Abstract
Objectives
Patients with anorexia nervosa (AN) are primarily at high risk of multiple somatic complications, including oral diseases. In recent years, a number of new molecules that may play a potentially important role in AN progress and prognosis have been identified in saliva, but their exact roles are still poorly understood. Two such group of substances are antioxidants and vaspin. The purpose of this observational, cross-sectional study was to measure both the salivary and serum total antioxidant status (TAS), and vaspin (VASP) concentrations of patients with AN in comparison to an average population.
Material and methods
Ninety subjects participated (30 patients with AN, 60 matched healthy control subjects). A clinical examination was made, and blood and salivary samples were taken during the acute stage of AN (BMI < 15 kg/m2) in the first week of hospitalization. Enzyme immunoassay (ELISA) suitable for measuring VASP and colorimetric assay for TAS were used.
Results
Anorexic patients had significant reductions in salivary flow, TAS, and an elevation in VASP levels in their saliva and serum. Significant correlations between TAS, VASP, salivary flow, and nutritional status were detected.
Conclusion
Determination of TAS and VASP in combined biological material confirmed that saliva might be a reliable non-invasive source of information for potent nutritional biomarkers.
Clinical relevance
Our findings suggest that VASP cannot be excluded, as its increased concentration in saliva is an adaptive mechanism in reduced TAS, one resulting from diminished salivary secretion. It is therefore worth conducting further research aimed at recognizing the role of TAS and VASP in the saliva of underweight patients.
Similar content being viewed by others
Introduction
In recent years, a number of novel molecules that may play a potentially important role in anorexia nervosa (AN) prognosis, such as total antioxidants status (TAS) and vaspin adipokine (VASP), have been identified, but their exact roles are still poorly understood [1,2,3].
Abnormal levels of TAS in the organism (including saliva) may be associated with a surplus production of reactive oxygen (ROS) and nitrogen (RNS) species and at the same time, a deficit in the production of antioxidants. In the clinical context, this can be manifested as a dysfunction in the transmission of cellular signals and as such, an increased threat of the occurrence of complications in respect of various organic systems, among others, cardiovascular. These dysfunctions appear relatively often in the case of AN [4,5,6]. Our previous study indicated a high variability among individuals in the salivary enzymic system, including those enzymes responsible for antioxidative protection [7].
The second molecule that may play a potentially important role in anorexia nervosa (AN) prognosis, vaspin (VASP), is contained and produced in adipose cells and has been detected in serum, saliva, gingival fluid, cerebrospinal fluid, mucous membranes of the stomach, liver, pancreas, hypothalamus and lipid in subcutaneous and visceral tissues [8]. The multilocalization of VASP in the human body is indicative of its role in the regulation of insulin level and food intake [9,10,11]. Just a few studies have focused on VASP status and its variations in AN. In a recent investigation of Oswiecimska et al., higher serum concentrations of VASP were found in patients with AN, compared with healthy controls and a lack of correlation with anthropometric parameters was evaluated [12].
Other studies have revealed that adipokines have an influence on inflammation and immune reactions in the oral cavity [8, 13,14,15,16]. It is suggested that vaspin has a potential role as an inflammatory biomarker of periodontitis. In Bozkurt Dogan et al.’s study (2016), vaspin was shown to be significantly higher in patients with chronic periodontitis than in periodontally healthy groups and decreased after non-surgical therapy [17].
Our previous study on the macroscopic status of oral tissues in the oral cavity of patients with AN has revealed subjective and objective symptoms [18]. The subjective symptoms included a burning sensation of the oral mucosa. An objective analysis of the oral mucosa revealed the following pathological changes: exfoliate cheilitis, pallor of the oral mucosa and skin, atrophic glossitis, white coating of the tongue, linea alba, erythematous spots on the palate, morsicatio buccarum, angular cheilitis, and ulcers of a traumatic etiology. In addition, the pH of unstimulated saliva was lower in the AN group and differed statistically from that in the healthy individuals [18]. According to the obtained findings, disturbances in VASP concentration and TAS may indicate that anorexic patients may produce a high reactivity to inflammatory processes [17, 18].
Therefore, the present study is aimed at assessing the evidence that (1) saliva might be a reliable non-invasive source of TAS and VASP and (2) whether these levels of TAS and VASP are altered in both, serum and saliva, during the acute stage of AN (BMI < 15 kg/m2) in the first week of hospitalization (hypothesis 1). The null hypothesis assumed there are no differences between the groups.
Material and methods
Subjects
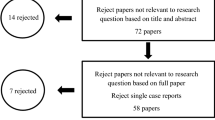
The clinical part of this controlled trial was carried out in the Department of Biomaterials and Experimental Dentistry, Poznan University of Medical Sciences (PUMS), in the years 2014–2016. The TAS and VASP assays were performed in the Division of Biology of Civilization-Linked Diseases, PUMS. All the clinical procedures were performed by a single investigator (EP). The study was conducted according to Good Clinical Practice guidelines and exemplar of the Declaration of Helsinki, after approval by the Bioethics Committee of PUMS. The subject matter and purpose of research were explained to all 90 participants, who gave their informed written consent to participate in the study. The subjects were assigned into two groups: an anorexia (AN) group and two control groups (C-SA, C-SE).
