body (O, AO = OB) and the middle point of the base of the spinous process (C). The angle between the midsagittal line and facet line was measured for each side of the lumbar vertebral body (α = right facet angle, β = left facet angle). The facet joint angle of this level = (α + β) / 2
Methods
This was a retrospective cohort study (evidence level, III). The study was approved by the Medical Ethics Committee of Tianjin First Center Hospital and complied with the Ethical Principles for Medical Research Involving Human Subjects in the World Medical Assembly Declaration of Helsinki.
Fifty-three patients with LDH and 129 cases with neither LDH nor low back pain, aged 18–35 years, were included in this study. LDH was diagnosed by clinical findings (radicular radiating leg pain, radicular radiating leg paresthesia, positive straight leg raising test, one of the following neurological signs: dermatomal hypoesthesia, depressed deep tendon reflexes, and muscle weakness in the distribution of the affected nerve root), by computed tomography (CT) and MRI. Exclusion criteria included patients with scoliosis, spondylolisthesis, transitional vertebra, vertebral fracture, previous surgery, previous trauma/spinal infection, and facet arthropathy. The 129 consecutive cases (aged 18–35 years) with no low back pain were identified and underwent abdominal and pelvic CT for reasons unrelated to lower back pain or LDH at our hospital. The cases whose CT examination showed no LDH were included as controls. Those who had a history of low back pain, sciatica, claudication, or previous problems involving the lower limbs were excluded. Abdominal CT offers excellent resolution for assessment of lumbar pathology; similar methods have been previously used to study spondylolysis [13].
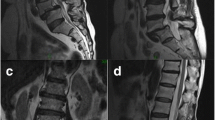
CT was performed on a CT scanner (Siemens, SOMATOM Definition Flash, Germany), with a slice thickness of 3 mm. The orientation of the facet joints was measured on axial CT scans using the method described by Noren et al. [14]. Facet joint angles were measured on the mid-disc cut, which was parallel to the inferior vertebral end-plate of the superior vertebra. A facet line was drawn between the two margins of each of the superior articular facets. The facet joint angle between the facet line and the midsagittal line was measured for each side and recorded as degrees (Fig. 1). The facet joint orientation was defined as the average of the left and the right facet joint angle degrees [(α + β) / 2]. All measurements were performed using bone window CT images by two observers blinded to the patients’ symptoms and the purpose of this study. The average value of the data from the two observers was used for the analysis. For this study, facet tropism was defined as a bilateral angle difference > 5°. Not only the facet joint angle of the herniated level (Fig. 2) and its corresponding level in the controls (Fig. 3) but also the facet joint angle of the no herniated level in LDH patients and its corresponding level in the controls were measured in this study.
CT of imaging of LDH patients. A Sagittal view of the lumbar spine. The lines indicate the location of the cross section. Facet joint angles were measured on the mid-disc cut, which was parallel to the inferior vertebral end-plate of the superior vertebra. B Cross section of L1–2. C Cross section of L2–3. D Cross section of L3–4. E Cross section of L4–5. F Cross section of L5–S1. Overall facet joint angle of this patient: L1–2 = (31.39 + 21.78) / 2 = 26.59°; L2–3 = (32.58 + 37.44) / 2 = 35.01°; L3–4 = (42.31 + 47.67) / 2 = 44.99°; L4–5 = (52.10 + 50.89) / 2 = 51.5°; L5–S1 = (50.51 + 47.82) / 2 = 49.17°. Facet tropism was presented at L1–2 and L3–4 levels. Lumbar disc herniation was presented at L5–S1 level and the disc herniated towards right
CT of cases without LDH and low back pain. A Sagittal view of the lumbar spine. The lines indicate the location of the cross section. B Cross section of L1–2. C Cross section of L2–3. D Cross section of L3–4. E Cross section of L4–5. F Cross section of L5–S1. Overall facet joint angle of this case: L1–2 = (23.52 + 29.63) / 2 = 26.58°; L2–3 = (33.78 + 27.42) / 2 = 30.6°; L3–4 = (34.93 + 35.79) / 2 = 35.36°; L4–5 = (45.04 + 41.18) / 2 = 43.11°; L5–S1 = (57.52 + 48.40) / 2 = 52.96°. Facet tropism was presented at L1–2, L2–3, and L5–S1 levels
Statistical analysis
Independent-samples t test was used to analyze the statistical difference in the degree of facet joint angle between the LDH patients and controls with neither low back pain nor LDH. p < 0.05 was considered to be statistically significant. The Pearson chi-square test was used to analyze the association between facet tropism and LDH, as well as herniated disc direction. The data management software package used was SPSS version 19.0 for Windows.
