Abstract
This study determined whether N-acetylcysteine (NAC) could improve intestinal function through phosphatidylinositol-3-kinase (PI3K)/protein kinase B (Akt)/mammalian target of rapamycin (mTOR), epithelial growth factor receptor (EGFR), toll-like receptor 4 (TLR4)/nuclear factor-kappa B (NF-κB), adenosine 5′-monophosphate-activated protein kinase (AMPK), and type I interferon (IFN) signaling pathways in a piglet model of lipopolysaccharides (LPS) challenge. Thirty-two piglets (24-day-old) were randomly allocated to one of four treatments, with eight replicates per treatment and one piglet per replicate. The experiment consisted of four treatments in a 2 × 2 factorial arrangement with two diets (supplemented with 0 or 500 mg NAC/kg diet) and saline or LPS administration. On day 20 of the trial, piglets in the LPS and LPS + NAC groups were intraperitoneally injected with 0 (saline) or 100 μg LPS/kg BW. Blood samples were obtained at 3 h and intestinal mucosae were collected at 6 h post LPS or saline injection. The growth performance was not affected by dietary NAC. LPS induced intestinal dysfunction, as indicated by: (1) reductions in the small-intestinal glutathione concentrations and plasma d-xylose levels; (2) elevations in plasma diamine oxidase activity, mucosal MMP3 mRNA levels and caspase-3 protein abundance; (3) reduced the activities of the small-intestinal mucosal maltase, sucrase and lactase. The adverse effects of LPS on porcine intestinal function and redox status were mitigated by NAC supplementation through the activation of multiple signaling pathways involving PI3K/Akt/mTOR, EGFR, TLR4/NF-κB, AMPK, and type I IFN. Our findings provide novel mechanisms for beneficial effects of NAC in protecting the intestine from inflammation in animals.
Similar content being viewed by others
Introduction
Because their organs and tissues are not well developed, weaned piglets are more vulnerable to various stresses, which impair intestinal health and finally reduce growth performance. It is well known that inflammation damages intestinal function as the body’s first line of defense for protecting the pigs from various harmful microorganisms, toxins, or antigens (Campbell et al. 2013). Typically, intestinal function includes digestive and absorptive functions, barrier function, and immune function, all of which are compromised in animal models with inflammation and in patients with intestinal diseases (Söderholm and Perdue 2001). Therefore, it is imperative to explore the mechanisms responsible for the regulation of intestinal function in the nutrition and health of humans and animals. To data, some key molecules are found to be involved in intestinal function, such as those for intestinal barrier function (claudin-1, occludin, zonula occludens) (Berkes et al. 2003; Hou et al. 2012), enterocyte proliferation and apoptosis (B cell lymphoma 2 and caspase-3) (Hou et al. 2012; Zhou et al. 2016), and immunity (secreted immunoglobulin A, toll-like receptor 4, nuclear factor-kappa B) (Liu et al. 2009; Chatterton et al. 2013; Hou et al. 2013). Meanwhile, mammalian target of rapamycin (mTOR) signaling pathway and toll-like receptor 4 (TLR4) signaling pathway are also reported to regulate intestinal cell growth and immune response, respectively (Marc Rhoads and Wu 2009; Hou et al. 2013; Yi et al. 2016a). However, the underlying mechanisms for stress-induced intestinal dysfunction remain largely unknown.
Lipopolysaccharide (LPS), a component of the outer membrane of Gram-negative bacteria, is commonly used to induce intestinal injury in piglets through inducing intestinal inflammation, impairing intestinal morphology and barrier function, reducing absorptive and digestive capacity, and altering intestinal energy status (Mercer et al. 1996; Liu et al. 2009; Hou et al. 2010, 2012). Using an LPS-challenged porcine model, we conducted a series of studies on the nutritional regulation of intestinal function and found that several nutrients, such as α-ketoglutarate (Hou et al. 2010), fish oil (Liu et al. 2012), N-acetylcysteine (NAC) (Hou et al. 2013), and asparagine (Chen et al. 2016), could improve intestinal function in piglets after LPS challenge. Of particular note, NAC is promising in treating various inflammatory diseases, such as gastrointestinal inflammation, cardiac injury, acute respiratory distress syndrome, bronchitis, AIDS, nephropathy, and psychiatric disorders (Samuni et al. 2013; Wu et al. 2004). Because NAC is a precursor of l-cysteine, which is utilized for the synthesis of reduced glutathione, the efficacy of NAC in treating clinical disease was contributed to its antioxidant/radical scavenger properties (Kim et al. 2001). However, recently, we found that NAC enhanced enterocyte growth and protein synthesis independent of glutathione synthesis (Yi et al. 2016a). Therefore, there could be alternative mechanisms responsible for the protective effects of NAC on intestinal function.