The AN group consisted of 30 girls with a diagnosis of the restrictive subtype of anorexia nervosa, confirmed by two independent psychiatrists from the Department of Child and Adolescent Psychiatry, using the ICD 10 (code F 50.1), DSM - IV (code 307.1) codes [19]. They had similar clinical characteristics (restrictive type) with reference to their menstrual status (secondary amenorrhea). Some of the patients had depressive and obsessive-compulsive symptoms, but fewer than 20% required pharmacotherapy (second and third week of hospitalization later). The participants did not suffer from any other medical disorder. In order to achieve homogeneity among the participants, the bulimic type of anorexia was excluded from the study. Both samples of saliva and blood were collected from 30 anorexic patients. The clinical examination, blood and saliva samples were taken during the acute stage of the symptoms (BMI < 15 kg/m2) within the patients’ first week of hospitalization. The average age in this group was 15.3 ± 1.66 years, with the eating disorders having started 11.5 ± 5.6 months earlier (Table 1).
The control groups consisted of healthy subjects receiving routine dental procedures in the Department of Biomaterials and Experimental Dentistry (PUMS). The recruitment of healthy volunteers in a clinical pediatric context gave them the opportunity to make a choice. Volunteers therefore chose the biological material to be sampled from them and what material to entrust for scientific research. More often than not, non-invasive collection of saliva was chosen by volunteers in this respect.
Finally, unstimulated and stimulated mixed saliva was collected from 30 subjects, the C-SA group and blood samples were taken from 30 subjects, the C-SE group. One serum sample from the C-SE group was invalid and omitted in further analysis. The remainder of the 29 serum samples was frozen at – 80 °C until analysis. All the subjects were matched by age (mean age 15.9 ± 1.6 years) and gender (females only) (Table 1). The criteria for inclusion in the investigation as controls were good general health and no previous history of eating disorders. Exclusion criteria for both groups included systemic diseases and other psychiatric disorders (except for the eating disorder in the AN group), pregnancy, smoking, periodontal inflammation, and the use of any drugs that might affect the secretion of saliva.
Collection of saliva
Factors affecting or biasing the rate of flow and the pH of saliva were avoided as much as possible by carrying out the examination of all the participants at the dental clinic (PUMS) at the same time of year (autumn/winter) and in the morning between 9.00 and 11.00 a.m. to minimize diurnal variation. Data and samples were collected by the same dentist (EP). In preparation for the collection of saliva, each participant was informed that she should refrain from eating and drinking and regular oral hygiene procedures for at least 60 min before the tests. Saliva was collected under unstimulated and stimulated conditions: at rest for 15 min and then stimulated by chewing paraffin tablets (CRT Paraffin, Ivoclar Vivadent, Liechtenstein) for 5 min [20, 21]. Directly after collecting samples, in order to separate impurities and squamous cells of the oral mucosa, the material was centrifuged at 4000 rpm for 10 min at room temperature. The salivary samples were frozen at − 80 °C until analysis. Analysis of the saliva was carried out blind.
Collection of blood
All the blood samples were collected in tubes without anticoagulant by venipuncture between 8.00 and 9.00 a.m. To obtain serum, these whole blood samples were allowed to coagulate at room temperature (RT) for 30 min and then centrifuged at RT for 15 min at 1000 rpm. The collected serum samples and saliva samples were stored in polypropylene tubes at − 80 °C for further analysis.
TAS measurements
Determining total antioxidant status (TAS) in serum/saliva provides an index of the sum of the activities of all antioxidants. Serum from peripheral blood and saliva after fasting were analyzed with the use of the TAS Randox®kit (Cat No. NX2332, Randox Laboratories, Ltd., Crumlin, UK), according to the manufacturer’s protocol. The TAS Randox®kit - enzymatic method with reagents and calibrator control allows measurement of the total amount of antioxidants in serum/saliva by inhibition of the transformation of 2.2-azino-di-[3-ethylbenzthiazoline sulfonate] (ABTS) into the radical cation (ABTS+) in the presence of a peroxidase (metmyoglobin) and H2O2. This cation has a fairly stable blue-green color which can be measured at 600 nm. Results were expressed in millimoles per liter of Trolox equivalents. The linearity of calibration extends to 2.5 mmol/L of Trolox. Intra-assay coefficients of variation and inter-assay coefficients of variation amounted to 4 and 8%, respectively.
VASP measurements
The measurement of vaspin concentrations in serum from peripheral blood and in saliva after fasting was conducted using the certified immunoenzymatic ELISA Kit (Mediagnost, Reutlingen, Germany) and a plate reader (MR-96, Clindiag Systems B.V.B.A., Pollare, Belgium), according to the manufacturer’s protocols. In the research, ready, standardized, and certified test sets have been used (prepared by Mediagnost, Reutlingen, Germany). For their preparation in both cases, purified rabbit IgG of I antibody 5 μg/mL and II antibody 1 μg/mL have been applied. Microtiter plates with the bound primary antibody (specific for the being examined protein) were incubated with serum/saliva (containing the antigen) and, then with the secondary antibody, labeled with peroxidase. This was followed by a reaction with peroxidase substrate and a readout of absorbance at 450 nm. Concentrations of vaspin were calculated according to standard curves estimated from a 4-parameter algorithm (SigmaPlot 11.00 software). Intra-assay coefficients of variation and inter-assay coefficients of variation amounted to 3.5 and 6%, respectively.
