Abstract
Objectives
To obtain a systematic and standardized evaluation of the current evidence on development process, metric properties, and administration issues of oral health-related quality of life instruments available for children and adolescents.
Materials and methods
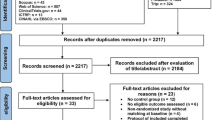
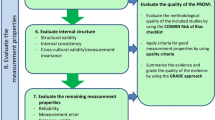
A systematic search until October 2016 was conducted in PubMed, Embase, Lilacs, SciELO, and Cochrane databases. Articles with information regarding the development process, metric properties, and administration issues of pediatric instruments measuring oral health-related quality of life were eligible for inclusion. Two researchers independently evaluated each instrument applying the Evaluating Measures of Patient-Reported Outcomes (EMPRO) tool. An overall and seven attribute-specific EMPRO scores were calculated (range 0–100, worst to best): measurement model, reliability, validity, responsiveness, interpretability, burden, and alternative forms.
Results
We identified 18 instruments evaluated in 132 articles. From five instruments designed for preschoolers, the Early Childhood Oral Health Impact Scale (ECOHIS) obtained the highest overall EMPRO score (82.2). Of nine identified for schoolchildren and adolescents, the best rated instrument was the Child Perceptions Questionnaire 11–14 (82.1). Among the four instruments developed for any age, the Family Impact Scale (FIS) obtained the highest scores (80.3).
Conclusion
The evidence supports the use of the ECOHIS for preschoolers, while the age is a key factor when choosing among the four recommended instruments for schoolchildren and adolescents. Instruments for specific conditions, symptoms, or treatments need further research on metric properties.
Clinical relevance
Our results facilitate decision-making on the correct oral health-related quality of life instrument selection for any certain study purpose and population during the childhood and adolescence life cycle.



Similar content being viewed by others
References
Zaror C, Pineda P, Orellana J (2011) Prevalence of early childhood caries and associated factors in 2 and 4 year-old Chilean children. Int J Odontostomatol 5:171–177
Aldrigui JM, Jabbar NS, Bonecker M, Braga MM, Wanderley MT (2014) Trends and associated factors in prevalence of dental trauma in Latin America and Caribbean: a systematic review and meta-analysis. Community Dent Oral Epidemiol 42:30–42. https://doi.org/10.1111/cdoe.12053
Do LG (2012) Distribution of caries in children: variations between and within populations. J Dent Res 91:536–543. https://doi.org/10.1177/0022034511434355
Kassebaum NJ, Smith AGC, Bernabé E, Fleming TD, Reynolds AE, Vos T, Murray CJL, Marcenes W, GBD 2015 Oral Health Collaborators (2017) Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990–2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res 96:380–387
Abanto J, Carvalho TS, Mendes FM, Wanderley MT, Bonecker M, Raggio DP (2011) Impact of oral diseases and disorders on oral health-related quality of life of preschool children. Community Dent Oral Epidemiol 39:105–114. https://doi.org/10.1111/j.1600-0528.2010.00580.x
Antonarakis GS, Patel RN, Tompson B (2013) Oral health-related quality of life in non-syndromic cleft lip and/or palate patients: a systematic review. Community Dent Health 30:189–195
Bendo CB, Paiva SM, Varni JW, Vale MP (2014) Oral health-related quality of life and traumatic dental injuries in Brazilian adolescents. Community Dent Oral Epidemiol 42:216–223. https://doi.org/10.1111/cdoe.12078
Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM (2016) The impact of malocclusions on oral health-related quality of life in children-a systematic review and meta-analysis. Clin Oral Investig 20:1881–1894. https://doi.org/10.1007/s00784-015-1681-3
Zaror C, Martinez-Zapata MJ, Abarca J, Diaz J, Pardo Y, Pont A, Ferrer M (2018) Impact of traumatic dental injuries on quality of life in preschoolers and schoolchildren: a systematic review and meta-analysis. Community Dent Oral Epidemiol 46:88–101. https://doi.org/10.1111/cdoe.12333
