Abstract
Objectives
The aim of the present study is to provide a detailed macroscopic mapping of the palatal and tuberal blood supply applying anatomical methods and studying specific anastomoses to bridge the gap between basic structural and empirical clinical knowledge.
Materials and methods
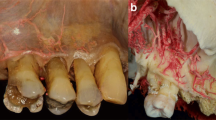
Ten cadavers (three dentate, seven edentulous) have been prepared for this study in the Department of Anatomy, Semmelweis University, Budapest, Hungary, and in the Department of Anatomy of the Medical University of Graz. All cadavers were fixed with Thiel’s solution. For the macroscopic analysis of the blood vessels supplying the palatal mucosa, corrosion casting in four cadavers and latex milk injection in other six cadavers were performed.
Results
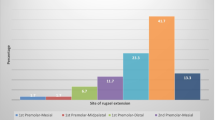
We recorded major- and secondary branches of the greater palatine artery (GPA) and its relation to the palatine spine, different anastomoses with the nasopalatine artery (NPA), and lesser palatal artery (LPA) as well as with contralateral branches of the GPA. Penetrating intraosseous branches at the premolar-canine area were also detected. In edentulous patients, the GPA developed a curvy pathway in the premolar area. The blood supply around the maxillary tuberosity was also presented.
Conclusion
The combination of different staining methods has shed light to findings with relevance to palatal blood supply, offering a powerful tool for the design and execution of surgical interventions involving the hard palate.
Clinical relevance
The present study provides clinicians with a good basis to understand the anatomical background of palatal and tuberal blood supply. This might enable clinicians to design optimized incision- and flap designs. As a result, the risk of intraoperative bleeding and postoperative wound healing complications related to impaired blood supply can be minimized.






Similar content being viewed by others
References
Arnold F, West DC (1991) Angiogenesis in wound healing. Pharmacol Ther 52(3):407–422
Klosek SK, Rungruang T (2009) Anatomical study of the greater palatine artery and related structures of the palatal vault: considerations for palate as the subepithelial connective tissue graft donor site. Surg Radiol Anat 31(4):245–250. https://doi.org/10.1007/s00276-008-0432-4
Fu JH, Hasso DG, Yeh CY, Leong DJ, Chan HL, Wang HL (2011) The accuracy of identifying the greater palatine neurovascular bundle: a cadaver study. J Periodontol 82(7):1000–1006. https://doi.org/10.1902/jop.2011.100619
Yu SK, Lee MH, Park BS, Jeon YH, Chung YY, Kim HJ (2014) Topographical relationship of the greater palatine artery and the palatal spine. Significance for periodontal surgery. J Clin Periodontol 41(9):908–913. https://doi.org/10.1111/jcpe.12288
Langer B, Calagna L (1980) The subepithelial connective tissue graft. J Prosthet Dent 44(4):363–367
Hürzeler MB, Weng D. (1999) A single-incision technique to harvest subepithelial connective tissue grafts from the palate. Int J Periodontics Restorative Dent 19(3):279–87.8)
Benninger B, Andrews K, Carter W (2012) Clinical measurements of hard palate and implications for subepithelial connective tissue grafts with suggestions for palatal nomenclature. J Oral Maxillofac Surg 70(1):149–153. https://doi.org/10.1016/j.joms.2011.03.066
Zuhr O, Bäumer D, Hürzeler M (2014) The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: critical elements in design and execution. J Clin Periodontol Suppl 15:S123–S142. https://doi.org/10.1111/jcpe.12185 Review
Sullivan HC, Atkins JH (1968) Free autogenous gingival grafts. 1. Principles of successful grafting. Periodontics 6(1):5–13
Edel A (1974) Clinical evaluation of free connective tissue grafts used to increase the width of keratinised gingiva. J Clin Periodontol 1(4):185–196
Cortellini P, Pini-Prato G, Tonetti M (1995a) Interproximal free gingival grafts after membrane removal in GTR treatment of infrabony defects. A controlled clinical trial indicating improved outcomes. J Periodontol 66:488–493
Tavelli L, Ravidà A, Saleh MHA, Maska B, Del Amo FS, Rasperini G, Wang HL. (2018) Pain perception following epithelialized gingival graft harvesting: a randomized clinical trial. Clin Oral Investig doi: https://doi.org/10.1007/s00784-018-2455-5
Abrams H, Gossett SE, Morgan WJ (1988) A modified flap design in exposing the palatally impacted canine. ASDC J Dent Child 55(4):285–287
Köşger H, Polat HB, Demirer S, Ozdemir H, Ay S (2009) Periodontal healing of marginal flap versus paramarginal flap in palatally impacted canine surgery: a prospective study. J Oral Maxillofac Surg 67(9):1826–1831. https://doi.org/10.1016/j.joms.2009.04.023
