Abstract
Introduction/objective
There are increasing numbers of children diagnosed with systemic lupus erythematosus (SLE). Given the chronicity of the disease, individuals are confronted with cocktails of medications for an extended period. The present study explores experiences in medication adherence among adolescents with SLE in an acute care hospital.
Method
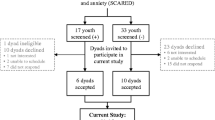
A descriptive qualitative design was employed. Fourteen adolescents with SLE were purposively selected. Face-to-face audio-recorded semi-structured interviews were conducted. Field notes and reflexive journals were maintained, and frequent debriefing sessions were performed to ensure the study’s methodological rigour. Interviews were transcribed verbatim and thematic analyses were used. Constant comparative analysis was used to identify similarities and differences among the participants.
Results
Four themes emerged from interviews: (1) making sense of the treatment; (2) contending with side effects of medications; (3) maintaining networks of support; and (4) creating a new normal. The participants were motivated to adhere to medications when they developed awareness, received social support from family and friends and created routines for new normal when confronted with their diseases. However, some attributed a lack of parental support, poor doctor-patient relationships and the large numbers of medications as deterrence to medication adherence.
Conclusions
This study highlights various medication-taking motivators and deterrents. Interdependent relationships between motivators and deterrents determine medication-taking behaviours. Findings from this multi-ethnic group of individuals of various ages and religious faith across the disease trajectory provide a deep insight into adolescents’ experiences of medication adherence. This can contribute to the development of unique interventions for such individuals.
Key points • Adolescents with systemic lupus erythematosus struggle with conforming to cocktails of medications. • A variety of factors either facilitate or impede their decisions to adhere to medication regimes. • Results suggest that tackling medication adherence among adolescents requires a multi-pronged approach from individual, familial and medical perspectives. |

Similar content being viewed by others
References
Harry O, Yasin S, Brunner H (2018) Childhood-onset systemic lupus erythematosus: a review and update. J Pediatr 196:22–30. https://doi.org/10.1016/j.jpeds.2018.01.045
Fatoye F, Gerbrye T, Svenson LW (2018) Real-world incidence and prevalence of systemic lupus erythematosus in Alberta, Canada. Rheumato Int 38(9):1721–1726. https://doi.org/10.1007/s00296-018-4091-4
Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W (2017) The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatol 56(11):1945–1961. https://doi.org/10.1093/rheumatology/kex260
Tan JHT, Hoh SF, Win MTM, Chan YH, Das L, Arkachaisri T (2015) Childhood-onset systemic lupus erythematosus in Singapore: clinical phenotypes, disease activity, damage, and autoantibody profiles. Lupus 24:998–1005. https://doi.org/10.1177/0961203315584413
Gergianaki I, Bertsias G (2018) Systemic lupus erythematosus in primary care: an update and practical messages for the general practitioner. Front Med 5(161):161. https://doi.org/10.3389/fmed.2018.00161
ACI Musculoskeletal Network. Model of care for the NSW paediatric rheumatology network. Available at: https://www.aci.health.nsw.gov.au/resources/musculoskeletal/paediatric_rheumatology/paediatric-rheumatology-moc Accessed May 22, 2020
McGrady ME, Hommel KA (2013) Medication adherence and health care utilization in pediatric chronic illness: a systematic review. Pediatr 132:730–740. https://doi.org/10.1542/peds.2013-1451
World Health Organisation. Adherence to long-term therapies: evidence for action. Available at: https://www.who.int/chp/knowledge/publications/adherence_full_report.pdf Accessed May 22, 2020
Scalzi LV, Hollenbeak CS, Mascuilli E, Olsen N (2018) Improvement of medication adherence in adolescents and young adults with SLE using web-based education with and without a social media intervention, a pilot study. Pediatr Rheumatol 16(1):18. https://doi.org/10.1186/s12969-018-0232-2
Pramanik B (2014) Diagnosis of systemic lupus erythematosus in an unusual presentation: what a primary care physician should know. Curr Rheumatol Rev 10(2):81–86. https://doi.org/10.2174/1573397111999150128103237
Feldman CH, Yazdany J, Guan H, Solomon DH, Costenbader KH (2015) Medication nonadherence is associated with increased subsequent acute care utilization among medicaid beneficiaries with systemic lupus erythematosus. Arthritis Care Res 67(12):1712–1721. https://doi.org/10.1002/acr.22636
Taddeo D, Egedy M, Frappier JY (2008) Adherence to treatment in adolescents. Paediatr Child Health 13(1):19–24. https://doi.org/10.1093/pch/13.1.19
Levy DM, Kamphuis S (2013) Systemic lupus erythematosus in children and adolescents. Pediatr Clin N Am 59(2):345–364. https://doi.org/10.1016/j.pcl.2012.03.007
Bradshaw C, Atkinson S, Doody O (2017) Employing a qualitative description approach in health care research. Glob Qual Nurs Res 4:1–8. https://doi.org/10.1177/2333393617742282
World Health Organisation. Adolescent health. Available at: http://www.who.int/topics/adolescent_health/en/ Accessed May 22, 2020