In view of the forgoing, we hypothesized that NAC may enhance intestinal function through multiple signaling pathways involving phosphatidylinositol-3-kinase (PI3K)/protein kinase B (Akt)/mTOR, epithelial growth factor receptor (EGFR), TLR4/nuclear factor-kappa B (NF-κB), AMP-activated protein kinase (AMPK), and type I interfere (IFN) signaling pathways. This study was conducted to test this hypothesis using a well-established piglet model of intestine injury by a LPS challenge (Liu et al. 2009; Hou et al. 2010).
Materials and methods
Experimental animals and design
The animal use protocol for the present study was approved by the Animal Care and Use Committee of Hubei Province. Thirty-two crossbred healthy piglets (Durc × Landrace × Yorkshire) were reared by sows and then weaned at 21 ± 2 days of age. After 3-day adaptation, piglets (24 ± 2 days of age, average body weight of 5.03 ± 0.59 kg) were housed individually in stainless steel metabolic cages (1.20 × 1.10 m2) and maintained at an ambient temperature of 22–25 °C (Hou et al. 2012). Piglets had free access to food and drinking water. The corn- and soybean meal-based diet was formulated to meet National Research Council (NRC, 1998)-recommended requirements for all nutrients. The experiment consisted of four treatment groups in a 2 × 2 factorial arrangement with two diets (basal diet or 500 mg/kg NAC) and two challenges (saline or LPS). All piglets had free access to the basal diet during the 3-day adaptation period. At 24 days of the age, piglets were assigned randomly into one of the four groups: (1) control group (piglets fed the basal diet and received intraperitoneal administration of sterile saline); (2) NAC group (piglets fed the basal diet supplemented with 500 mg/kg NAC and received intraperitoneal administration of sterile saline); (3) LPS group (piglets fed the basal diet and received intraperitoneal administration of Escherichia coli LPS); (4) LPS + NAC group (piglets fed the basal diet supplemented with 500 mg/kg NAC and received intraperitoneal administration of E. coli LPS). Each group had eight piglets. LPS was dissolved in sterile saline. To obtain isocaloric diets, the diets for piglets in the control and LPS groups were supplemented with 500 mg cornstarch per kg diet (Hou et al. 2012, 2013). The dosage of 500 mg/kg NAC was chosen according to our previous studies that dietary supplementation with 500 mg/kg NAC exerted positive effects on the small intestine in LPS-challenged piglets (Hou et al. 2012, 2013). Due to a negligible increase of 0.0042% nitrogen by NAC supplementation, we deemed it not necessary to use non-essential amino acids as an isonitrogenous control (Yi et al. 2014). Feed consumption and BW were recorded on day 0 and 20 of the trial before the administration of LPS or saline. On days 20 of the trial, overnight fasted piglets of the LPS and LPS + NAC groups received intraperitoneal administration of LPS (E. coli serotype 055: B5; Sigma Chemical Inc., St. Louis, MO, USA) at the dose of 100 μg/kg BW, whereas piglets in the control and NAC groups received intraperitoneal administration of the same volume of sterile saline (Hou et al. 2012, 2013). To test intestinal function, 2 h after LPS or saline administration, d-xylose was orally administrated to all piglets at the dose of 0.1 g/kg BW (Hou et al. 2010). At 3 h post-administration of LPS or saline (1 h after d-xylose infusion), blood samples were collected from the anterior vena cava into heparinized vacuum tubes and centrifuged (3500g for 10 min at 4 °C) for separating plasma (Wang et al. 2015). Plasma samples were stored at −80 °C until analysis.
