Abstract
Objectives
This randomized split-mouth clinical trial investigated the influence of implant macrogeometry on bone properties and peri-implant health parameters during the healing process.
Material and methods
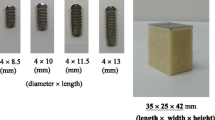
Ninety-nine implants were placed bilaterally in posterior mandibles of 23 patients that received at least four dental implant macrogeometries: standard geometry, Integra (IN) and three geometries inducing “healing chamber”: Duo (D), Compact (C), and Infra (IF). Insertion torque (IT) and implant stability quotient (ISQ) were measured. Peri-implant health were monitored by visible plaque index (VPI), peri-implant inflammation (PI), and presence of calculus (CC). Data were collected during 90 days. Data were assessed for normality using the asymmetry and kurtosis coefficients followed by the Shapiro-Wilk test. A one-way ANOVA was used to investigate differences in IT and linear bone dimensions between the macrogeometry groups. The repeated measurements ANOVA test or ANOVA-R was used for analysis of ISQ, VPI, and PI. Tukey-Kramer test or Student’s t test was used for comparisons between the groups or within each macrogeometry.
Results
Macrogeometry did not significantly influence IT and ISQ values. The minimum ISQ was recorded after 7 days (71.95 ± 12.04, p = 0.0001). Intermediate ISQ was found after 14 days, when the ISQ reached values that are statistically identical to primary stability. The VPI showed significantly higher scores for the D (0.88 ± 1.03) and IN (0.72 ± 0.94) implants after 7 days. The PI was only influenced by the healing time significantly decreasing from 7 (1.07 ± 0.89) to 21 days (0.18 ± 0.18).
Conclusion
Implant macrogeometry did not influence IT nor ISQ values. The relationship between IT and SS was more evident for the Duo implant, but only in the final stage of healing process.
Clinical relevance
Show to the clinician that the macrogeometry and drilling protocols did not interfere in the clinical behavior of the implants during the healing process. However, the IT, primary and secondary stability, is quite dependent of the surgeon experience.





Similar content being viewed by others
References
Coelho PG, Jimbo R, Tovar N, E A B (2015) Osseointegration: hierarchical designing encompassing the macrometer, micrometer, and nanometer length scales. Dent Mater 31:37–52
Leonard G, Coelho P, Polyzois I, Stassen L, Claffey N (2009) A study of the bone healing kinetics of plateau versus screw root design titanium dental implants. Clin Oral Implants Res 20:232–239
Freitas ACJ, Bonfante EA, Giro G et al (2012) The effect of implant design on insertion torque and immediate micromotion. Clin Oral Implants Res 23:113–118
Norton M (2013) Primary stability versus viable constraint—a need to redefine. Int J Oral Maxillofac Implants 28:19–21
Chowdhary R, Halldin A, Jimbo R, Wennerberg A (2015) Influence of micro threads alteration on osseointegration and primary stability of implants: an FEA and in vivo analysis in rabbits. Clin Implant Dent Relat Res 17:562–569
Petrie CS, Williams JL (2005) Comparative evaluation of implant designs: influence of diameter, length, and taper on strains in the alveolar crest. A three-dimensional finite-element analysis Clin Oral Implants Res 16:486–494
Isidor F (2006) Influence of forces on peri-implant bone. Clin Oral Implants Res 17(Suppl 2):8–18
Huang HL, Chang YY, Lin DJ, Li YF, Chen KT, Hsu JT (2011) Initial stability and bone strain evaluation of the immediately loaded dental implant: an in vitro model study. Clin Oral Implants Res 22:691–698
Gottlow J, Barkamo S, Sennerby L (2012) An experimental comparison of two different clinically used implant designs and surfaces. Clin Implant Dent Relat Res 14:204–212
Santamaría-Arrieta G, Brizuela-Velasco A, Fernández-González FJ et al (2016) Biomechanical evaluation of oversized drilling technique on primary implant stability measured by insertion torque and resonance frequency analysis. J Clin Exp Dent 8:e307–e311. https://doi.org/10.4317/jced.52873
Li H, Liang Y, Zheng Q (2015) Meta-analysis of correlations between marginal bone resorption and high insertion torque of dental implants. Int J Oral Maxillofac Implants 30:767–772
Wang T-M, Lee M-S, Wang J-S, Lin L-D (2015) The effect of implant design and bone quality on insertion torque, resonance frequency analysis, and insertion energy during implant placement in low or low- to medium-density bone. Int J Prosthodont 28:40–47
Raghavendra S, Wood MC, Taylor TD et al (2005) Early wound healing around endosseous implants: a review of the literature. Int J Oral Maxillofac Implants 20:425–431
Barone A, Alfonsi F, Derchi G, Tonelli P, Toti P, Marchionni S, Covani U (2016) The effect of insertion torque on the clinical outcome of single implants: a randomized clinical trial. Clin Implant Dent Relat Res 18:588–600
Berglundh T, Abrahamsson I, Lang NP, Lindhe J (2003) De novo alveolar bone formation adjacent to endosseous implants. Clin Oral Implants Res 14:251–262
Lang NP, Salvi GE, Huynh-Ba G, Ivanovski S, Donos N, Bosshardt DD (2011) Early osseointegration to hydrophilic and hydrophobic implant surfaces in humans. Clin Oral Implants Res 22:349–356