Results
Fifty-three patients with LDH (62.3% male, 37.7% female) and 129 cases with neither LDH nor low back pain (56.6% male, 43.4% female) were included in this study. The mean age of the LDH patients and controls was 28.22 ± 4.90 and 27.45 ± 5.84 years, respectively. There were 69 disc herniations in 53 LDH patients, which included 7 (10.15%) at L3–4, 25 (36.23%) at L4–5, and 37 (53.62%) at L5–S1. No disc herniation was found at L1–2 and L2–3 in the LDH group. Among these 69 herniated discs, 15 discs herniated towards left, 32 towards right, and 22 towards center.
Mean facet joint orientation was measured as follows (from L1–2 to L5–S1): 23.08° (range 7.28°–43.2°), 26.61° (range 13.63°–45.08°), 33.72° (range 10.82°–57.43°), 42.95° (range 22.96°–57.74°), and 49.18° (range 34.24°–64.62°). Facet joints of the distal lumbar levels were more coronally oriented as compared to those at proximal lumbar levels, which were more sagittally oriented.
LDH was significantly associated with more coronal facet joint orientation at L1–2 (p = 0.009), L2–3 (p = 0.004), and L3–4 (p = 0.004) (Table 1). This means that LDH was associated with more coronally oriented facet joints of upper lumbar levels. There was no significant association between LDH and facet joint orientation at L4–5 (p = 0.110) and L5–S1 (p = 0.673). When the disc herniation affected segments as compared to the controls, there was no statistical difference in L3–L4, L4–L5, and L5–S1 facet joint orientation between the two groups (p > 0.05) (Table 2).
Prevalence of facet tropism was 58.79% in all levels, in which 66.36% was in the controls and 50.72% in the LDH patients at the herniation level. Facet joint tropism occurred on all segments of the lumbar spine, with no significant difference in the incidence of lumbar segments (p > 0.05). There was no significant association between LDH and facet joint tropism (p = 0.153). No significant association was found between the side of disc herniation and the distribution of the more coronal or sagittal facing facet (p = 0.483).
Discussion
With hyaline cartilage overlying subchondral bone, the facet joints are the only synovial joints in the spine, which transmit shear forces and help the intervertebral discs to carry about 16% of the vertical load [1, 2]. The facet joints provide posterior mechanical support, stabilizing the motion segment in flexion and extension and protecting the disc from excessive torsion. The two facet joints at the same level may carry parallel loading in the normal lumbar spine. Alteration of facet joint orientation and symmetry can create an asymmetrical stress distribution in the zygapophysial tissues and intervertebral disc. Facet tropism and orientation have been postulated as factors associated with LDH, but the relationship is not fully established [3,4,5,6,7,8,9,10,11,12]. Some groups considered facet tropism and orientation to be important causes of LDH [3, 4, 14], which was refuted by others [5, 6].