Six hours after the LPS or saline injection, all piglets were killed under anesthesia with an intravenous injection of pentobarbital sodium (50 mg/kg BW). The pig abdomen was then opened immediately from the sternum to the pubis, and the whole gastrointestinal tract was immediately exposed (Hou et al. 2010). The small intestine was dissected free of the mesentery and placed on a chilled stainless steel tray. Segments (10 cm in length) were obtained from the distal duodenum, mid-jejunum, and mid-ileum (Wang et al. 2008a) and were then opened longitudinally and contents were carefully flushed with ice-cold PBS (Hou et al. 2012). Mucosa was collected by scraping using a sterile glass microscope slide at 4 °C (Hou et al. 2010), rapidly frozen in liquid nitrogen and stored at −80 °C until analysis. All samples were collected within 15 min after being killed.
Plasma biochemical parameters and hormones
An automatic biochemical analyzer (HITACHI 7020, Japan) was used to determine plasma biochemical parameters, such as aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase (ALP), creatine kinase (CK), blood urea nitrogen (BUN), total bilirubin (TBIL), cholesterol (CHOL) and creatinine.
Concentrations of insulin, insulin-like growth factor 1 (IGF-1), and cortisol in plasma were analyzed using commercially available 125I kits (Beijing SINO-UK Institute of Biological Technology, Beijing, China) as previously described by Kang et al. (2010, 2014). The detection limit for insulin was 2 μIU/mL, and the intra-and interassay CV were 10 and 15%. The detection limits for IGF-1 and cortisol analyses were 21 and 1 ng/mL, respectively. The coefficients of variation for intra- and inter-assays of IGF-1 were less than 15 and 10%, respectively, and less than 10 and 15% for cortisol analysis.
d-Xylose in plasma
d-Xylose in plasma was determined as described by Hou et al. (2012). Briefly, plasma (50 μL) was added to 5 mL of the phloroglucinol color reagent solution (Sigma Chemical Inc., St. Louis, MO, USA) and heated then at 100 °C for 4 min. The samples were allowed to cool to room temperature in a water bath. Xylose standard solutions were prepared by dissolving d-xylose in saturated benzoic acid (prepared in deionized water) to obtain 0, 0.7, 1.3, 2.6 mM. Each d-xylose standard or sample was added to the color reagent solution. The absorbance of samples and standard solutions at 554 nm were measured using a spectrophotometer (Model 6100, Jenway Ltd., Felsted, Dunmow, CM6 3LB, Essex, England, UK). The standard solution of 0 mmol/L d-xylose was considered as the blank (Hou et al. 2010).
Diamine oxidase (DAO) activity in plasma and intestine
Diamine oxidase activities in plasma and intestinal mucosa were determined by spectrophotometry method as previously described (Hou et al. 2012). For measurement of intestinal DAO activity, the small intestinal mucosa (0.5 g) was homogenized in phosphate buffer (0.1 M, pH 7.2) and centrifuged then (10,000g for 30 min at 4 °C) to collect the supernatant fluid for DAO assays. The assay mixture (3.8 mL) contained 3 mL of phosphate buffer (0.2 M, pH 7.2), 0.1 mL (0.004%) of horseradish peroxidase solution (Sigma Chemicals), 0.1 mL of o-dianisidine-methanol solution (0.5% of o-dianisidine in methanol), 0.5 mL of plasma or intestinal homogenate and 0.1 mL of substrate solution (0.175% of cadaverine dihydrochloride, Sigma Chemicals). This mixture was incubated for 30 min at 37 °C, and absorbance at 436 nm was measured to indicate DAO activity (Hou et al. 2012). Protein was also measured as described by Hou et al. (2010).