Thresholds for TAS in the case of undiluted samples were values between 0.01 and 2.5 mmol/L and for vaspin, under or equal to 4 pg/mL.
Nutritional status
The total time of illness (TTI, months) was determined. Some indices of body weight were also calculated, i.e., the body mass index (BMI) as a ratio of body weight [kg] to [height]2 and the percentage of ideal body weight (%IBW) as a ratio of actual to ideal body weight (IBW) × 100%, where IBW (kg) = height (cm) − 100 − {[(height (cm) − 150)]/2} according to Lorentz’s formula [22].
Statistical analysis
The normality of distribution of quantitative variables was checked with the Shapiro-Wilk test. The statistical evaluation of differences between the groups was performed by means of the Student’s t test, for normally distributed variables and the non-parametric Mann-Whitney test was used when the distributions were significantly different from normal. Associations between quantitative variables were characterized by the Pearson correlation coefficient (for parametric data distribution) and Spearman’s rank correlation coefficient (for non-parametric data distribution). Statistica 12 software (TULSA, OK, USA) with Medical Bundle (the receiver operating characteristics curve—ROC curves) was used for statistical calculations. The results are presented as the means, medians (interquartile range), and SD (standard deviation). The level of statistical significance was set at p = 0.05.
Results
All the details of socio-demographic data, height, weight, salivary flow rate, TAS, and VASP are given in Table 1. No significant differences were found for age between any of the groups. Participants in the AN group were 37% lighter in weight than those in the healthy control group (p = 0.001).
The most relevant finding of the present study is the tendency for a reduction in TAS levels and an elevation in VASP levels detected in the saliva and serum of anorexic patients, compared with those in the control groups (p = 0.012, p = 0.012 for salivary TAS, VASP and p = 0.020, p = 0.049 for serum TAS, VASP respectively) (Table 1). The TAS and VASP concentrations were lower in all the salivary samples than in the serum samples in both anorexic (p = 0.008; p = 0.006) and control groups (p = 0.0001) respectively (Table 1). In addition, there was a statistically significant positive relationship between serum TAS and TAS in saliva (r = 0.3681; p = 0.030).
In the AN group, a significant positive correlation between TAS and the unstimulated flow rate was obtained (r = 0.29; p = 0.024). In the AN group, the salivary VASP level increased with a reduction in the salivary flow (r = − 0.43; p = 0.010). In the AN group, a significant negative correlation between the salivary VASP level and the stimulated flow rate (r = − 0.43; p = 0.010) and a positive correlation between the serum VASP level and IBW% were detected (r = 0.34, p = 0.049).
In the control groups, significant negative correlations between TAS and both BMI (r = − 0.39; p = 0.020) and weight (r = − 0.42; p = 0.020) were detected. In this group, salivary TAS and VASP levels showed a positive correlation with the stimulated flow rate of saliva (r = 0.38; p = 0.040 and r = 0.45; p = 0.010).
The mean values (± standard deviation) for the receiver operating characteristics curve (ROC) in the case of salivary TAS level were higher (0.6328 ± 0.0727) compared to those for the serum TAS level (0.5828 ± 0.0760). The mean value (± the standard deviation) for the ROC curve in the case of salivary VASP concentration (0.6194 ± 0.0735) was higher compared to those for the serum VASP concentration (0.5425 ± 0.0768). In the case of the saliva, cutoff value for TAS was 0.75 mmol/L, for VASP was 0.7 ng/mL (for details, see Fig. 1a, b).
a Receiver operating characteristics curve (ROC) comparison for salivary VASP concentration (broken black line) and salivary TAS level (continuous black line) with baseline (fine gray line) in the entire examined salivary samples, for the AN and control groups (n = 59). b Receiver operating characteristics curve (ROC) comparison for serum VASP concentration (broken black line) and serum TAS level (continuous black line) with baseline (fine gray line) in the entire examined serum samples, for the AN and control groups (n = 59). The values of sensitivity, specificity, and area of characteristic AUC (mean ± SD) for salivary TAS were 60%, 88%, and 0.633 ± 0.072, respectively. In the case of salivary VASP, these values amounted to 58%, 70%, and 0.620 ± 0.073. The sensitivity, specificity, and area of characteristic AUC (mean ± SD) values for serum TAS amounted to 37%, 90%, and 0.583 ± 0.075, respectively. In the case of serum VASP, these values amounted to 38%, 80%, and 0.542 ± 0.075
Discussion
For the first time, this study investigated the concentration of TAS and VASP in the saliva of patients suffering from anorexia nervosa, in comparison to that of the healthy control group. The most relevant finding of the present study is the reduced TAS and increased VASP levels detected in the saliva and serum of anorexic patients. In addition, we have demonstrated that the level of TAS is associated with a low salivary flow rate.