An appropriate control is crucial for a clinical test. The facet joints of low back pain patients, or the adjacent facet joints without disc herniation in LDH patients, were used as a control group in many studies [5, 9, 12, 14, 15]. The biomechanical nature of the lumbar movement of low back pain patients is abnormal and the facet joints of these patients cannot replace a normal facet joint. The facet joint of adjacent segment in LDH patients is a potential cause of LDH for force transmission. Different segments have different roles and motion ranges in lumbar biomechanics, so using the adjacent segment as the control was not rigorous [16]. In our study, young cases with neither LDH nor low back pain were used as controls, which can accurately reflect facet tropism and orientation for herniation of the lumbar disc. The facet joints in the same segment as the herniated level, but not the adjacent segment, in asymptomatic young people were used to compare to corresponding levels in this study, which can achieve more accurate results.
The age of the control group was different from that of the LDH group in most studies, which is another reason for conflicting results. Majority of the studies were conducted in adults over 18 years of age, and, in some cases, even above 80 years. Kalichman et al [17] and Jixing Wang [18] found that with advancing age, the coronal orientation of the lumbar facet joints gradually decreased. So the degenerative changes should be considered when assessing the pathogenesis of LDH in adults. Due to the effect of degeneration, when the young, middle-aged, and elderly patients are grouped together in a study, the proportion of the different age groups will show different results, which will lead to conflicting conclusions. Only 18–35-year-old cases were included in this study, which can minimize the interference caused by degeneration and achieve more accurate results.
Mean facet joint orientation was measured, from L1–2 to L5–S1, as 23.08°, 26.61°, 33.72°, 42.95°, and 49.18°. This study showed a significant steady progression from sagittal towards a more coronal facet joint orientation in a cephalocaudal fashion, which is in line with the findings of Kalichman et al [17].
This study revealed that young patients (aged 18–35 years) with LDH had more coronally oriented facet joints in L1–L2, L2–L3, and L3–L4, but not in L4–L5 and L5–S1. The LDH patients have more coronally oriented facet joints at the upper lumbar spine, which should be attributed to the specific function of facet joints at different lumbar levels: more sagittal orientation in the upper lumbar segments for more flexion and extension as well as resistance against axial rotation, and more coronal orientation in the lower lumbar segments for more axial rotation as well as resistance against flexion and shearing forces [17, 19]. The more coronally orientated facet joints of the upper lumbar spine (L1–L2, L2–L3, and L3–L4) will limit sagittal rotation and restrict the flexion-extension movement of the upper lumbar spine, which will force the facet joint of the lower lumbar spine (L4–5, L5–S1) to share more flexion-extension function. However, the coronal and flat facet joints of the lower lumbar spine offer less resistance to shear intervertebral force because they are not designed to withstand repeated flexion and extension. Consequently, the discs of L4–5 and L5–S1 will bear more shearing force and tend to herniate, which explains why the incidence of disc herniation at L5–S1 and L4–L5 levels is higher than that at upper lumbar levels.
The criteria for determining facet tropism are very varied, although facet tropism means asymmetry of the left and right facet joints. Noren et al. [14] defined facet asymmetry as a bilateral angle difference > 5°. In other biomechanical studies [9, 20], facet asymmetry was defined as a difference in facet joint angles greater than 1°–10°. Yet others [6, 16] defined facet asymmetry as a bilateral angle difference > 1 standard deviation or 2 IE [4, 9]. In this study, facet tropism was defined as bilateral angular asymmetry > 5°. Contrary to several studies, we found no association between facet tropism and disc herniation at all levels. Prevalence of facet tropism was 66.36% in the controls (normal young people) and 58.79% in all levels. Facet joint tropism occurred on all segments of the lumbar spine, with no significant difference in the incidence of lumbar segments. These findings are supported by the findings of Masharawi et al. [21] where facet joint asymmetry was considered a normal characteristic of the thoracolumbar spine. Our results suggest that facet joint tropism is a common pathology of the lumbar spine in 18–35-year-old population.