Disaccharidase activity in the small intestine
Mucosal disaccharidase activity was determined using glucose kits (Cat. A082-1, A082-2, and A082-3 for lactase, sucrase, and maltase, respectively; Nanjing Jiancheng Bioengineering Institute, Nanjing, China) as previously described (Liu et al. 2009). Briefly, 10 mL of double-distilled water, glucose standard solution (5.55 mM) or test samples (supernatant fluid collected from the mucosal homogenate with PBS) were added to a test tube and incubated with 20 mL of respective substrate for 20 min at 37 °C. 10 mL of terminating agent and 1 mL of chromogenic agent were then added and incubated at 37 °C for 15 min. Double-distilled water was used to set zero at 505 nm, followed by the reading of the optical density value of each tube. One unit (U) of enzyme activity was defined as 1 nmol substrate hydrolyzed per minute under assay conditions (37 °C, pH 6). Mucosal protein was also determined as described by Hou et al. (2010).
Intestinal mucosal DNA, RNA and protein
The DNA, RNA and protein were extracted using the TRI REAGENT-RNA/DNA/Protein isolation reagent and their concentrations were determined with the use of a colorimetric method (Hou et al. 2012). DNA was analyzed fluorimetrically using the method of Prasad et al. (1972). RNA was determined by spectrophotometry using a modified Schmidt–Tannhauser method as described by Munro and Fleck (1969). Protein was analyzed according to the method of Lowry et al. (1951). For measurement of DNA and RNA concentrations, the mucosa was homogenized (2 min) in a 100-fold volume of ice-cold saline (0.9%) and the homogenate was centrifuged (1800g for 10 min at 4 °C) to obtain the supernatant fluid for analysis. For measurement of mucosal protein, mucosal samples (~0.1 g) were homogenized in a 1 mL of ice-cold PBS-EDTA buffer (0.05 M Na3PO4, 2.0 M NaCl, 2 mM EDTA, pH 7.4) and homogenates were then centrifuged (12,000g for 10 min at 4 °C) to obtain the supernatant fluid for assays.
Intestinal mucosal glutathione (GSH) and cysteine
Cellular concentrations of GSH and cysteine were determined by high-performance liquid chromatography (HPLC) according to the methods of Wang et al. (2014) with modifications. A frozen intestinal tissue (~50 mg) was homogenized with 1.5 mL of homogenization buffer (a mixture of 12 mM iodoacetic acid and 1.5 M HClO4; 50:50, v/v), and the homogenate was transferred to a 15-mL polystyrene tube. The homogenizer was rinsed with 1.5 mL of the homogenization buffer. The combined homogenate was neutralized with 0.75 mL of 2 M K2CO3 and mixed. After centrifugation (3000g for 5 min), an aliquot of the supernatant fluid (50 μL) was stored at −20 °C until derivatization with iodoacetic acid (25 mM) (Yi et al. 2016a). The HPLC system consisted of a model 2475 multi λ fluorescence detector (excitation and emission wavelength were set at 220 and 450 nm, respectively; gain was set at 1), a Supelco C18 column (4.6 mm × 15 cm, 3 μm; Sigma-Aldrich, St. Louis, MO, USA), a Supelco C18 guard column (4.6 mm × 5 cm, 20–40 μm; Sigma-Aldrich, St. Louis, MO, USA), and a Model 600E Powerline multisolvent delivery system with 100 μL heads, a Model 717 plus WISP Autosampler. In the HPLC workstation, the autosampler was programmed to mix 25 μL of sample (or standard) with 25 μL of the o-phthaldialdehyde solution (50 mg o-phthaldialdehyde was dissolved in 1.25 mL methanol and added with 11.2 mL of 40 mM sodium borate buffer, 50 μL of 2-mercaptoethanol, and 0.4 mL of Brij-35) for 1 min, and the derivatized solution was then injected into the HPLC column without any delay (Yi et al. 2016a).
mRNA analysis by qRT-PCR
Each frozen mucosal sample (~100 mg) was powdered under liquid nitrogen using a mortar and pestle. The powdered samples were homogenized and the total RNA was isolated using the TRIzol Reagent protocol (Invitrogen, Carlsbad, CA, USA). Total RNA was quantified using the NanoDrop® ND-1000A UV–VIS spectrophotometer (Thermo Scientific, Wilmington, DE, USA) at an OD of 260 nm, and its purity was assessed by determining the OD260/OD280 ratio. All of the samples had an OD260/OD280 ratio above 1.8, corresponding to 90–100% pure nucleic acids (Hou et al. 2013; Yi et al. 2016a). Meanwhile, RNA integrity in each sample was determined using 1% denatured agarose gel electrophoresis. RNA was used for RT-PCR analysis when it had a 28 S/18 S rRNA ratio ≥1.8. Total RNA was reverse-transcribed using a PrimeScript® RT reagent kit with gDNA Eraser (Takara, Dalian, China) according to the manufacturer’s instruction. cDNA was synthesized and stored at −20 °C until use.
