Abstract
Purpose
Recurrence after laparoscopic inguinal herniorrhaphy is poorly understood. Reports suggest that up to 13% of all inguinal herniorrhaphies worldwide, irrespective of the approach, are repaired for recurrence. We aim to review the risk factors responsible for these recurrences in laparoscopic mesh techniques.
Methods
A search of the Medline, Embase, Science Citation Index, Current Contents and PubMed databases identified English language, peer reviewed articles on the causes of recurrence following laparoscopic mesh inguinal herniorrhaphy published between 1990 and 2018. The search terms included ‘Laparoscopic methods’, ‘Inguinal hernia; Mesh repair’, ‘Recurrence’, ‘Causes’, ‘Humans’.
Results
The literature revealed several contributing risk factors that were responsible for recurrence following laparoscopic mesh inguinal herniorrhaphy. These included modifiable and non-modifiable risk factors related to patient and surgical techniques.
Conclusions
Recurrence can occur at any stage following inguinal hernia surgery. Patients’ risk factors such as higher BMI, smoking, diabetes and postoperative surgical site infections increase the risk of recurrence and can be modified. Amongst the surgical factors, surgeon’s experience, larger mesh with better tissue overlap and careful surgical techniques to reduce the incidence of seroma or hematoma help reduce the recurrence rate. Other factors including type of mesh and fixation of mesh have not shown any difference in the incidence of recurrence. It is hoped that future randomized controlled trials will address some of these issues and initiate preoperative management strategies to modify some of these risk factors to lower the risk of recurrence following laparoscopic inguinal herniorrhaphy.
Similar content being viewed by others
Change history
27 September 2018
In the original publication, affiliation 3 was incorrectly published for the author ‘Darius Ashrafi’. The correct affiliation should read as ‘Department of Surgery, Sunshine Coast University Hospital, Birtinya, QLD, Australia.
References
Jenkins JT, O’Dwyer PJ (2008) Inguinal hernias. Br Med J 336(7638):269–272. https://doi.org/10.1136/bmj.39450.428275.AD
Kehlet H, Bay-Nielsen M, Danish Hernia Database C (2008) Nationwide quality improvement of groin hernia repair from the danish hernia database of 87,840 patients from 1998 to 2005. Hernia 12:1–7. https://doi.org/10.1007/s10029-007-0285-5
Olmi S, Scaini A, Erba L, Guaglio M, Croce E (2007) Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identifies marked differences between prosthesis fixation systems. Surgery 142:40–46
Schwab R, Willms A, Kroger A, Becker HP (2006) Less chronic pain following mesh fixation using a fibrin sealant in TEP inguinal hernia repair. Hernia 10:272–277
Lovisetto F, Zonta S, Rota E, Bottero L, Faillace G, Turra G, Fantini A, Longoni M (2007) Laparoscopic transabdominal preperitoneal (TAPP) hernia repair: surgical phases and complications. Surg Endosc 21:646–652. https://doi.org/10.1007/s00464-006-9031-9
Junge K, Rosch R, Klinge U, Schwab R, Peiper C, Binnebosel M, Schenten F, Schumpelick V (2006) Risk factors related to recurrence in inguinal hernia repair: a retrospective analysis. Hernia 10:309–315
Memon MA, Feliu X, Sallent EF, Camps J, Fitzgibbons RJ Jr (1999) Laparoscopic repair of recurrent hernias. Surg Endosc 13:807–810
El-Dhuwaib Y, Corless D, Emmett C, Deakin M, Slavin J (2013) Laparoscopic versus open repair of inguinal hernia: a longitudinal cohort study. Surg Endosc 27:936–945. https://doi.org/10.1007/s00464-012-2538-3
Scott NW, McCormack K, Graham P, Go PM, Ross SJ, Grant AM (2002) Open mesh versus non-mesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev 4:CD002197. https://doi.org/10.1002/14651858.CD002197