A distinct TAS reduction in serum of AN patients was already reported [23, 24]. This is also reflected in measurements of single antioxidant markers such as albumin, apolipoprotein B, and uric acid [23, 25,26,27,28]. Diminished uric acid level was also observed in extended period of time after re-alimentation [29]. The complexity of oxidational and anti-oxidational processes appearing in patients with a restrictive type of anorexia nervosa should therefore be stressed [30,31,32,33,34]. Metabolic dysfunctions, among others, in respect to the production of carbohydrates and often an intensive bout of physical exercise, are conducive to the production of significant amounts of free radicals, which in the context of a depletion of antioxidants in the system (among others tied to a low supply in the diet) can generate oxidational stress and its ensuing complications [35]. In the clinical context, this can manifest as dysfunctions in the transmission of cellular signals, which in turn can lead to the threat of complications occurring in various systems such as cardiovascular, oral, and periodontal tissues, which occur relatively often in AN [18, 36,37,38,39].
Reduced salivary flow rate has previously been associated with AN [2, 7, 40,41,42,43]. This mechanism in AN is unclear but might be partly mediated by starvation [44, 45]. Further explanations relate to dehydration, reduced salivary gland output, malabsorption, anemia, and hormonal disorders [40, 46, 47]. However, we should consider also the central mechanism of salivary gland activity. Any alterations in the hypothalamic-pituitary-adrenal (HPA) axis and neuroendocrine regulation may impact on salivation. One novel hypothesis of the pathogenesis of AN is the possible role of mental stress in hyperactivity of both the autonomic part of the nervous system (ANS) and of the HPA axis [43, 48,49,50,51].
Another finding of our study is the elevation of VASP levels in the saliva and serum of AN patients, compared with those in the control groups. Although the salivary VASP level was lower than in the serum samples, the results indicated a raised concentration in AN patients. Moreover, a negative correlation between the concentration of salivary VASP and flow rate has been observed. To the best of our knowledge, this is the first report on salivary VASP concentrations in girls with AN. In other publications, elevated VASP was confirmed only in serum samples [12].
The research relevance of our investigation has been shown to be the exploration of the new adipokine—discovered only in the recent past—in both biological materials, serum, and saliva, in the restrictive type of AN.
In general, it should be emphasized that vaspin is a new adipokine and in the data concerning vaspin and AN, exists to a low degree. Vaspin belongs to the family of antiorexigenic molecules and its mechanism of activity in laboratory animals (mice) was dependent on serpin activity and related to the level of leptin [52], which becomes lower in persons with AN. Consequently, it is argued that vaspin activity can lead to high insulin sensitivity and consequently decreases food intake in the case of the acute stage of AN [12, 27, 53].
In contrast to the above investigations, a low VASP level was detected in serum of underweight children due to loss of appetite [3]. However, in AN, we are dealing not with loss of appetite but the voluntary and unpredictable restriction in food intake. These observations and our own results suggest that the mechanism of elevated VASP levels may contribute to an individual’s adaptation to a condition of undernutrition [12, 54, 55]. Therefore, a simple examination of saliva might be one non-invasive method of nutritional assessment in patients with AN.
The recent findings that provide evidence of a causal link between vaspin and anti-inflammatory effect were published by Qi et al. in 2017 [56]. These studies have confirmed that the use of vaspin in cell culture of human pulmonary microvascular endothelial cells (HPMECs) and stimulated lipopolysaccharide (LPS) exerts an inhibitory effect on both levels of proinflammatory interleukins (IL-6, IL-10) and tumor necrosis factor (TNF-α) as well as activation of nuclear factor-κB (NF-κB) (a pleiotropic factor which stimulates proinflammatory action) [56].
Additionally, VASP inhibits the release of other proinflammatory adipokines such as leptin and resistin [57].
The mechanism of action of VASP is related, among others, to inhibiting the formation of free radicals under the influence of LPS (research on HPMECs) [56] or methylglyoxal research on vascular smooth muscle cells [58].
In respect to the association of saliva and AN, there is a lack of direct research evaluating the influence of the former on the homeostasis of the oral cavity. Some investigations have suggested that VASP has a potential role as an inflammatory biomarker of chronic periodontitis and can be altered after non-surgical treatment in the oral cavity [17]. Regarding oral cavity and vaspin, in three studies in which gingival crevicular fluid (GCF) concentrations were determined in patients with moderate severity of periodontitis, higher levels of this protein were found relative to the reference groups [15, 17, 59]. In the analyzes carried out by Pradeep et al. in 2015, similar relationships were also found in the concentrations of this protein in the tear fluid [15]. In addition, the levels of vaspin were correlated positively with the clinical signs of the advanced periodontal disease, i.e., with clinical attachment level (CAL) and gingival index (GI) [15, 59]. In one of them, positive correlations between the level of VASP and the number of deep pockets were also found [59]. The degree of advancement of periodontitis in studies of Balli et al. (2016) has been described in relation to clinical signs of inflammation as a red color and the swelling of the gingival margin, and GI greater than 2, CAL greater than 5 mm, and bone loss affecting 30% of the existing teeth [59].
