Abstract
Objectives
The aim of this paper is to evaluate the influence of the internal anatomy on the leakage of root canals filled with the thermoplastic technique.
Materials and methods
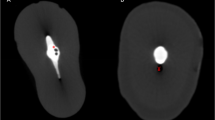
The upper central incisors (UCI) and mesial roots of the lower molars (MRLM) (n = 12 each) were tested regarding leakage using the gas-enhanced permeation test (GEPT) after root filling. The quality of the root fillings was assessed using micro-computed tomography (μCT) by superimposing scans before and after treatment to calculate unfilled volume. The calculated void volume was compared between the groups and correlated to the measured leakage values. Data were analyzed using t test and Pearson’s correlation tests (p < 0.05).
Results
The mean void volume did not differ between UCI and MRLM (13.7 ± 6.2% vs. 14.2 ± 6.8%, respectively). However, significantly more leakage was evident in the MRLM (p < 0.001). While the leakage correlated highly to the void volume in the MRLM group (R 2 = 0.981, p < 0.001), no correlation was found in UCI (R 2 = 0.467, p = 0.126).
Conclusion
MRLM showed higher leakage values, which correlated to the void volume in the root canal fillings.
Clinical relevance
Care should always be taken while doing root canal treatments, but attention to teeth with known/expected complex root canal anatomy should be considered.




Similar content being viewed by others
References
JOE Editorial Board (2008) Microbiology in endodontics: an online study guide. J Endod 34:151–164
Wu M, Wesselink P (1993) Endodontic leakage studies reconsidered. Part I. Methodology, application and relevance. Int Endod J 26:37–43
Goldman LB, Goldman M, Kronman JH, Letourneau JM (1980) Adaptation and porosity of poly-HEMA in a model system using two microorganisms. J Endod 6:683–686
Torabinejad M, Ung B, Kettering JD (1990) In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J Endod 16:566–569
Wu MK, De Gee AJ, Wesselink PR, Moorer WR (1993) Fluid transport and bacterial penetration along root canal fillings. Int Endod J 26:203–208
Shipper G, Ørstavik D, Teixeira FB, Trope M (2004) An evaluation of microbial leakage in roots filled with a thermoplastic synthetic polymer-based root canal filling material (Resilon). J Endod 30:342–347
Baumgartner G, Zehnder M, Paqué F (2007) Enterococcus faecalis type strain leakage through root canals filled with Gutta-Percha/AH plus or Resilon/Epiphany. J Endod 33:45–47
Zmener O, Pameijer CH, Alvarez Serrano S (2010) Effect of immediate and delayed post space preparation on coronal bacterial microleakage in teeth obturated with a methacrylate-based sealer with and without accelerator. Am J Dent 23:116–120
Metgud SS, Shah HH, Hiremath HT, Agarwal D, Reddy K (2015) Effect of post space preparation on the sealing ability of mineral trioxide aggregate and gutta-percha: a bacterial leakage study. J Conserv Dent 18:297–301
Ricucci D, Bergenholtz G (2003) Bacterial status in root-filled teeth exposed to the oral environment by loss of restoration and fracture or caries-a histobacteriological study of treated cases. Int Endod J 36:787–802
Ricucci D, Siqueira JF Jr, Bate AL, Pitt Ford TR (2009) Histologic investigation of root canal-treated teeth with apical periodontitis: a retrospective study from twenty-four patients. J Endod 35:493–502
Rechenberg D, De-Deus G, Zehnder M (2011) Potential systematic error in laboratory experiments on microbial leakage through filled root canals: review of published articles. Int Endod J 44:183–194
Paqué F, Al-Jadaa A, Kfir A (2012) Hard-tissue debris accumulation created by conventional rotary versus self-adjusting file instrumentation in mesial root canal systems of mandibular molars. Int Endod J 45:413–418
Rechenberg DK, Paqué F (2013) Impact of cross-sectional root canal shape on filled canal volume and remaining root filling material after retreatment. Int Endod J 46:547–555