Amato B, Moja L, Panico S, Persico G, Rispoli C, Rocco N, Moschetti I (2012) Shouldice technique versus other open techniques for inguinal hernia repair. Cochrane Database Syst Rev 4:CD001543
Schjøth-Iversen L, Refsum A, Brudvik KW (2017) Factors associated with hernia recurrence after laparoscopic total extraperitoneal repair for inguinal hernia: a 2-year prospective cohort study. Hernia 21:729–735. https://doi.org/10.1007/s10029-017-1634-7
van der Pool AE, Harlaar JJ, den Hoed PT, Weidema WF, van Veen RN (2010) Long-term follow-up evaluation of chronic pain after endoscopic total extraperitoneal repair of primary and recurrent inguinal hernia. Surg Endosc 24:1707–1711. https://doi.org/10.1007/s00464-009-0833-4
Tran H, Tran K, Turingan I, Zajkowska M, Lam V, Hawthorne W (2015) Single-incision laparoscopic inguinal herniorraphy with telescopic extraperitoneal dissection: technical aspects and potential benefits. Hernia 19:407–416. https://doi.org/10.1007/s10029-015-1349-6
Burcharth J, Andresen K, Pommergaard HC, Bisgaard T, Rosenberg J (2014) Direct inguinal hernias and anterior surgical approach are risk factors for female inguinal hernia recurrences. Langenbecks Arch Surg 399:71–76. https://doi.org/10.1007/s00423-013-1124-z
Burcharth J, Pommergaard HC, Bisgaard T, Rosenberg J (2015) Patient-related risk factors for recurrence after inguinal hernia repair: a systematic review and meta-analysis of observational studies. Surg Innov 22:303–317. https://doi.org/10.1177/1553350614552731
Burcharth J, Andresen K, Pommergaard H-C, Rosenberg J (2015) Groin hernia subtypes are associated in patients with bilateral hernias: a 14-year nationwide epidemiologic study. Surg Endosc 29:2019–2026. https://doi.org/10.1007/s00464-014-3905-z
Burcharth J (2014) The epidemiology and risk factors for recurrence after inguinal hernia surgery. Da Med J 61:B4846
Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I (2004) Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 114:1752–1761. https://doi.org/10.1172/JCI21625
Carilli SAA, Emre A (2004) Inguinal cord lipomas. Hernia 8:252–254
Niebuhr HKF (2017) Surgical risk factors for recurrence in inguinal hernia repair—a review of the literature. Innov Surg Sci 2:53–59
de Lange DH, Aufenacker TJ, Roest M, Simmermacher RKJ, Gouma DJ, Simons MP (2005) Inguinal hernia surgery in The Netherlands: a baseline study before the introduction of the Dutch Guidelines. Hernia 9:172–177
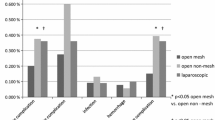
McCormack K, Scott NW, Go PM, Ross S, Grant AM, Collaboration EUHT (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev 1:CD001785
Karthikesalingam A, Markar SR, Holt PJE, Praseedom RK (2010) Meta-analysis of randomized controlled trials comparing laparoscopic with open mesh repair of recurrent inguinal hernia. Br J Surg 97:4–11
Kockerling F, Bittner R, Adolf D, Fortelny R, Niebuhr H, Mayer F, Schug-Pass C (2018) Seroma following transabdominal preperitoneal patch plasty (TAPP): incidence, risk factors, and preventive measures. Surg Endosc 32:2222–2231. https://doi.org/10.1007/s00464-017-5912-3
Sajid MS, Khawaja AH, Sayegh M, Baig MK (2016) A systematic review comparing single-incision versus multi-incision laparoscopic surgery for inguinal hernia repair with mesh. Int J Surg 29:25–35. https://doi.org/10.1016/j.ijsu.2016.02.088
Wakasugi M, Tei M, Akamatsu H (2016) Single-incision totally extraperitoneal inguinal hernia repair after previous inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 26:e149–e152. https://doi.org/10.1097/sle.0000000000000346
Bittner R, Montgomery MA, Arregui E, Bansal V, Bingener J, Bisgaard T, Buhck H, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Grimes KL, Klinge U, Kockerling F, Koeckerling F, Kumar S, Kukleta J, Lomanto D, Misra MC, Morales-Conde S, Reinpold W, Rosenberg J, Singh K, Timoney M, Weyhe D, Chowbey P, International Endohernia S (2015) Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc 29:289–321