Collectively, the above investigations have suggested that VASP has a potential role as an anti-inflammatory, anti-apoptotic, and antioxidant biomarker of chronic periodontitis and can be altered after non-surgical treatment in the oral cavity [17, 56].
Because of the paucity of data relating to patients with an extremely low body mass, we can only speculate that VASP could play an inhibitory role on the antioxidant status in the acute stage of AN. Phalitakul et al. reported that VASP produces antioxidative effects and influences inflammatory signal transduction [58, 60]. One explanation lies in the localization of VASP in a wide number of tissues, including the mucous membrane of the gastrointestinal tract and the hypothalamus. This might suggest possible central VASP administration connected with the cognitive regulation of eating behavior [9].
Unfortunately, VASP regulation remains still poorly understood and needs further research.
Limitations of the study
We have identified several potential limitations to our observation. Firstly, the research was conducted on a numerically medium-sized cohort in respect to pediatric individuals among patients with anorexia nervosa. For the purposes of validating research results, one should consider broadening the investigation with a larger study cohort, which in the case of patients at this stage of their illness, especially among adolescents, is no easy matter.
Secondly, the salivary samples were mostly taken between 9.00 and 11.00 but not strictly at the same time. While unlikely, this might influence the secretion rate, due to the circadian rhythm of salivary flow rate [44]. Considering the marked difference in the mean value of salivary flow rate between groups, the lower flow rate of whole saliva in anorexic subjects presumably reflects a true difference, probably induced by malnutrition rather than difference in sampling time. However, clinical studies, using standardized saliva collection procedures, including point of time, are needed to confirm the observation of reduced salivary flow rate in subjects with AN.
The third limitation in this study is its cross-sectional design; longitudinal studies would be necessary to verify the fact that anorexic status negatively affects the salivary flow rate.
The fourth limitation is that body composition was not analyzed. We did not perform these measurements because there is some evidence that bioimpedance (BIA), the most common and cost-effective method of assessing body composition has little utility in AN patients [45]. In this context, future research should take also into account a control sub-group, where the saliva and serum sample is taken at the same time from the same people, which is no easy matter in the adolescent population. However, it shall be argued that the above described potential limitations do not render our results invalid.
Conclusion
The present results demonstrated for the first time the detection and measurement of TAS and vaspin in saliva. The investigation confirmed that the levels of TAS and VASP are altered in both serum and saliva during the acute stage of AN (BMI < 15 kg/m2) (hypothesis 1). The results also indicated that girls with AN have lower TAS and increased vaspin concentrations. Therefore, the null hypothesis was rejected. In addition, we identified associations between anorexia nervosa, low salivary flow rate, and total antioxidant status (under 0.75 mmol/L) and enhanced vaspin level (above 0.34 ng/mL).
The determination of total antioxidant status (TAS) and vaspin (VASP) in combined biological material (serum and saliva) confirmed that saliva might be a reliable non-invasive source of information for potent nutritional biomarkers. Our findings suggest that the increase in VASP plays a role in adaptive mechanisms in reduced TAS one resulting from diminished salivary secretion. It is therefore worth continuing research aimed at recognizing the respective mechanisms of TAS and VASP activity in the saliva of underweight patients.
References
Caregaro L, Favaro A, Santonastaso P, Alberino F, Di Pascoli L, Nardi M et al (2001) Insulin-like growth factor 1 (IGF-1), a nutritional marker in patients with eating disorders. Clin Nutrition 20(3):251–257. https://doi.org/10.1054/clnu.2001.0397
Paszynska E, Dmitrzak-Weglarz M, Slopien A, Tyszkiewicz-Nwafor M, Rajewski A (2016a) Salivary and serum insulin-like growth factor (IGF-1) assays in anorexic patients. World J Biol Psychiatry 17(8):615–621. https://doi.org/10.3109/15622975.2015.1023356
Vehapoglu A, Ustabas F, Ozgen TI, Terzioglu S, Cermik BB, Ozen OF (2015) Role of circulating adipocytokines vaspin, apelin and visfatin in the loss of appetite in underweight children: a pilot trial. J Pediatr Endocrinol Metab 28(9-10):1065–1071. https://doi.org/10.1515/jpem-2014-0490