Zhou Y, Wang Y, Wang X, Voliere G, Hu R (2014) The impact of orthodontic treatment on the quality of life a systematic review. BMC Oral Health 14:66. https://doi.org/10.1186/1472-6831-14-66
Sischo L, Broder HL (2011) Oral health-related quality of life: what, why, how, and future implications. J Dent Res 90:1264–1270. https://doi.org/10.1177/0022034511399918
Aaronson N, Alonso J, Burnam A, Lohr KN, Patrick DL, Perrin E, Stein RE (2002) Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res 11:193–205
Valderas JM, Ferrer M, Mendivil J, Garin O, Rajmil L, Herdman M, Alonso J, Scientific Committee on “Patient-Reported Outcomes” of the IRYSS Network (2008) Development of EMPRO: a tool for the standardized assessment of patient-reported outcome measures. Value Health 11:700–708. https://doi.org/10.1111/j.1524-4733.2007.00309.x
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC (2010) The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res 19:539–549. https://doi.org/10.1007/s11136-010-9606-8
Garin O, Herdman M, Vilagut G, Ferrer M, Ribera A, Rajmil L, Valderas JM, Guillemin F, Revicki D, Alonso J (2014) Assessing health-related quality of life in patients with heart failure: a systematic, standardized comparison of available measures. Heart Fail Rev 19:359–367. https://doi.org/10.1007/s10741-013-9394-7
Schmidt S, Ferrer M, Gonzalez M, Gonzalez N, Valderas JM, Alonso J, Escobar A, Vrotsou K, Group E (2014) Evaluation of shoulder-specific patient-reported outcome measures: a systematic and standardized comparison of available evidence. J Shoulder Elb Surg 23:434–444. https://doi.org/10.1016/j.jse.2013.09.029
Schmidt S, Garin O, Pardo Y, Valderas JM, Alonso J, Rebollo P, Rajmil L, Garcia-Forero C, Ferrer M, Group E (2014) Assessing quality of life in patients with prostate cancer: a systematic and standardized comparison of available instruments. Qual Life Res 23:2169–2181. https://doi.org/10.1007/s11136-014-0678-8
Gibbons CJ, Bee PE, Walker L, Price O, Lovell K (2014) Service user- and career-reported measures of involvement in mental health care planning: methodological quality and acceptability to users. Front Psychiatry 5:178. https://doi.org/10.3389/fpsyt.2014.00178
Maratia S, Cedillo S, Rejas J (2016) Assessing health-related quality of life in patients with breast cancer: a systematic and standardized comparison of available instruments using the EMPRO tool. Qual Life Res 25:2467–2480. https://doi.org/10.1007/s11136-016-1284-8
Gilchrist F, Rodd H, Deery C, Marshman Z (2014) Assessment of the quality of measures of child oral health-related quality of life. BMC Oral Health 14:40. https://doi.org/10.1186/1472-6831-14-40
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Higgins JPT, Green S (editors) (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. Available from www.handbook.cochrane.org
Versloot J, Veerkamp JS, Hoogstraten J (2004) Dental Discomfort Questionnaire: predicting toothache in preverbal children. Eur J Paediatr Dent 5:170–173
Pahel BT, Rozier RG, Slade GD (2007) Parental perceptions of children’s oral health: the Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual Life Outcomes 5:6. https://doi.org/10.1186/1477-7525-5-6
Filstrup SL, Briskie D, da Fonseca M, Lawrence L, Wandera A, Inglehart MR (2003) Early childhood caries and quality of life: child and parent perspectives. Pediatr Dent 25:431–440
Mathur VP, Dhillon JK, Logani A, Agarwal R (2014) Development and validation of oral health-related early childhood quality of life tool for North Indian preschool children. Indian J Dent Res 25:559–566. https://doi.org/10.4103/0970-9290.147078
Tsakos G, Blair YI, Yusuf H, Wright W, Watt RG, Macpherson LM (2012) Developing a new self-reported scale of oral health outcomes for 5-year-old children (SOHO-5). Health Qual Life Outcomes 10:62. https://doi.org/10.1186/1477-7525-10-62