Ferzli GS, Rim S, Edwards ED (2013) Combined laparoscopic and open extraperitoneal approach to scrotal hernias. Hernia 17:223–228
Siow SL, Mahendran HA, Hardin M, Chea CH, Nik Azim NA (2013) Laparoscopic transabdominal approach and its modified technique for incarcerated scrotal hernias. Asian J Surg 36:64–68
Lal P, Kajla RK, Chander J, Ramteke VK (2004) Laparoscopic total extraperitoneal (TEP) inguinal hernia repair: overcoming the learning curve. Surg Endosc 18:642–645
Morales-Conde S, Socas M, Fingerhut A (2012) Endoscopic surgeons’ preferences for inguinal hernia repair: TEP, TAPP, or OPEN. Surg Endosc 26:2639–2643
Schrenk P, Woisetschlager R, Rieger R, Wayand W (1996) Prospective randomized trial comparing postoperative pain and return to physical activity after transabdominal preperitoneal, total preperitoneal or Shouldice technique for inguinal hernia repair. Br J Surg 83:1563–1566
Dedemadi G, Sgourakis G, Karaliotas C, Christofides T, Kouraklis G, Karaliotas C (2006) Comparison of laparoscopic and open tension-free repair of recurrent inguinal hernias: a prospective randomized study. Surg Endosc 20:1099–1104
Butler RE, Burke R, Schneider JJ, Brar H, Lucha PA Jr (2007) The economic impact of laparoscopic inguinal hernia repair: results of a double-blinded, prospective, randomized trial. Surg Endosc 21:387–390
Bansal VK, Misra MC, Babu D, Victor J, Kumar S, Sagar R, Rajeshwari S, Krishna A, Rewari V (2013) A prospective, randomized comparison of long-term outcomes: chronic groin pain and quality of life following totally extraperitoneal (TEP) and transabdominal preperitoneal (TAPP) laparoscopic inguinal hernia repair. Surg Endosc 27:2373–2382
Wang W-J, Chen J-Z, Fang Q, Li J-F, Jin P-F, Li Z-T (2013) Comparison of the effects of laparoscopic hernia repair and Lichtenstein tension-free hernia repair. J Laparoendosc Adv Surg Tech A 23(4):301–305
Kockerling F, Bittner R, Jacob DA, Seidelmann L, Keller T, Adolf D, Kraft B, Kuthe A (2015) TEP versus TAPP: comparison of the perioperative outcome in 17,587 patients with a primary unilateral inguinal hernia. Surg Endosc 29:3750–3760. https://doi.org/10.1007/s00464-015-4150-9
Sharma D, Yadav K, Hazrah P, Borgharia S, Lal R, Thomas S (2015) Prospective randomized trial comparing laparoscopic transabdominal preperitoneal (TAPP) and laparoscopic totally extra peritoneal (TEP) approach for bilateral inguinal hernias. Int J Surg 22:110–117. https://doi.org/10.1016/j.ijsu.2015.07.713
McCormack K, Wake BL, Fraser C, Vale L, Perez J, Grant A (2005) Transabdominal pre-peritoneal (TAPP) versus totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair: a systematic review. Hernia 9:109–114. https://doi.org/10.1007/s10029-004-0309-3
Antoniou SA, Antoniou GA, Bartsch DK, Fendrich V, Koch OO, Pointner R, Granderath FA (2013) Transabdominal preperitoneal versus totally extraperitoneal repair of inguinal hernia: a meta-analysis of randomized studies. Am J Surg 206:245–252.e241
Wei FX, Zhang YC, Han W, Zhang YL, Shao Y, Ni R (2015) Transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) for laparoscopic hernia repair: a meta-analysis. Surg Laparosc Endosc Percutan Tech 25:375–383
Chen LS, Chen WC, Kang YN, Wu CC, Tsai LW, Liu MZ (2018) Effects of transabdominal preperitoneal and totally extraperitoneal inguinal hernia repair: an update systematic review and meta-analysis of randomized controlled trials. Surg Endosc. https://doi.org/10.1007/s00464-018-6314-x (Epub ahead of print)
Chan AC, Lee TW, Ng KW, Chung SC, Li AK (1994) Early results of laparoscopic intraperitoneal onlay mesh repair for inguinal hernia. Br J Surg 81:1761–1762