Nagler RM, Klein I, Zarzhevsky N, Drigues N, Reznick AZ (2002) Characterization of the differentiated antioxidant profile of human saliva. Free Radic Biol Med 32(3):268–277. https://doi.org/10.1016/S0891-5849(01)00806-1
Sies H (1997) Oxidative stress: oxidants and antioxidants. Exp Physiol 82(2):291–295. https://doi.org/10.1113/expphysiol.1997.sp004024
Valko M, Morris H, Cronin MT (2005) Metals toxicity and oxidative stress. Curr Med Chem 12(10):1161–1208. https://doi.org/10.2174/0929867053764635
Paszynska E, Schlueter N, Slopien A, Dmitrzak-Weglarz M, Dyszkiewicz-Konwinska M, Hannig C (2015) Salivary enzyme activity in anorexic persons—a controlled clinical trial. Clin Oral Investig 19(8):1981–1989. https://doi.org/10.1007/s00784-015-1442-3
Heiker JT (2014) Vaspin (serpin A12) in obesity, insulin resistance, and inflammation. J Pept Sci 20(5):299–306. https://doi.org/10.1002/psc.2621
Klöting N, Kovacs P, Kern M, Heiker JT, Fasshauer M, Schön MR, Stumvoll M, Beck-Sickinger AG, Blüher M (2011) Central vaspin administration acutely reduces food intake and has sustained blood glucose-lowering effects. Diabetologia 54(7):1819–1823. https://doi.org/10.1007/s00125-011-2137-1
Li Q, Chen R, Moriya J, Yamakawa J, Sumino H, Kanda T (2008) A novel adipocytokine, visceral adipose tissue-derived serine protease inhibitor (vaspin), and obesity. J Int Med Res 36(4):625–629. https://doi.org/10.1177/147323000803600402
Chang HM, Park HS, Park CY, Song YS, Jang YJ (2010) Association between serum vaspin concentrations and visceral adipose tissue in Korean subjects. Metabolism 59(9):1276–1281. https://doi.org/10.1016/j.metabol.2009.11.021
Oswiecimska J, Suwala A, Swietochowska E, Ostrowska Z, Gorczyca P, Ziora-Jakutowicz K et al (2016) Serum vaspin concentrations in girls with anorexia nervosa. J Pediatr Endocrinol Metab 29:681–886
Fantuzzi G (2005) Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol 115(5):911–919. https://doi.org/10.1016/j.jaci.2005.02.023
Ogawa H, Damrongrungruang T, Hori S, Nouno K, Minagawa K, Sato M, Miyazaki H (2014) Effect of periodontal treatment on adipokines in type 2 diabetes. World J Diabetes 5(6):924–931. https://doi.org/10.4239/wjd.v5.i6.924
Pradeep AR, Raghavendra NM, Sharma A, Patel SP, Raju A, Kathariya R, Rao NS, Naik SB (2012) Association of serum and crevicular visfatin levels in periodontal health and disease with type 2 diabetes mellitus. J Periodontal 83(5):629–634. https://doi.org/10.1902/jop.2011.110272
Tan BK, Adya R, Randeva HS (2010) Omentin: a novel link between inflammation, obesity, diabesity, and cardiovascular disease. Trends Cardiovasc Med 20(5):143–148. https://doi.org/10.1016/j.tcm.2010.12.002
Bozkurt Dogan S, Ongoz Dede F, Balli U, Sertoglu E (2016) Levels of vaspin and omentin-1 in gingival crevicular fluid as potential markers of inflammation in patients with chronic periodontitis and type 2 diabetes mellitus. J Oral Sci 58(3):379–389. https://doi.org/10.2334/josnusd.15-0731
Paszynska E, Slopien A, Slebioda Z, Dyszkiewicz-Konwinska M, Weglarz M, Rajewski A (2014) Macroscopic evaluation of the oral mucosa and analysis of salivary pH in patients with anorexia nervosa. Psychiar Pol 48(3):453–464
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, 4th ed. DSM IV. Washington, DC:APA
Fontana M, Zunt S, Eckert GJ, Zero D (2005) A screening test for unstimulated salivary flow measurement. Open Dent 30:3–8
Navazesh M (1993) Methods for collecting saliva. Ann N Y Acad Sci 694(1 Saliva as a D):72–77. https://doi.org/10.1111/j.1749-6632.1993.tb18343.x
Nahler G (2009) Lorentz-formula. In: Nahler G (ed) Dictionary of pharmaceutical medicine. Springer, Vienna, p 107
Oliveras-Lopez MJ, Ruiz-Prieto I, Bolanos-Rios P, Cerda F, Martin F, Jauregui-Lobera I (2015) Antioxidant activity and nutritional status in anorexia nervosa: effects of weight recovery. Nutrients 7(4):2193–2208. https://doi.org/10.3390/nu7042193
Solmi M, Veronese N, Luchini C, Manzato E, Sergi G, Favaro A, Santonastaso P, Correll CU (2016) Oxidative stress and antioxidant levels in patients with anorexia nervosa after oral re-alimentation: a systemic review and exploratory meta-analysis. Eur Eat Disord Rev 24(2):101–105. https://doi.org/10.1002/erv.2420
Dostalova L, Kavalkova P, Papezova H, Domluvilova D, Zikan V, Haluzik M (2010) Association of macrophage inhibitory cytokine-1 with nutritional status, body composition and bone mineral density in patients with anorexia nervosa: the influence of partial realimentation. Nutr Metab (Lond) 7(1):34. https://doi.org/10.1186/1743-7075-7-34