Barretto ER, Paiva SM, Pordeus IA, Ferreira e Ferreira E (2011) Validation of a child dental pain questionnaire instrument for the self-reporting of toothache in children. Pediatr Dent 33:228–232
Broder HL, McGrath C, Cisneros GJ (2007) Questionnaire development: face validity and item impact testing of the Child Oral Health Impact Profile. Community Dent Oral Epidemiol 35(Suppl 1):8–19. https://doi.org/10.1111/j.1600-0528.2007.00401.x
Gherunpong S, Tsakos G, Sheiham A (2004) Developing and evaluating an oral health-related quality of life index for children; the CHILD-OIDP. Community Dent Health 21:161–169
Jokovic A, Locker D, Tompson B, Guyatt G (2004) Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Pediatr Dent 26:512–518
Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G (2002) Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res 81:459–463
Fyffe HE, Deery C, Nugent Z, Nuttall NM, Pitts NB (1999) The reliability of two methods of utility assessment in dentistry. Community Dent Health 16:72–79
Mandall NA, Vine S, Hulland R, Worthington HV (2006) The impact of fixed orthodontic appliances on daily life. Community Dent Health 23:69–74
Patel N, Hodges SJ, Hall M, Benson PE, Marshman Z, Cunningham SJ (2016) Development of the malocclusion impact questionnaire (MIQ) to measure the oral health-related quality of life of young people with malocclusion: part 1—qualitative inquiry. J Orthod 43:7–13. https://doi.org/10.1080/14653125.2015.1114712
Akram AJ, Jerreat AS, Woodford J, Sandy JR, Ireland AJ (2011) Development of a condition-specific measure to assess quality of life in patients with hypodontia. Orthod Craniofac Res 14:160–167. https://doi.org/10.1111/j.1601-6343.2011.01517.x
Locker D, Jokovic A, Stephens M, Kenny D, Tompson B, Guyatt G (2002) Family impact of child oral and oro-facial conditions. Community Dent Oral Epidemiol 30:438–448
Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G (2003) Measuring parental perceptions of child oral health-related quality of life. J Public Health Dent 63:67–72
Steele MM, Steele RG, Varni JW (2009) Reliability and validity of the PedsQL oral health scale: measuring the relationship between child oral health and health-related quality of life. Child Health Care 38:228–244. https://doi.org/10.1080/02739610903038818
Huntington NL, Spetter D, Jones JA, Rich SE, Garcia RI, Spiro A 3rd (2011) Development and validation of a measure of pediatric oral health-related quality of life: the POQL. J Public Health Dent 71:185–193
Gomes MC, Pinto-Sarmento TC, Costa EM, Martins CC, Granville-Garcia AF, Paiva SM (2014) Impact of oral health conditions on the quality of life of preschool children and their families: a cross-sectional study. Health Qual Life Outcomes 12:55. https://doi.org/10.1186/1477-7525-12-55
Shin HS, Han DH, Shin MS, Lee HJ, Kim MS, Kim HD (2015) Korean version of child perceptions questionnaire and dental caries among Korean children. PLoS One 10:e0116011. https://doi.org/10.1371/journal.pone.0116011
Marshman Z, Rodd H, Stern M, Mitchell C, Locker D, Jokovic A, Robinson PG (2005) An evaluation of the Child Perceptions Questionnaire in the UK. Community Dent Health 22:151–155
Kumar S, Kroon J, Lalloo R, Johnson NW (2016) Psychometric properties of translation of the child perception questionnaire (CPQ11-14) in Telugu speaking Indian children. PLoS One 11:e0149181. https://doi.org/10.1371/journal.pone.0149181
O’Brien C, Benson PE, Marshman Z (2007) Evaluation of a quality of life measure for children with malocclusion. J Orthod 34:185–193. https://doi.org/10.1179/146531207225022185
O’Brien K, Wright JL, Conboy F, Macfarlane T, Mandall N (2006) The child perception questionnaire is valid for malocclusions in the United Kingdom. Am J Orthod Dentofac Orthop 129:536–540. https://doi.org/10.1016/j.ajodo.2004.10.014
Wogelius P, Gjorup H, Haubek D, Lopez R, Poulsen S (2009) Development of Danish version of child oral-health-related quality of life questionnaires (CPQ8-10 and CPQ11-14). BMC Oral Health 9:11. https://doi.org/10.1186/1472-6831-9-11