In this study, no association was found between the side of lateral herniation and the more coronal or sagittal facet joint, which was in line with the findings of Hagg and Wallner [8] and Cassidy [5]. In contrast, Farfan and Sullivan [3] indicated that the side of disc herniation was associated with the side of coronal facing facet joint.
In this study, the LDH was diagnosed by clinical findings, CT and MRI, and most patients underwent these procedures at our hospital. Though MRI has no radiation and few contraindications as compared to CT, very few healthy young people were willing to undergo MRI examination. In contrast, many young patients underwent abdominal and pelvic CT at our hospital for reasons unrelated to LDH or low back pain, for example, abdominal illness. Abdominal CT offers excellent resolution for assessment of lumbar pathology; similar methods have been previously used to study spondylolysis [13]. The 1-year CT data of 129 consecutive young cases was easily obtained. For measuring joint angles, CT is more accurate than MRI because of the interference of cartilage imaging on MRI.
This study had several limitations. The first was the small number of cases. Also, setting up standard facet joint angles from a few measured vertebrae was an overestimation. Future multi-center studies with large sample sizes are necessary for setting up standard facet joint angles of the vertebrae. In a recent systematic review and meta-analysis, which included 17 studies, the facet joint angle of L4–5 ranged from 30° ± 11° to 47.9° ± 4.8° in the normal group, with no association between facet joint angle and LDH [22]. The second was that using adolescents as research subjects can minimize degenerative influence. However, the number of LDH patients under 18 years of age at our hospital was insufficient for this study. Ishihara et al. found that facet tropism was a common radiological feature of LDH in adolescents [20]. D. Y. Lee et al. found that facet tropism did not influence the development of LDH in adolescents or adults [12]. Wang et al. found that facet tropism was associated with LDH in both L4–5 and L5–S1 levels, and irregular alteration of facet orientation in L3–4, L4–5, and L5–S1 levels was associated with LDH in adolescents [23, 24].
In summary, this study showed that young patients with LDH had more coronal facet joints in L1–L2, L2–L3, and L3–L4, but not in L4–L5 and L5–S1. Facet joint tropism is a common pathology of the lumbar spine in 18–35-year-old people and was not associated with LDH. The side of disc herniation was not associated with the more coronal or sagittal facing facet joints. This suggested that the coronal orientation of the facet joints at the upper lumbar in young people was part of the pre-existing morphology of LDH rather than a result of degeneration.
References
Adams MA, Hutton WC (1980) The effect of posture on the role of the apophysial joints in resisting intervertebral compressive forces. J Bone Joint Surg 62(3):358–362
Kalichmanand L, Hunter DJ (2007) Lumbar facet joint osteoarthritis: a review. Semin Arthritis Rheum 37(2):69–80. https://doi.org/10.1016/j.semarthrit.2007.01.007
Farfan HF, Sullivan JD (1967) The relation of facet orientation to intervertebral disc failure. Can J Surg 10:179–185
Cyron BM, Hutton WC (1980) Articular tropism and stability of the lumbar spine. Spine 5(2):168–172. https://doi.org/10.1097/00007632-198003000-00011
Cassidy JD, Loback D, Yong-Hing K, Tchang S (1992) Lumbar facet joint asymmetry. Intervertebral disc herniation. Spine 17(5):570–574. https://doi.org/10.1097/00007632-199205000-00016
Vanharanta H, Floyd T, Ohnmeiss D (1993) The relationship of facet tropism to degenerative disc disease. Spine 18(8):1000–1005. https://doi.org/10.1097/00007632-199306150-00008