Feillet F, Feillet-Coudray C, Bard JM, Parra HJ, Favre E, Kabuth B, Fruchart JC, Vidailhet M (2000) Plasma cholesterol and endogenous cholesterol synthesis during refeeding in anorexia nervosa. Clin Chim Acta 294(1-2):45–56. https://doi.org/10.1016/S0009-8981(99)00256-9
Haluzik M, Papezova M, Nedvidkova J, Kabrt J (1999) Serum leptin levels in patients with anorexia nervosa before and after partial refeeding, relationships to serum lipids and biochemical nutritional parameters. Physiol Res 48(3):197–202
Russell DM, Prendergast PJ, Darby PL, Garfinkel PE, Whitwell J, Jeejeebhoy KN (1983) A comparison between muscle function and body composition in anorexia nervosa: the effect of refeeding. Am J Clin Nutr 38(2):229–237. https://doi.org/10.1093/ajcn/38.2.229
Umeki S (1988) Biochemical abnormalities of the serum in anorexia nervosa. J Nerv Ment Dis 176(8):503–506. https://doi.org/10.1097/00005053-198808000-00009
Wang Y, Yang M, Lee SG, Davis CG, Koo SI, Chun OK (2012) Dietary total antioxidant capacity is associated with diet and plasma antioxidant status in healthy young adults. J Acad Nutr Diet 112(10):1626–1635. https://doi.org/10.1016/j.jand.2012.06.007
Yang M, Chung SJ, Floegel A, Song WO, Koo SI, Chun OK (2013) Dietary antioxidant capacity is associated with improved serum antioxidant status and decreased serum C-reactive protein and plasma homocysteine concentrations. Eur J Nutr 52(8):1901–1911. https://doi.org/10.1007/s00394-012-0491-5
Moyano D, Sierra C, Brandi N, Artuch R, Mira A, Garcia-Tornel S et al (1999) Antioxidant status in anorexia nervosa. Int J Eat Disord 25(1):99–103. https://doi.org/10.1002/(SICI)1098-108X(199901)25:1<99::AID-EAT12>3.0.CO;2-N
Halliwell B (1994) Free radicals, antioxidants, and human disease: curiosity, cause, or consequence? Lancet 344(8924):721–724. https://doi.org/10.1016/S0140-6736(94)92211-X
Roediger WE (1995) New views on the pathogenesis of kwashiorkor: methionine and other amino acids. J Pediatr Gastroenterol Nutr 21(2):130–136. https://doi.org/10.1097/00005176-199508000-00002
Yavari A, Javadi M, Mirmiran P, Bahadoran Z (2015) Exercise-induced oxidative stress and dietary antioxidants. Asian J Sports Med 6(1):e24898. https://doi.org/10.5812/asjsm.24898
Omodei D, Pucino V, Labruna G, Procaccini C, Galgani M, Perna F, Pirozzi D, de Caprio C, Marone G, Fontana L, Contaldo F, Pasanisi F, Matarese G, Sacchetti L (2015) Immune-metabolic profiling of anorexic patients reveals an anti-oxidant and anti-inflammatory phenotype. Metabolism 64(3):396–405. https://doi.org/10.1016/j.metabol.2014.10.025
Diab-Ladki R, Pellat B, Chahine R (2003) Decrease in the total antioxidant activity of saliva in patients with periodontal diseases. Clin Oral Investig 7(2):103–107. https://doi.org/10.1007/s00784-003-0208-5
Surdacka A, Ciezka E, Piorunska-Stolzman M, Wender-Ozegowska E, Korybalska K, Kawka E et al (2011) Relation of salivary antioxidant status and cytokine levels to clinical parameters of oral health in pregnant women with diabetes. Arch Oral Biol 56(5):428–436. https://doi.org/10.1016/j.archoralbio.2010.11.005
Brock GR, Butterworth CJ, Matthews JB, Chapple IL (2004) Local or systemic? Total antioxidant capacity in periodontitis and health. J Clin Periodontol 31(7):515–521. https://doi.org/10.1111/j.1600-051X.2004.00509.x
Johansson AK, Norring C, Unell L, Johansson A (2012) Eating disorders and oral health, a matched case-control study. Eur J Oral Sci 120(1):61–68. https://doi.org/10.1111/j.1600-0722.2011.00922.x
Ohrn R, Enzell K, Angmar-Mansson B (1999) Oral status of 81 subjects with eating disorders. Eur J Oral Sci 107(3):157–163. https://doi.org/10.1046/j.0909-8836.1999.eos1070301.x
Ohrn R, Angmar-Mansson B (2000) Oral status of 35 subjects with eating disorders 1-year study. Eur J Oral Sci 108(4):275–280. https://doi.org/10.1034/j.1600-0722.2000.108004275.x
Paszynska E, Dmitrzak-Weglarz M, Tyszkiewicz-Nwafor M, Slopien A (2016b) Salivary alpha-amylase, secretory IgA and free cortisol as neurobiological components of the stress response in the acute phase of anorexia nervosa. World J Biol Psychiatry 17(4):266–273. https://doi.org/10.3109/15622975.2016.1163419
Flink H, Bergdahl M, Tegelberg A, Rosenblad A, Lagerlof F (2008) Prevalence of hyposalivation in relation to general health, body mass index and remaining teeth in different age groups of adults. Community Dent Oral Epidemiol 36(6):523–531. https://doi.org/10.1111/j.1600-0528.2008.00432.x
Piccoli A, Codognotto M, Di Pascoli L, Boffo G, Caregaro L (2005) Body mass index and agreement between bioimpedance and anthropometry estimates of body compartments in anorexia nervosa. J Parenter Enter Nutr 29(3):148–156. https://doi.org/10.1177/0148607105029003148