Kumar S, Kroon J, Lalloo R, Johnson NW (2016) Validity and reliability of short forms of parental-caregiver perception and family impact scale in a Telugu speaking population of India. Health Qual Life Outcomes 14:34. https://doi.org/10.1186/s12955-016-0433-7
Marshman Z, Rodd H, Stem M, Mitchell C, Robinson PG (2007) Evaluation of the Parental Perceptions Questionnaire, a component of the COHQoL, for use in the UK. Community Dent Health 24(4):198–204
Wallander JL, Schmitt M, Koot HM (2001) Quality of life measurement in children and adolescents: issues, instruments, and applications. J Clin Psychol 57:571–585
Piovesan C, Batista A, Ferreira F, Ardenghi TM (2009) Oral health-related quality of life in children: conceptual issues. Rev Odonto Cienc 24(1):81–85
Abanto J, Tsakos G, Paiva SM, Raggio DP, Celiberti P, Bonecker M (2014) Agreement between children aged 5–6 years and their mothers in rating child oral health-related quality of life. Int J Paediatr Dent 24:373–379. https://doi.org/10.1111/ipd.12081
Barbosa TS, Gaviao MB (2008) Oral health-related quality of life in children: part I. How well do children know themselves? A systematic review. Int J Dent Hyg 6:93–99. https://doi.org/10.1111/j.1601-5037.2007.00276.x
Barbosa TS, Gaviao MB (2008) Oral health-related quality of life in children: part III. Is there agreement between parents in rating their children’s oral health-related quality of life? A systematic review. Int J Dent Hyg 6:108–113. https://doi.org/10.1111/j.1601-5037.2007.00271.x
Theunissen NC, Vogels TG, Koopman HM, Verrips GH, Zwinderman KA, Verloove-Vanhorick SP, Wit JM (1998) The proxy problem: child report versus parent report in health-related quality of life research. Qual Life Res 7:387–397
Reissmann DR, John MT, Sagheri D, Sierwald I (2016) Diagnostic accuracy of parents’ ratings of their child’s oral health-related quality of life. Qual Life Res 26:881–891. https://doi.org/10.1007/s11136-016-1427-y
Lee GH, McGrath C, Yiu CK, King NM (2011) Sensitivity and responsiveness of the Chinese ECOHIS to dental treatment under general anaesthesia. Community Dent Oral Epidemiol 39:372–377. https://doi.org/10.1111/j.1600-0528.2010.00604.x
Locker D, Jokovic A, Clarke M (2004) Assessing the responsiveness of measures of oral health-related quality of life. Community Dent Oral Epidemiol 32:10–18. https://doi.org/10.1111/j.1600-0528.2004.00114.x
Khurana V, Sharma H, Afroz N, Callan A, Medin J (2017) Patient-reported outcomes in multiple sclerosis: a systematic comparison of available measures. Eur J Neurol 24:1099–1107. https://doi.org/10.1111/ene.13339
Sinclair S, Russell LB, Hack TF, Kondejewski J, Sawatzky R (2017) Measuring compassion in healthcare: a comprehensive and critical review. Patient 10:389–405. https://doi.org/10.1007/s40271-016-0209-5
Acknowledgements
We would like to acknowledge Aurea Martin for her help in the English editing process and figure edition of this manuscript.
Funding
Carlos Zaror is a PhD candidate in Methodology of Biomedical Research and Public Health program, Universitat Autònoma de Barcelona, Barcelona, Spain.
Ma. José Martínez is funded by a Miguel Servet research contract from the Instituto de Salud Carlos III and European Social Fund (CP15/00116).
Montse Ferrer is partially funded by the Departament d’Innovació, Universitats i Empresa, Generalitat de Catalunya (2014 SGR 748).
This project was funded by a grant from the Convenio de Desempeño Regional, FRO 1301, Universidad de La Frontera, No. UNT15-0012.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Zaror, C., Pardo, Y., Espinoza-Espinoza, G. et al. Assessing oral health-related quality of life in children and adolescents: a systematic review and standardized comparison of available instruments. Clin Oral Invest 23, 65–79 (2019). https://doi.org/10.1007/s00784-018-2406-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2406-1