To amplify cDNA fragments, the primer pairs (Supplementary Table 1) were used for qRT-PCR. To minimize amplification of potentially contaminating genomic DNA, the primers were designed to span introns and intron–exon boundaries. The qRT-PCR was performed using the SYBR® Premix Ex Taq™ (Takara, Dalian, China) on an Applied Biosystems 7500 Fast Real-Time PCR System (Foster City, CA, USA). The total volume of PCR reaction system was 50 μL. In brief, the reaction mixture contained 0.2 µM of each primer, 25 µL of SYBR® Premix Ex Taq™ (2×) and 4 µL of cDNA in a 50-µL reaction volume. All PCRs were performed in triplicate on a 96-well real-time PCR plate (Applied Biosystems) under the following conditions (two-step amplification): 95 °C for 30 s, followed by 40 cycles of 95 °C for 5 s and 60 °C for 31 s. A subsequent melting curve (95 °C for 15 s, 60 °C for 1 min and 95 °C for 15 s) with continuous fluorescence measurement and final cooling to room temperature was processed. The specificity of the qRT-PCR reactions was assessed by analyzing the melting curves of the products and size verification of the amplicons (Meurens et al. 2009). To ensure the sensitivity and accuracy of the results obtained by qRT-PCR, samples were normalized internally using simultaneously the average cycle threshold (C t) of ribosomal protein L4 (RPL4), hypoxanthine phosphoribosyltransferase 1 (HPRT1), and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) as references in each sample to avoid any artifact of variation in the target gene (Meurens et al. 2009; Hou et al. 2013). Results were analyzed by \(2^{ - \Delta\Delta C_t}\) method (Livak and Schmittgen 2001; Nygard et al. 2007). Each biological sample was run in triplicate.
Protein immunoblot analysis
Protein immunoblot analysis was carried out in accordance with the previously described method (Hou et al. 2012; Yi et al. 2014, 2016a). Briefly, frozen mucosal sample (~100 mg) were powdered and homogenized in 1 mL lysis buffer (20 mM HEPES, pH 7.4, 2 mM EGTA, 50 mM NaF, 100 mM KCl, 0.2 mM EDTA, 50 mM b-glycerophosphate, 1 mM dithiothreitol, 0.1 mM PMSF, 1 mM benzamidine, and 0.5 mM sodium vanadate) with a homogenizer. After centrifuged (12,000g, 15 min, 4 °C), the supernatant fluid was aliquoted into micro-centrifuge tubes, to which 2× SDS sample buffer was added in a 1:1 ratio. The samples were boiled and cooled on ice before use for western blotting. Proteins were separated by electrophoresis on a 10% polyacrylamide gel, and then electrophoretically transferred to a polyvinylidene difluoride (PVDF) membrane. Skim-milk powder in TBST buffer (1× Tris-buffered saline including 0.1% Tween 20) was used to block membrane for 1 h at room temperature. Membranes were incubated with primary antibodies overnight at 4 °C: claudin-1 (1:1000, Invitrogen Technology), occludin (1:1000, Invitrogen Technology), casapse-3 (1:1000, Cell Signaling Technology), Ras (1:1000, Cell Signaling Technology), EGFR (1:1000, Cell Signaling Technology), PI3K (1:1000, Santa Cruz), Erk1/2 (1:1000, Cell Signaling Technology), Akt (1:1000, Cell Signaling Technology), p-EGFR (Tyr1173, 1:1000, Santa Cruz), p-PI3K (Tyr508, 1:1000, Santa Cruz), p-Erk1/2 (Thr202/Tyr204, 1:1000, Cell Signaling Technology), p-Akt (Ser473, 1:1000, Cell Signaling Technology) or β-actin (1:5000, Sigma Chemicals). The membranes were washed with TBS-T and incubated for 1 h at room temperature with anti-rabbit (mouse) immunoglobulin G horseradish peroxidase conjugated secondary antibody (Beijing ZhongShan Golden Bridge Biological Technology Co., LTD, China; 1:5000 dilution). After being washed with TBST, blots on the membrane were developed using an enhanced chemiluminescence Western blotting kit (ECL-plus, Amersham Biosciences, Sweden), visualized and quantified using an imaging system (Alpha Innotech FluorChem FC2, CA, USA).