Studen-Pavlovich D, Elliott M (2001) Eating disorders in women’s oral health. Dent Clin N Am 45(3):491–511
Winston AP (2012) The clinical biochemistry of anorexia nervosa. Ann Clin Biochem 49(2):132–143. https://doi.org/10.1258/acb.2011.011185
Engert V, Vogel S, Efanov SI, Duchesne A, Corbo V, Ali N (2011) Investigation into the cross-correlation of salivary cortisol and alpha-amylase responses to psychological stress. Psychoneuroendocrinology 36(9):1294–1302. https://doi.org/10.1016/j.psyneuen.2011.02.018
Granger DA, Kivlighan KT, el-Sheikh M, Gordis EB, Stroud LR (2007) Salivary alpha-amylase in biobehavioral research: recent developments and applications. Ann N Y Acad Sci 1098(1):122–144. https://doi.org/10.1196/annals.1384.008
Monteleone P, Scognamiglio P, Canestrelli B, Serino I, Monteleone AM, Maj M (2011) Asymmetry of salivary cortisol and α-amylase responses to psychosocial stress in anorexia nervosa but not in bulimia nervosa. Psychol Med 41(09):1963–1969. https://doi.org/10.1017/S0033291711000092
Nater UM, La Marca R, Florin L, Moses A, Langhans W, Koller MM et al (2006) Stress-induced changes in human salivary alpha-amylase activity—associations with adrenergic activity. Psychoneuroendocrinology 31(1):49–58. https://doi.org/10.1016/j.psyneuen.2005.05.010
Min-Seon K, Byung-Soo Y (2011) Method of preventing or treating body weight-related disorders by employing vaspin. The Asan Foundation. WO2011138977 A1. https://www.google.com/patents/WO2011138977A1?cl=en. Accessed 17 Aug 2017
Youn BS, Klöting N, Kratzsch J, Lee N, Park JW, Song ES et al (2008) Serum vaspin concentrations in human obesity and type 2 diabetes. Diabetes 57(2):372–377. https://doi.org/10.2337/db07-1045
Derosa G, Fogari E, D’Angelo A, Bianchi L, Bonaventura A, Romano D (2013) Adipocytokine levels in obese and non-obese subjects: an observational study. Inflammation 36(4):914–920. https://doi.org/10.1007/s10753-013-9620-4
Suleymanoglu S, Tascilar E, Pirgon O, Tapan S, Meral C, Abaci A (2009) Vaspin and its correlation with insulin sensitivity indices in obese children. Diabetes Res Clin Pract 84(3):325–328. https://doi.org/10.1016/j.diabres.2009.03.008
Qi D, Wang D, Zhang C, Tang X, He J, Zhao Y, Deng W, Deng X (2017) Vaspin protects against LPS-induced ARDS by inhibiting inflammation, apoptosis and reactive oxygen species generation in pulmonary endothelial cells via the Akt/GSK-3β pathway. Int J Mol Med 40(6):1803–1817. https://doi.org/10.3892/ijmm.2017.3176
Klöting N, Berndt J, Kralisch S, Kovacs P, Fasshauer M, Schön MR, Stumvoll M, Blüher M (2006) Vaspin gene expression in human adipose tissue: association with obesity and type 2 diabetes. Biochem Biophys Res Commun 339(1):430–436. https://doi.org/10.1016/j.bbrc.2005.11.039
Phalitakul S, Okada M, Hara Y, Yamawaki H (2012) A novel adipocytokine, vaspin inhibits platelet-derived growth factor-BB-induced migration of vascular smooth muscle cells. Biochem Biophys Res Commun 423(4):844–849. https://doi.org/10.1016/j.bbrc.2012.06.052
Balli U, Dogan SB, Dede FO, Sertoglu E, Keles GC (2016) The levels of visceral adipose tissue-derive d serpin, omentin-1 and tumor necrosis factor-α in the gingival crevicular fluid of obese patients following periodontal therapy. J Oral Sci 58(4):465–473. https://doi.org/10.2334/josnusd.16-0212
Phalitakul S, Okada M, Hara Y, Yamawaki H (2011) Vaspin prevents TNF-α-induced intracellular adhesion molecule-1 via inhibiting reactive oxygen species-dependent NF-κB and PKCθ activation in cultured rat vascular smooth muscle cells. Pharmacol Res 64(5):493–500. https://doi.org/10.1016/j.phrs.2011.06.001
Acknowledgements
The authors would like to thank all those who participated in this study for their enthusiastic involvement and hard work. The authors would like to thank the Poznan University of Medical Sciences for supporting the study. We gratefully acknowledge the assistance of Prof. Roger W.A. Linden and dr Richard Reisner for their helpful guidance and advice concerning English language editing.
Funding
The work was supported by the Poznan University of Medical Sciences (PUMS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. All procedures involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Disclaimer
The editors and funders had no role in the study design, data collection and analysis, the decision to publish, or the preparation of this manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Paszynska, E., Tyszkiewicz-Nwafor, M., Slopien, A. et al. Study of salivary and serum vaspin and total antioxidants in anorexia nervosa. Clin Oral Invest 22, 2837–2845 (2018). https://doi.org/10.1007/s00784-018-2370-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2370-9