Marin C, Granato R, Suzuki M, Gil JN, Janal MN, Coelho PG (2010) Histomorphologic and histomorphometric evaluation of various endosseous implant healing chamber configurations at early implantation times: a study in dogs. Clin Oral Implants Res 21:577–583
Jimbo R, Tovar N, Anchieta RB, Machado LS, Marin C, Teixeira HS, Coelho PG (2014) The combined effects of undersized drilling and implant macrogeometry on bone healing around dental implants: an experimental study. Int J Oral Maxillofac Surg 43:1269–1275
Coelho PG, Jimbo R (2014) Osseointegration of metallic devices: current trends based on implant hardware design. Arch Biochem Biophys 561:99–108
Coelho PG, Suzuki M, Guimaraes MVM, Marin C, Granato R, Gil JN, Miller RJ (2010) Early bone healing around different implant bulk designs and surgical techniques: a study in dogs. Clin Implant Dent Relat Res 12:202–208
Coelho PG, Granato R, Marin C, Teixeira HS, Suzuki M, Valverde GB, Janal MN, Lilin T, Bonfante EA (2011) The effect of different implant macrogeometries and surface treatment in early biomechanical fixation: an experimental study in dogs. J Mech Behav Biomed Mater 4:1974–1981
Jimbo R, Janal MN, Marin C, Giro G, Tovar N, Coelho PG (2014) The effect of implant diameter on osseointegration utilizing simplified drilling protocols. Clin Oral Implants Res 25:1295–1300
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 63:834–840
Waechter J, Madruga M de M, do CFLC et al (2017) Comparison between tapered and cylindrical implants in the posterior regions of the mandible: a prospective, randomized, split-mouth clinical trial focusing on implant stability changes during early healing. Clin Implant Dent Relat Res 19:733–741.
Simons W-F, De Smit M, Duyck J, Coucke W, Quirynen M (2015) The proportion of cancellous bone as predictive factor for early marginal bone loss around implants in the posterior part of the mandible. Clin Oral Implants Res 26:1051–1059
Salvi GE, Lang NP (2004) Diagnostic parameters for monitoring peri-implant conditions. Int J Oral Maxillofac Implants 19(Suppl):116–127
Coelho PG, Suzuki M, Marin C et al (2015) Osseointegration of plateau root form implants: unique healing pathway leading to Haversian-like long-term morphology. Adv Exp Med Biol 881:111–128
Gallucci G, Benic G, Eckert S, Papaspyridakos P, Schimmel M, Schrott A, Weber HP (2014) Consensus statements and clinical recommendations for implant loading protocols. Int J Oral Maxillofac Implants 29:287–290
Menicucci G, Pachie E, Lorenzetti M, Migliaretti G, Carossa S (2012) Comparison of primary stability of straight-walled and tapered implants using an insertion torque device. Int J Prosthodont 25:465–471
Nedir R, Bischof M, Szmukler-Moncler S, Bernard JP, Samson J (2004) Predicting osseointegration by means of implant primary stability: a resonance-frequency analysis study with delayed and immediately loaded ITI SLA implants. Clin Oral Implants Res 15:520–528
Lioubavina-Hack N, Lang NP, Karring T (2006) Significance of primary stability for osseointegration of dental implants. Clin Oral Implants Res 17:244–250
Baltayan S, Pi-Anfruns J, Aghaloo T, Moy PK (2016) The predictive value of resonance frequency analysis measurements in the surgical placement and loading of endosseous implants. J Oral Maxillofac Surg 74:1145–1152
Sennerby L, Meredith N (2008) Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol 2000 47:51–66
Atsumi M, Park S-H, Wang H-L (2007) Methods used to assess implant stability: current status. Int J Oral Maxillofac Implants 22:743–754
Javed F, Ahmed HB, Crespi R, Romanos GE (2013) Role of primary stability for successful osseointegration of dental implants: factors of influence and evaluation. Interv Med Appl Sci 5:162–167
Park J-C, Kim H-D, Kim S-M, Kim MJ, Lee JH (2010) A comparison of implant stability quotients measured using magnetic resonance frequency analysis from two directions: a prospective clinical study during the initial healing period. Clin Oral Implants Res 21:591–597
Koutouzis T, Koutouzis G, Gadalla H, Neiva R (2013) The effect of healing abutment reconnection and disconnection on soft and hard peri-implant tissues: a short-term randomized controlled clinical trial. Int J Oral Maxillofac Implants 28:807–814
Acknowledgements
The authors thank to Signo Vinces Dental Implants Company for supplying the dental implants used in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The research protocol was approved by the Ethics Committee of School of Dentistry (Report no. 1.458.507), Federal University of Pelotas.
Informed consent
The informed consent was obtained from all individual participants included in the study.
Additional information
Carmo Filho LC and Faot F shared first authorship.
Electronic supplementary material
ESM 1
(DOCX 68 kb)
Rights and permissions
About this article
Cite this article
Carmo Filho, L.C., Faot, F., Madruga, M.M. et al. Effect of implant macrogeometry on peri-implant healing outcomes: a randomized clinical trial. Clin Oral Invest 23, 567–575 (2019). https://doi.org/10.1007/s00784-018-2463-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2463-5