Statistical analysis
All values are expressed as mean with pooled SEM. The data were analyzed using the General Linear Model (Univariate) procedure in SPSS13.0 (SPSS Inc., Chicago, IL, USA) in a 2 × 2 factorial arrangement with diet and LPS as the main effects. The differences among treatments were evaluated by Duncan’s multiple comparison test. Additionally, difference in the means of growth performance was determined by the Student’s paired t test. Probability values ≤0.05 were taken to indicate statistical significance.
Results
Growth performance
From day 0 to 20 of the trial, piglets fed the NAC diet exhibited no significant difference in growth performance, compared with those fed with the basal diet (Table 1).
Blood biochemical parameters and hormones
LPS induced alterations in blood biochemical parameters and hormones of piglets (Table 2). Regardless of diet, LPS treatment increased (P < 0.05) the activities of plasma AST and ALP, as well as the concentrations of plasma BUN and creatinine in comparison with the saline treatment. On the other hand, dietary NAC supplementation elevated (P < 0.05) the plasma insulin concentration irrespective of LPS challenge. In addition, there were significant interactions (P < 0.05) between NAC and LPS in plasma TBIL and cortisol levels (Table 2), showing that dietary supplementation of NAC mitigated the elevations of plasma TBIL and cortisol in piglets challenged with LPS.
Concentrations of plasma d-xylose, DAO activity in plasma and intestinal mucosa
As shown in Table 3, pigs in the LPS group showed lower (P < 0.05) DAO activity in the duodenum than those of the saline group. Dietary supplementation with NAC increased (P < 0.05) DAO activity in the jejunum compared with the basal diet. There were significant interactions (P < 0.05) between LPS and NAC in plasma d-xylose level and DAO activity, and the data showed that dietary NAC supplementation increased d-xylose concentration and decreased DAO activity in plasma of LPS-challenged piglets (Table 3).
Intestinal disaccharidase activity
Effects of NAC on the activities of maltase, sucrase and lactase in the small intestine are shown in Table 4. Compared with piglets administrated with saline, LPS-challenged piglets exhibited lower (P < 0.05) activities of maltase and lactase in the duodenum and ileum, and of sucrase activity in the jejunum and ileum. Dietary supplementation with NAC increased (P < 0.05) maltase activity in the duodenum and jejunum, sucrase activity in the ileum, and lactase activity in the duodenum compared with the basal diet. Additionally, there were significant interactions between NAC and LPS in duodenal sucrase activity and jejunal lactase activity. It was observed that under LPS challenge dietary supplementation of NAC increased (P < 0.05) the activities of duodenal sucrase and jejunal lactase.
Concentrations of DNA, RNA, and protein in the small intestinal mucosa
Compared with the saline treatment, LPS treatment decreased (P < 0.05) the DNA concentration and protein/DNA ratio in the duodenum. Piglets receiving the NAC diet had higher (P < 0.05) DNA concentration, RNA/DNA, and protein/DNA in the duodenum in comparison with those receiving the basal diet (Table 5). No interactions between NAC and LPS were observed in mucosal DNA concentrations, RNA/DNA, and protein/DNA.