Hatzitheofilou C, Lakhoo M, Sofianos C, Levy RD, Velmahos G, Saadia R (1997) Laparoscopic inguinal hernia repair by an intraperitoneal onlay mesh technique using expanded PTFE: a prospective study. Surg Laparosc Endosc 7:451–455
Olmi S, Scaini A, Erba L, Bertolini A, Croce E (2007) Laparoscopic repair of inguinal hernias using an intraperitoneal onlay mesh technique and a Parietex composite mesh fixed with fibrin glue (Tissucol). Personal technique and preliminary results. Surg Endosc 21:1961–1964. https://doi.org/10.1007/s00464-007-9355-0
Antoniou SA, Garcia-Alamino JM, Hajibandeh S, Hajibandeh S, Weitzendorfer M, Muysoms FE, Granderath FA, Chalkiadakis GE, Emmanuel K, Antoniou GA, Gioumidou M, Iliopoulou-Kosmadaki S, Mathioudaki M, Souliotis K (2018) Single-incision surgery trocar-site hernia: an updated systematic review meta-analysis with trial sequential analysis by the minimally invasive surgery synthesis of interventions outcomes network (MISSION). Surg Endosc 32:14–23. https://doi.org/10.1007/s00464-017-5717-4
Voitk AJ (1998) The learning curve in laparoscopic inguinal hernia repair for the community general surgeon. Can J Surg 41:446–450
Edwards CC 2nd, Bailey RW (2000) Laparoscopic hernia repair: the learning curve. Surg Laparosc Endosc Percutan Tech 10:149–153
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403. https://doi.org/10.1007/s10029-009-0529-7
Bansal VK, Krishna A, Misra MC, Kumar S (2016) Learning curve in laparoscopic inguinal hernia repair: experience at a tertiary care centre. Ind J Surg 78:197–202. https://doi.org/10.1007/s12262-015-1341-5
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E, Kukleta J, Lomanto D, Misra MC, Montgomery A, Morales-Conde S, Reinpold W, Rosenberg J, Sauerland S, Schug-Pass C, Singh K, Timoney M, Weyhe D, Chowbey P (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25:2773–2843
Bokeler U, Schwarz J, Bittner R, Zacheja S, Smaxwil C (2013) Teaching and training in laparoscopic inguinal hernia repair (TAPP): impact of the learning curve on patient outcome. Surg Endosc 27:2886–2893. https://doi.org/10.1007/s00464-013-2849-z
Bracale U, Merola G, Sciuto A, Cavallaro G, Andreuccetti J, Pignata G (2018) Achieving the learning curve in laparoscopic inguinal hernia repair by Tapp: a quality improvement study. J Invest Surg June 14:1–8. https://doi.org/10.1080/08941939.2018.1468944
Schouten N, Simmermacher RK, van Dalen T, Smakman N, Clevers GJ, Davids PH, Verleisdonk EJ, Burgmans JP (2013) Is there an end of the “learning curve” of endoscopic totally extraperitoneal (TEP) hernia repair? Surg Endosc 27:789–794. https://doi.org/10.1007/s00464-012-2512-0
Lamb AD, Robson AJ, Nixon SJ (2006) Recurrence after totally extraperitoneal laparoscopic repair: implications for operative technique and surgical training. Surgeon 4:299–307
HerniaSurg Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Kaafarani HM, Itani KM, Giobbie-Hurder A, Gleysteen JJ, McCarthy M Jr, Gibbs J, Neumayer L (2005) Does surgeon frustration and satisfaction with the operation predict outcomes of open or laparoscopic inguinal hernia repair? J Am Coll Surg 200:677–683. https://doi.org/10.1016/j.jamcollsurg.2004.11.018
Cheatle GL (1921) An Operation for Inguinal Hernia. Br Med J 2:1025–1026
Henry A (1936) Operation for femoral hernia by a midline extraperitoneal approach; with a preliminary note on the use of this route for reducible inguinal hernia. Lancet 1:531–533
Klinge U, Klosterhalfen B, Muller M, Schumpelick V (1999) Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg 165:665–673
Trandafir AF, Popa DE, Vasile D (2017) Prostheses used in laparoscopic inguinal hernia repair: biocompatibility, postoperative complications and quality of life—review of the literature. Maedica (Buchar) 12:202–207