Boden SD, Riew KD, Yamaguchi K et al (1996) Orientation of the lumbar facet joints: association with degenerative disc disease. J Bone Joint Surg Am 78(3):403–411. https://doi.org/10.2106/00004623-199603000-00012
Hagg O, Wallner A (1990) Facet joint asymmetry and protrusion of intervertebral disc. Spine 15(5):356–359. https://doi.org/10.1097/00007632-199005000-00003
Karacan I, Aydin T, Sahin Z, Cidem M, Koyuncu H, Aktas I, Uludag M (2004) Facet joint angles in lumbar disc herniation: their relation to anthropometric features. Spine 29(10):1132–1136. https://doi.org/10.1097/00007632-200405150-00016
Van Schaik JPJ, Verbiest H, Van Schanik FDJ (1984) The orientation and shape of the lower lumbar facet joints: a computed tomographic study of their variation in 100 patients with low back pain and a discussion of their possible clinical implications. In: Computed tomography of the spine, pp 495–505
Kunakornsawat S, Ngamlamaidt K, Tungsiripat R, Prasartritha T (2007) The relationship of facet tropism to lumbar disc herniation. J Med Assoc Thail 90(7):1337–1341
Lee DY, Ahn Y, Lee SH (2006) The influence of facet tropism on herniation of the lumbar disc in adolescents and adults. J Bone Joint Surg Br 88:520–523
Belfi LM, Ortiz AO, Katz DS (2006) Computed tomography evaluation of spondylolysis and spondylolisthesis in asymptomatic patients. Spine 31(24):E907–E910. https://doi.org/10.1097/01.brs.0000245947.31473.0a
Noren R, Trafimow J, Andersson GB et al (1991) The role of facet joint tropism and facet joint angle in disc degeneration. Spine 16(5):530–532. https://doi.org/10.1097/00007632-199105000-00008
Manish C, Gaurav S, Shobha SA et al (2013) Association of facet tropism with lumbar disc herniation. Eur Spine J 22(5):1045–1052
Ko HY, Park BK (1997) Facet tropism in lumbar motion segments and its significance in disc herniation. Arch Phys Med Rehabil 78(11):1211–1214. https://doi.org/10.1016/S0003-9993(97)90334-8
Leonid K, Pradeep S, Ali G, Ling L (2009) Facet tropism and orientation: associations with facet joint osteoarthritis and degenerative spondylolisthesis. Spine 34(16):E579–E585
Wang J, Yang X (2009) Age-related changes in the orientation of lumbar facet joints. Spine 34(17):E596–E598. https://doi.org/10.1097/BRS.0b013e3181abbf1e
Cohen Steven P, Raja Srinivasa N (2007) Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology 106(3):591–614. https://doi.org/10.1097/00000542-200703000-00024
Ishihara H, Matsui H, Osada R, Ohshima H, Tsuji H (1997) Facet joint asymmetry as a radiologic feature of lumbar intervertebral disc herniation in children and adolescents. Spine 22(17):2001–2004. https://doi.org/10.1097/00007632-199709010-00012
Masharawi Y, Rothschild B, Salame K, Dar G, Peleg S, Hershkovitz I (2005) Facet tropism and interfacet shape in the thoracolumbar vertebrae: characterization and biomechanical interpretation. Spine 30(11):E281–E292. https://doi.org/10.1097/01.brs.0000164098.00201.8d
Liu Z, Duan Y, Rong X et al (2017) Variation of facet joint orientation and tropism in lumbar degenerative spondylolisthesis and disc herniation at L4-L5: a systematic review and meta-analysis. 161:41–47
Wang H, Zhou Y (2016) Facet tropism: possible role in the pathology of lumbar disc herniation in adolescents. J Neurosurg Pediatr 18(1):111–115. https://doi.org/10.3171/2015.7.PEDS15175
Wang H, Zhang Z, Zhou Y (2016) Irregular alteration of facet orientation in lumbar segments: possible role in pathology of lumbar disc herniation in adolescents. World Neurosurg 86:321–327
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Written informed consent was obtained from all subjects in this study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zhou, Q., Teng, D., Zhang, T. et al. Association of facet tropism and orientation with lumbar disc herniation in young patients. Neurol Sci 39, 841–846 (2018). https://doi.org/10.1007/s10072-018-3270-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-018-3270-0