Concentrations of GSH and cysteine in intestinal mucosa
Effects of NAC on intestinal GSH and cysteine of piglets was illustrated in Table 6. LPS challenge decreased (P < 0.05) the concentrations of GSH in the duodenum and cysteine in the duodenum and jejunum as compared with the saline group. On the other hand, compared with the basal diet, NAC diet increased (P < 0.05) the levels of GSH and cysteine in the duodenum of piglets.
mRNA levels for genes associated with intestinal functions and several important signaling pathways
As shown in Table 7, both LPS and NAC affected intestinal gene expression of piglets. LPS-challenged piglets exhibited higher (P < 0.05) mRNA levels for matrix metalloproteinase-3 (MMP3), sodium-dependent neutral amino acid transporter (ASCT2) and sodium-coupled neutral amino acid transporter 2 (SNAT2), but lower (P < 0.05) mRNA levels for sodium-independent amino acid transporter (b0,+AT) and peptide transporter 1 (PepT1) than piglets administrated with saline. On the other hand, NAC diet up-regulated (P < 0.05) the expression of porcine β defensin 1 (pBD-1), and Gap junction alpha-1 (GJA1) in the jejunal mucosa of piglets compared with the basal diet. In addition, there were significant interactions between NAC and LPS in the mRNA levels for Bcl-2, junctional adhesion molecule A (JAM-A), villin, aquaporin 3 (AQP3), and aquaporin 10 (AQP10). Specifically, dietary NAC attenuated the reductions of Bcl-2, villin, AQP3, and AQP10 mRNA levels and increased JAM-A mRNA levels in the jejunal mucosa of LPS-challenged piglets (Table 7).
Regarding the mRNA levels for genes encoding key molecules of PI3K/Akt/mTOR signaling, significant interactions between NAC and LPS were observed in mRNA levels for mTOR and 4E-binding protein-1 (4EBP1). Dietary NAC supplementation attenuated the reduction in mTOR mRNA levels in the jejunal mucosa of LPS-challenged piglets. NAC also up-regulated (P < 0.05) 4EBP1 expression in the jejunal mucosa of piglets.
Concerning gene expression related to EGFR signaling pathway, NAC supplementation up-regulated (P < 0.05) EGFR expression in porcine intestine compared to the basal diet group. On the contrary, LPS administration down-regulated (P < 0.05) of EGFR expression in the jejunal mucosa of piglets in comparison with saline treatment. NAC or LPS did not affect the mRNA abundances of Ras and extracellular signal-regulated kinase 1/2 (Erk1/2) in the jejunal mucosa of piglets (Table 7).
The immune-responsive signaling pathway, TLR4/NF-κB signaling, was also regulated by LPS and NAC (Table 7). Significant interactions (P < 0.05) between LPS and NAC were observed in mRNA levels for TLR4, NF-κB, chemokine (C-X-C motif) ligand 9 (CXCL9), CXCL10, CXCL11, interleukin-1 beta (IL-1β), and heat shock protein 105 kDa (HSPH1). Specifically, dietary NAC supplementation attenuated the elevations of mRNA levels for TLR4, NF-κB, CXCL10, CXCL11, IL-1β, and HSPH1 in the jejunal mucosa of piglets challenged with LPS. It was interesting that piglets fed the NAC diet and simultaneously challenged by LPS had the highest CXCL9 mRNA level than other piglets. Additionally, pigs in the LPS group showed an increase (P < 0.05) in NOD2 expression than those in saline group.
LPS challenge induced up-regulation (P < 0.05) of AMPK in the jejunum of piglets. Significant interactions between NAC and LPS were also observed in mRNA levels for uncoupling protein 2 (UCP2) and ADP/ATP translocase 1 (ANT1), showing that dietary NAC reduced UCP2 mRNA levels and increased ANT1 mRNA levels in the small intestine of LPS-challenged piglets (Table 7).
There were significant interactions (P < 0.05) between NAC and LPS in regulating expression of genes encoding for the proteins involved in type I IFN signaling. Specifically, dietary NAC supplementation increased (P < 0.05) the mRNA levels for IFN-β, interferon-induced protein with tetratricopeptide repeats 1 (IFIT1), and myxovirus resistance 1 (MX1) in the jejunal mucosa of piglets challenged with LPS. Additionally, piglets receiving the NAC diet showed higher mRNA levels for (P < 0.05) 2′-5′-oligoadenylate synthetase-like protein (OASL) and dsRNA dependent protein kinase R (PKR) than those receiving the basal diet.