Heikkinen T, Wollert S, Österberg J, Smedberg S, Bringman S (2006) Early results of a randomised trial comparing Prolene and VyproII-mesh in endoscopic extraperitoneal inguinal hernia repair (TEP) of recurrent unilateral hernias. Hernia 10:34–40. https://doi.org/10.1007/s10029-005-0026-6
Bittner R, Leibl BJ, Kraft B, Schwarz J (2011) One-year results of a prospective, randomised clinical trial comparing four meshes in laparoscopic inguinal hernia repair (TAPP). Hernia 15:503–510
Chowbey PK, Garg N, Sharma A, Khullar R, Soni V, Baijal M, Mittal T (2010) Prospective randomized clinical trial comparing lightweight mesh and heavyweight polypropylene mesh in endoscopic totally extraperitoneal groin hernia repair. Surg Endosc 24:3073–3079
Langenbach MR, Schmidt J, Ubrig B, Zirngibl H (2008) Sixty-month follow-up after endoscopic inguinal hernia repair with three types of mesh: a prospective randomized trial. Surg Endosc 22:1790–1797. https://doi.org/10.1007/s00464-008-9863-6
Currie A, Andrew H, Tonsi A, Hurley PR, Taribagil S (2012) Lightweight versus heavyweight mesh in laparoscopic inguinal hernia repair: a meta-analysis. Surg Endosc 26:2126–2133. https://doi.org/10.1007/s00464-012-2179-6
Melkemichel M, Bringman S, Widhe B (2017) Lower recurrence rate with heavyweight mesh compared to lightweight mesh in laparoscopic total extra-peritoneal (TEP) inguinal hernia repair. A nationwide population-based register study. Hernia 21:S162. https://doi.org/10.1007/s10029-017-1595-x
Birk D, Hess S, Garcia-Pardo C (2013) Low recurrence rate and low chronic pain associated with inguinal hernia repair by laparoscopic placement of Parietex ProGrip mesh: clinical outcomes of 220 hernias with mean follow-up at 23 months. Hernia 17:313–320. https://doi.org/10.1007/s10029-013-1053-3
Ozmen J, Choi V, Hepburn K, Hawkins W, Loi K (2015) Laparoscopic totally extraperitoneal groin hernia repair using a self-gripping mesh: clinical results of 235 primary and recurrent groin hernias. J Laparoendosc Adv Surg Tech A 25:915–919
Fumagalli Romario U, Puccetti F, Elmore U, Massaron S, Rosati R (2013) Self-gripping mesh versus staple fixation in laparoscopic inguinal hernia repair: a prospective comparison. Surg Endosc 27:1798–1802
Ferrarese A, Bindi M, Rivelli M, Solej M, Enrico S, Martino V (2016) Self-gripping mesh versus fibrin glue fixation in laparoscopic inguinal hernia repair: a randomized prospective clinical trial in young and elderly patients. Open Med (Wars) 11:497–508
Stoppa R, Petit J, Abourachid H, Henry X, Duclaye C, Monchaux G, Hillebrant JP (1973) Original procedure of groin hernia repair: interposition without fixation of Dacron tulle prosthesis by subperitoneal median approach. Chir 99:119–123
Phillips EH, Rosenthal R, Fallas M, Carroll B, Arregui M, Corbitt J, Fitzgibbons R, Seid A, Schultz L, Toy F et al (1995) Reasons for early recurrence following laparoscopic hernioplasty. Surg Endosc 9:140–144
Kapiris SA, Brough WA, Royston CM, O’Boyle C, Sedman PC (2001) Laparoscopic transabdominal preperitoneal (TAPP) hernia repair. A 7-year two-center experience in 3017 patients. Surg Endosc 15:972–975
Leibl BJ, Schmedt CG, Kraft K, Ulrich M, Bittner R (2000) Recurrence after endoscopic transperitoneal hernia repair (TAPP): causes, reparative techniques, and results of the reoperation. J Am Coll Surg 190:651–655
Garg P, Nair S, Shereef M, Thakur JD, Nain N, Menon GR, Ismail M (2011) Mesh fixation compared to nonfixation in total extraperitoneal inguinal hernia repair: a randomized controlled trial in a rural center in India. Surg Endosc 25:3300–3306. https://doi.org/10.1007/s00464-011-1708-z