Kleinheinz J, Büchter A, Kruse-Lösler B, Weingart D, Joos U (2005) Incision design in implant dentistry based on vascularization of the mucosa. Clin Oral Implants Res 16(5):518–523
Niu L, Wang J, Yu H, Qiu L (2018) New classification of maxillary sinus contours and its relation to sinus floor elevation surgery. Clin Implant Dent Relat Res. https://doi.org/10.1111/cid.12606
Simion M, Fontana F, Rasperini G, Maiorana C (2004) Long-term evaluation of osseointegrated implants placed in sites augmented with sinus floor elevation associated with vertical ridge augmentation: a retrospective study of 38 consecutive implants with 1- to 7-year follow-up. Int J Periodontics Restorative Dent. 24(3):208–221, 2004
Istvan A. Urban, Sascha A. Jovanovic, Jaime L. Lozada (2017) Vertical ridge augmentation using guided bone regeneration (GBR) in three clinical scenarios prior to implant placement: a retrospective study of 35 patients 12 to 72 months after loading. Biomed Res Int 2017:4042902. doi: https://doi.org/10.1155/2017/4042902., 2017, 1, 11
Buser D, Chappuis V, Kuchler U, Bornstein MM, Wittneben JG, Buser R, Cavusoglu Y, Belser UC (2013) Long-term stability of early implant placement with contour augmentation. J Dent Res 92(12 Suppl):176S–182S. https://doi.org/10.1177/0022034513504949
Reiser GM, Bruno JF, Mahan PE, Larkin LH (1996) The subepithelial connective tissue graft palatal donor site: anatomic considerations for surgeons. Int J Periodontics Restorative Dent. 16(2):130–137
Chrcanovic BR, Custódio AL (2010) Anatomical variation in the position of the greater palatine foramen. J Oral Sci 52(1):109–113
Kim DH, Won SY, Bae JH, Jung UW, Park DS, Kim HJ, Hu KS (2014) Topography of the greater palatine artery and the palatal vault for various types of periodontal plastic surgery. Clin Anat 27(4):578–584. https://doi.org/10.1002/ca.22252
Mörmann W, Ciancio SG (1977) Blood supply of human gingiva following periodontal surgery. A fluorescein angiographic study. J Periodontol 48(11):681–692
Hoke JA, Burkes EJ, White JT, Duffy MB, Klitzman B (1994) Blood-flow mapping of oral tissues by laser Doppler flowmetry. Int J Oral Maxillofac Surg 23(5):312–315
Csempesz F, Vág J, Kerémi B, Györfi A, Fazekas A (2000) Blood flow measurements in human oral tissues with laser Doppler flowmetry. Fogorv Sz 93(4):115–120
Molnár E, Molnár B, Lohinai Z, Tóth Z, Benyó Z, Hricisák L, Windisch P, Vág J (2017) Evaluation of laser speckle contrast imaging for the assessment of oral mucosal blood flow following periodontal plastic surgery: an exploratory study. Biomed Res Int 2017:4042902. doi: https://doi.org/10.1155/2017/4042902, 1, 11.
Alvernia JE, Pradilla G, Mertens P, Lanzino G, Tamargo RJ (2010) Latex injection of cadaver heads: technical note. Neurosurgery 67(2 Suppl Operative):362–7. doi: https://doi.org/10.1227/NEU.0b013e3181f8c247
Verli FD, Rossi-Schneider TR, Schneider FL, Yurgel LS, de Souza MA (2007) Vascular corrosion casting technique steps. Scanning 29(3):128–132
Thiel W (1992b) Eine Arterienmasse zur Nachinjektion bei der konservierung ganzer Leichen. Ann Anat 174:197–200
Thiel W (2002) Ergänzung für die Konservierung ganzer Leichen nach W. Thiel. Ann Anat 184:267–269
Liang X, Jacobs R, Lambrichts I, Vandewalle G (2007) Lingual foramina on the mandibular midline revisited: a macroanatomical study. Clin Anat 20(3):246–251
He P, Truong MK, Adeeb N, Tubbs RS, Iwanaga J (2017) Clinical anatomy and surgical significance of the lingual foramina and their canals. Clin Anat 30(2):194–204. https://doi.org/10.1002/ca.22824.
Robinson RE (1966) The distal wedge operation. Periodontics 4(5):256–264
Acknowledgements
The authors would like to express their gratitude to Dr. Gábor Baksa from the Department of Anatomy, Histology and Embryology, Semmelweis University for his precious support. The authors also would like to thank all other co-workers of the Department of Anatomy, Histology and Embryology, and Dr. Ferenc Bartha and Dr. Dániel Palkovics from the Department of Periodontology, Semmelweis University and the Department of Macroscopical and Clinical Anatomy of Graz University for their work and support.
Funding
The work was supported by the Department of Periodontology, Semmelweis University, Budapest, Hungary; Department of Anatomy, Histology and Embryology, Semmelweis University, Budapest, Hungary; Department of Macroscopical and Clinical Anatomy, Medical University of Graz, Graz, Austria.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shahbazi, A., Grimm, A., Feigl, G. et al. Analysis of blood supply in the hard palate and maxillary tuberosity—clinical implications for flap design and soft tissue graft harvesting (a human cadaver study). Clin Oral Invest 23, 1153–1160 (2019). https://doi.org/10.1007/s00784-018-2538-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2538-3