Abstract
Introduction
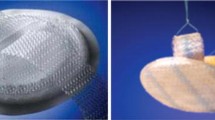
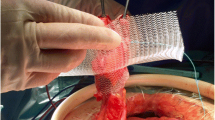
The aim of this study is to compare the integration of two types of prostheses (high and low density, written as HD and LD, respectively) implanted around the stoma to reinforce the abdominal wall to prevent parastomal eventration. The surgical technique used for preperitoneal placement of the prostheses is also described.
Materials and methods
We performed terminal sigmoid colostomies on 16 porcine animals. In 8 of the animals, HD prostheses were placed around the stoma in preperitoneal position, while in the other 8, we implanted wide-pore LD prostheses using the same surgical technique. The following macroscopic variables were then measured: adhesion, extrusion, stenosis, and retraction. A morphological study was also carried out to evaluate the foreign body reaction and the formation of neovascularization and collagen. All animals were killed 3 months after surgery.
Results
Differences were observed with regard to retraction (47 ± 17.8 % for HD vs. 55 ± 19.4 % for LD) and extrusion (50 % for HD vs. 0 % for LD). These differences did not reach statistical significance. There was a great amount of scarring for both types of prostheses, with stomal stenosis being observed in all cases. The number and consistency of intra-abdominal adhesions was low and similar for both types of prostheses. Neither eventration nor necrosis was observed for either type. With regard to the tissue response, we observed both fibrosis and calcification phenomena in the peristomal areas of the LD prostheses. In the HD group, there was both a lower scarring response and a higher foreign body response, with the areas of the prostheses remaining intact.
Conclusions
Both types of prostheses are appropriate for preperitoneal placement in the experimental model used, leading to few intra-abdominal adhesions. Still, due to their integration characteristics, LD prostheses are more appropriate for implanting around the colon since they do not seem to lead to extrusions. When using prostheses, however, it is also essential to consider the important phenomenon of retraction, which is more common with LD mesh.






Similar content being viewed by others
References
Israelsson LA (2008) Parastomal hernias. Surg Clin North Am 88(1):113–125
Devlin HB (1973) Colostomy. Indications, management and complications. Ann R Coll Surg Engl 52(6):392–408
Goligher J (1987) Cirugía del ano, recto y colon. 2nd ed. pp 686–7
Bouillot JL (2002) Traitement chirurgical des complications des colostomies. In: Editions Scientifiques et Médicales Elsevier SAS, editor. Techniques chirurgicales—Appareil digestif. Paris, pp 1–12
LeBlanc KA, Bellanger DE, Whitaker JM, Hausmann MG (2005) Laparoscopic parastomal hernia repair. Hernia 9(2):140–144
Mancini GJ, McClusky DA III, Khaitan L, Goldenberg EA, Heniford BT, Novitsky YW, Park AE, Kavic S, LeBlanc KA, Elieson MJ, Voeller GR, Ramshaw BJ (2007) Laparoscopic parastomal hernia repair using a nonslit mesh technique. Surg Endosc 21(9):1487–1491
Muysoms F (2007) Laparoscopic repair of parastomal hernias with a modified sugarbaker technique. Acta Chir Belg 107(4):476–480
Zacharakis E, Hettige R, Purkayastha S, Aggarwal R, Athanasiou T, Darzi A, Ziprin P (2008) Laparoscopic parastomal hernia repair: a description of the technique and initial results. Surg Innov 15(2):85–89
Serra Aracil X, Bombardo-Junca J, Moreno-Matias J, Darnell A, Mora-Lopez L, Alcantara-Moral M, Ayguavives-Garnica I, Navarro-Soto S (2009) Randomized, controlled, prospective trial of the use of a mesh to prevent parastomal hernia. Ann Surg 249(4):583–587
Janes A, Cengiz Y, Israelsson LA (2004) Randomized clinical trial of the use of a prosthetic mesh to prevent parastomal hernia. Br J Surg 91(3):280–282
Gogenur I, Mortensen J, Harvald T, Rosenberg J, Fischer A (2006) Prevention of parastomal hernia by placement of a polypropylene mesh at the primary operation. Dis Colon Rectum 49(8):1131–1135
Marimuthu K, Vijayasekar C, Ghosh D, Mathew G (2006) Prevention of parastomal hernia using preperitoneal mesh: a prospective observational study. Colorectal Dis 8(8):672–675
Schug-Pass C, Tamme C, Sommerer F, Tannapfel A, Lippert H, Köckerling F (2008) A lightweight, partially absorbable mesh (Ultrapro) for endoscopic hernia repair: experimental biocompatibility results obtained with a porcine model. Surg Endosc 22(4):1100–1106 Epub 2007 Oct 26
Junge K, Klinge U, Rosch R, Klosterhalfen B, Schumperlick V (2002) Functional and morphologic properties of a modified mesh for inguinal hernia repair. World J Surg 26:1472–1480
Böhm G, Binnebösel M, Kräling E, Stanzel S, Anurov M, Titkova S et al (2011) Influence of the elasticity module of synthetic and natural polymeric tissue substitutes on the mobility of the diaphragm and healing process in a rabbit model. J Biomater Appl 25(8):771–793
Seiler C, Baumann P, Kienle P, Kuthe A, Kuhlgatz J, Engemman R, Frankenberg M, Knaebel HP (2010) A randomised, multi-centre, prospective, double blind pilot-study to evaluate safety and efficacy of the non-absorbable Optilene® Mesh Elastic versus the partly absorbable Ultrapro® Mesh for incisional hernia repair. BMC Surg 10:21
Scales JT (1953) Tissue reactions to synthetic materials. Proc R Soc Med 46:647–652
Bellón JM, Bujan J, Contreras LA, Carrera-San Martin A, Jurado F (1996) Comparison of a new type of polytetrafluorethylene patch (mycro mesh) and polypropylene prosthesis (Marlex) for repair of abdominal wall defects. J Am Coll Surg 83:11–18
Demir U, Mihmanli M, Coskun H, Dilege E, Kalyoncu A, Altinli E, Gunduz B, Yilmaz B (2005) Comparison of prosthetic materials in incisional hernia repair. Surg Today 35:223–227
Silvestre AC, De Mathia GB, Fagundes DG, Medeiros LR, Rosa MI (2011) Shrinkage evaluation of heavyweight and lightweight polypropylene meshes in inguinal hernia repair: a randomized controlled trial. Hernia 15:629–634
Bellón JM, Rodriguez M, García- Honduvilla N, Pascual G, Bujan J (2007) Partially absorbable meshes for hernia repair offer advantages over nonabsorbable meshes. Am J Surg 194:68–74
Dirk W, Inge S, Orlin B (2006) Experimental comparison of monofile light and heavy polypropylene meshes: less weight does not mean less. Biol Response 8:1581–1591
Aldridge AJ, Simson JN (2001) Erosion and perforation of colon by synthetic mesh in a recurrent paracolostomy hernia. Hernia 5:110–112
Acknowledgments
This work was supported by grant FISCAM (Foundation for Research in Castilla la Mancha) to create novel research groups. File number. AN/2006/15.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tadeo, G., Picazo, J., Moreno, C. et al. A comparison of two types of preperitoneal mesh prostheses in stoma surgery: application to an animal model. Hernia 16, 669–675 (2012). https://doi.org/10.1007/s10029-012-0966-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-012-0966-6