Messaris E, Nicastri G, Dudrick SJ (2010) Total extraperitoneal laparoscopic inguinal hernia repair without mesh fixation: prospective study with 1-year follow-up results. Arch Surg 145:334–338
Morrison JE Jr, Jacobs VR (2008) Laparoscopic preperitoneal inguinal hernia repair using preformed polyester mesh without fixation: prospective study with 1-year follow-up results in a rural setting. Surg Laparosc Endosc Percutan Tech 18:33–39. https://doi.org/10.1097/SLE.0b013e318157b155
Liew W, Wai YY, Kosai NR, Gendeh HS (2017) Tackers versus glue mesh fixation: an objective assessment of postoperative acute and chronic pain using inflammatory markers. Hernia 21:549–554
Liem MS, van Duyn EB, van der Graaf Y, van Vroonhoven TJ (2003) Recurrences after conventional anterior and laparoscopic inguinal hernia repair: a randomized comparison. Ann Surg 237:136–141. https://doi.org/10.1097/01.sla.0000041049.69383.0e
Arvidsson D, Smedberg S (2000) Laparoscopic compared with open hernia surgery: complications, recurrences and current trends. Eur J Surg 166(Suppl 585):40–47
Claus CMRG, Campos AC, Bonin EA, Dimbarre D, Loureiro MP, Coelho JC (2016) Prospective, randomized and controlled study of mesh displacement after laparoscopic inguinal repair: fixation versus no fixation of mesh. Surg Endosc 30:1134–1140
Kaul A, Hutfless S, Le H, Hamed SA, Tymitz K, Nguyen H, Marohn MR (2012) Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc 26:1269–1278. https://doi.org/10.1007/s00464-011-2025-2
Lau H (2005) Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitoneal inguinal hernioplasty: a randomized prospective trial. Ann Surg 242:670–675
Topart P, Vandenbroucke F, Lozac’h P (2005) Tisseel versus tack staples as mesh fixation in totally extraperitoneal laparoscopic repair of groin hernias: a retrospective analysis. Surg Endosc 19:724–727
Smith AI, Royston CM, Sedman PC (1999) Stapled and nonstapled laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair. A prospective randomized trial. Surg Endosc 13:804–806
Ferzli GS, Frezza EE, Pecoraro AM Jr, Ahern KD (1999) Prospective randomized study of stapled versus unstapled mesh in a laparoscopic preperitoneal inguinal hernia repair. J Am Coll Surg 188:461–465
Garg P, Rajagopal M, Varghese V, Ismail M (2009) Laparoscopic total extraperitoneal inguinal hernia repair with nonfixation of the mesh for 1,692 hernias. Surg Endosc 23:1241–1245
Teng YJ, Pan SM, Liu YL, Yang KH, Zhang YC, Tian JH, Han JX (2011) A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc 25:2849–2858. https://doi.org/10.1007/s00464-011-1668-3
Sajid MS, Ladwa N, Kalra L, Hutson K, Sains P, Baig MK (2012) A meta-analysis examining the use of tacker fixation versus no-fixation of mesh inlaparoscopic inguinal hernia repair. Int J Surg 10:224–231
Choy C, Shapiro K, Patel S, Graham A, Ferzli G (2004) Investigating a possible cause of mesh migration during totally extraperitoneal (TEP) repair. Surg Endosc 18:523–525
Irving SODG, Sedman PC, Royston CM, Brough WA (1995) Does the mesh move after TAPP hernia repair? An X-ray study. Minim Invasive ther 4:54
Dion YM, Laplante R, Charara J, Marois M (1994) The influence of the number of endoclips and of mesh incorporation on the strength of an experimental hernia patch repair. Surg Endosc 8:1324–1328
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MSS declares no conflict of interest. DA declares no conflict of interest. MAM declares no conflict of interest. BM declares no conflict of interest.
Ethical approval
No ethical approval is required as this is a literature review.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Siddaiah-Subramanya, M., Ashrafi, D., Memon, B. et al. Causes of recurrence in laparoscopic inguinal hernia repair. Hernia 22, 975–986 (2018). https://doi.org/10.1007/s10029-018-1817-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1817-x