Kallio H, Pietila A, Johnson M et al (2016) Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs 72(12):2954–2965. https://doi.org/10.1111/jan.13031
Mulhall A (2003) In the field: notes on observation in qualitative research. J Adv Nurs 41(3):306–313. https://doi.org/10.1046/j.1365-2648.2003.02514.x
Morse JM (1995) The significance of saturation. Sage Publications, Thousand Oaks, CA
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3(2):77–101. https://doi.org/10.1191/1478088706qp063oa
Hewitt-Taylor J (2001) Use of constant comparative analysis in qualitative research. Nurs Stand 15(42):39–42. https://doi.org/10.7748/ns2001.07.15.42.39.c3052
Lincoln YS, Guba EG (1985) Naturalistic inquiry. Sage Publications, Thousand Oaks, CA
Shenton AK (2004) Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf 22(2):63–75
Weckerle CE, Niewold TB (2011) The unexplained female predominance of systemic lupus erythematosus: clues from genetic and cytokine studies. Clin Rev Allergy Immunol 40(1):42–49. https://doi.org/10.1007/s12016-009-8192-4
Singapore Department of Statistics. Population trends, 2018. Available at: https://www.singstat.gov.sg/-/media/files/publications/population/population2018.pdf Accessed May 22, 2020
Hommel KA, Odell S, Sander E, Baldassano RN, Barg FK (2011) Treatment adherence in paediatric inflammatory bowel disease: perceptions from adolescent patients and their families. Health Soc Care Commun 19(1):80–88. https://doi.org/10.1111/j.1365-2524.2010.00951.x
Kumar K, Gordon C, Barry R et al (2011) ‘It’s like taking poison to kill poison but I have to get better’: a qualitative study of beliefs about medicines in rheumatoid arthritis and systemic lupus erythematosus patients of South Asian origin. Lupus 20:837–844. https://doi.org/10.1177/0961203311398512
Dumontheil I (2014) Development of abstract thinking during childhood and adolescence: the role of rostrolateral prefrontal cortex. Dev Cogn Neurosci 10:57–76. https://doi.org/10.1016/j.dcn.2014.07.009
Pratt M, Searles GE (2017) Using visual aids to enhance physician-patient discussions and increase health literacy. J Cutan Med Surg 21(6):497–501. https://doi.org/10.1177/1203475417715208
Flower C, Hambleton I, Campbell M (2016) The effect of psychosocial and neuropsychiatric factors on medication adherence in a cohort of women with systemic lupus erythematosus. J Clin Rheumatol 22(8):411–417. https://doi.org/10.1097/RHU.0000000000000470
Payne ME, Eaton CK, Laura LM et al (2013) Promoting medication adherence and regimen responsibility in two adolescents on hemodialysis for end-stage renal disease: a case study. Clin Case Stud 12(2):95–110. https://doi.org/10.1177/1534650112467079
Rogers RW (1975) A protection motivation theory of fear appeals and attitude change. J Psychol 91:93–114. https://doi.org/10.1080/00223980.1975.9915803
Skinner BF (1938) The behavior of organisms: an experimental analysis. B.F. Skinner Foundation, Cambridge, Massachusetts
Tunnicliffe DJ, Singh-Grewal D, Chaitow J, Mackie F, Manolios N, Lin MW, O’neill SG, Ralph AF, Craig JC, Tong A (2016) Lupus means sacrifice: perspectives of adolescents and young adults with systemic lupus erythematosus. Arthritis Care Res 68(6):828–837. https://doi.org/10.1002/acr.22749
Knight A, Vickery M, Fiks AG, Barg FK (2016) The illness experience of youth with lupus/mixed connective tissue disease: a mixed methods analysis of patient and parent perspectives. Lupus 25(9):1028–1039. https://doi.org/10.1177/0961203316646460
Hale ED, Treharne GJ, Lyons AC, Norton Y, Mole S, Mitton DL, Douglas KM, Erb N, Kitas GD (2006) “Joining the dots” for patients with systemic lupus erythematosus: personal perspectives on health care from a qualitative study. Ann Rheum Dis 65:585–589. https://doi.org/10.1136/ard.2005.037077
El-Rachidi S, LaRochelle JM, Morgan JA (2017) Pharmacists and pediatric medication adherence: bridging the gap. Hosp Pharm 52(2):124–131. https://doi.org/10.1310/hpj5202-124
Lloyd J (2017) ‘You’re not big, you’re just in Asia’: expatriate embodiment and emotional experiences of size in Singapore. Soc Cult Geogr 20(6):806–825. https://doi.org/10.1080/14649365.2017.1384047
Farinha F, Freitas F, Agueda A et al (2017) Concerns of patients with systemic lupus erythematosus and adherence to therapy-a qualitative study. Patient Prefer Adherence 11:1213–1219. https://doi.org/10.2147/PPA.S137544
Tan C (2012) ‘Our shared values’ in Singapore: a Confucian perspective. Educ Theory 62(4):449–463. https://doi.org/10.1111/j.1741-5446.2012.00456.x
Koneru S, Kockarla L, Higgins GC et al (2008) Adherence to medications in systemic lupus erythematosus. J Clin Rheum 14(4):195–201. https://doi.org/10.1097/RHU.0b013e31817a242a
Acknowledgements
The authors thank Dr. Jennie Wong from the Research Support Unit, National University Health System Singapore, for the assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Ethics approval
Ethical approval was obtained from Singhealth Centralised Institutional Review Board (2018/2752).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tan, Q.E.C., Gao, X., Ang, W.H.D. et al. Medication adherence: a qualitative exploration of the experiences of adolescents with systemic lupus erythematosus. Clin Rheumatol 40, 2717–2725 (2021). https://doi.org/10.1007/s10067-021-05583-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05583-0