De-Deus G (2012) Research that matters—root canal filling and leakage studies. Int Endod J 45:1063–1064
Salathe M (2010) Vorlagen für eine Generaleinwilligung und für ein Reglement. Schweiz Ärztez 91:761–763
World Health Organization (2003) Guideline for obtaining informed consent for the procurement and use of human tissue, cells and fluids in research
Federal Assembly of the Swiss Confederation. Federal act on research involving human beings 810.30, 2(2) and 32(3)
Al-Jadaa A, Attin T, Peltomäki T, Heumann C, Schmidlin PR (2014) Laboratory validation of a new gas-enhanced dentine liquid permeation evaluation system. Clin Oral Investig 18:2067–2075
Sjogren U, Hagglund B, Sundqvist G, Wing K (1990) Factors affecting the long-term results of endodontic treatment. J Endod 16:498–504
Ricucci D, Gröndahl K, Bergenholtz G (2000) Periapical status of root-filled teeth exposed to the oral environment by loss of restoration or caries. Oral Surg Oral Med Oral Pathol Oral Radiol 90:354–359
Kirkevang LL, Ørstavik D, Hörsted-Bindslev P, Wenzel A (2000) Periapical status and quality of root fillings and coronal restorations in a Danish population. Int Endod J 33:509–515
Song M, Park M, Lee CY, Kim E (2014) Periapical status related to the quality of coronal restorations and root fillings in a Korean population. J Endod 40:182–186
Archana D, Gopikrishna V, Gutmann JL, Savadamoorthi KS, Kumar AR, Narayanan LL (2015) Prevalence of periradicular radiolucencies and its association with the quality of root canal procedures and coronal restorations in an adult urban Indian. J Conserv Dent 18:34–38
Gillen BM, Looney SW, Gu LS, Loushine BA, Weller RN, Loushine RJ, Pashley DH, Tay FR (2011) Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta-analysis. J Endod 37:895–902
Muliyar S, Shameem KA, Thankachan RP, Francis PG, Jayapalan CS, Hafiz KA (2014) Microleakage in endodontics. J Int Oral Health 6:99–104
De-Deus G, Reis C, Beznos D, de Abranches AM, Coutinho-Filho T, Paciornik S (2008) Limited ability of three commonly used thermoplasticized gutta-percha techniques in filling oval-shaped canals. J Endod 34:1401–1405
von Arx T (2005) Frequency and type of canal isthmuses in first molars detected by endoscopic inspection during periradicular surgery. Int Endod J 38:160–168
Peters OA, Laib A, Rüegsegger P, Barbakow F (2000) Three-dimensional analysis of root canal geometry by high-resolution computed tomography. J Dent Res 79:1405–1409
Zhao LQ, Xu XY (2014) Influence of root canal working length on the clinical effect evaluated by periapical radiography and cone-beam computed tomography. Shanghai Kou Qiang Yi Xue 23:708–712
Di Filippo G, Sidhu SK, Chong BS (2014) Apical periodontitis and the technical quality of root canal treatment in an adult sub-population in London. Br Dent J 216:E22
Funding
The work was supported by the Clinic of Preventive Dentistry, Periodontology and Cariology, Center of Dental Medicine, University of Zurich, Zürich, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human teeth were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The current research protocol was according to the guidelines of Good Clinical Practice (ICH, Geneva, Switzerland) and did not alter the treatment plan of any of the involved patients. The institutional ethics committee approved the procedures.
Informed consent
The patients gave an informed consent that their extracted teeth could be used for study purposes anonymously.
Additional information
P. R. Schmidlin and F. Paquè share last authorship
Rights and permissions
About this article
Cite this article
Al-Jadaa, A., Attin, T., Peltomäki, T. et al. Influence of the internal anatomy on the leakage of root canals filled with thermoplastic technique. Clin Oral Invest 22, 1385–1393 (2018). https://doi.org/10.1007/s00784-017-2235-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2235-7