Abundance of proteins involving in intestinal function and EGFR and PI3K/Akt/mTOR signaling pathways
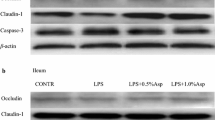
Piglets challenged by LPS and fed the NAC diet exhibited a decrease (P < 0.05) in intestinal caspase-3 abundance, but an increase (P < 0.05) in claudin-1 abundance in comparison with those challenged by LPS and fed the basal diet (Fig. 1). Moreover, compared with the saline treatment, LPS induced a reduction (P < 0.05) in occludin abundance, which was tended to be elevated (P = 0.056) by NAC.
Abundances of caspase-3, claudin-1, occludin, epithelial growth factor receptor (EGFR), Ras, Erk1/2, phosphatidylinositol-3-kinase (PI3K), and Akt in the jejunal mucosa of piglets. The experiment consisted of four treatment groups in a 2 × 2 factorial arrangement with two diets (basal diet or 500 mg/kg NAC) and two injections (saline injection or LPS injection). Piglets were randomly allocated to one of four treatments. The experiment lasted for 21 days. Piglets were killed at 6 h post LPS or saline injection (day 20 of the trial) and intestinal mucosa were collected for protein analysis. NAC reduced the caspase-3 amount, but increased the protein abundances of claudin-1, as well as the relative EGFR, Erk1/2, PI3K, and Akt phosphorylation in LPS-challenged piglets. Data are mean ± SEM, n = 8. a–cMeans sharing different letters differ (P < 0.05)
Additionally, both NAC and LPS could regulate the EGFR and PI3K/Akt/mTOR signaling at protein levels. Specifically, compared with the saline group, LPS decreased (P = 0.031) Erk1/2 phosphorylation in the porcine jejunum. However, NAC supplementation increased (P = 0.011) Erk1/2 phosphorylation, compared with the basal diet. Significant interactions between NAC and LPS were observed in the phosphorylation of the EGFR, PI3K and Akt proteins. The data showed that NAC could enhance (P < 0.05) EGFR, PI3K, and Akt phosphorylation in the small intestine of LPS-challenged piglets (Fig. 1).
Discussion
The present study showed the dietary NAC supplementation did not affect the growth performance of piglets in the absence of LPS challenge, which was in a good line with our previous studies (Hou et al. 2012; Wang et al. 2013). However, NAC could increase the average daily gain of piglets under chronic LPS challenge (Hou et al. 2012) and decrease the feed/gain and mortality rate of heat-stressed broilers (Yi et al. 2016b), indicating that NAC may exert beneficial effects on the growth of stressed animals.
With an acute LPS challenge, the porcine liver may be damaged as indicated by the elevations in the activities of plasma AST and ALP, as well as plasma TBIL level. Similarly, renal function may be adversely affected by LPS injection as substantiated by the increases of BUN and creatinine concentrations in plasma of LPS piglets. It is well known that LPS challenge can induce elevations in plasma pro-inflammatory cytokines, such as TNF-α, IL-1 and IL-6, and subsequently result in hepatic abnormalities (McClain et al. 1993; Kamimura and Tsukamoto 1995) and renal dysfunction (Samuvel et al. 2016). Our previous studies have also reported the hepatic injury induced by LPS in a porcine model (Yi et al. 2014; Wang et al. 2015). However, dietary NAC supplementation may partially attenuate the hepatic injury in LPS-challenged piglets, which was supported by the reduction in plasma TBIL and cortisol levels in spite of no differences in plasma AST and ALP activities. Actually, there appeared to be an inconsistency with our earlier report that NAC decreased AST activity in the plasma of LPS-challenged piglets (Yi et al. 2014). We speculated the type of LPS challenge (chronic vs. acute) and sampling times (24 vs. 6 h after LPS injection) might have contributed to the inconsistency. Additionally, it is worth noting that NAC could increase the plasma insulin level irrespective of LPS challenge, showing that NAC may promote anabolic metabolism in piglets.
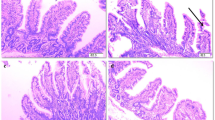
Moreover, the present study also focused on the effects of NAC on intestinal functions of piglets. It has been demonstrated that LPS challenge can induce immune stress and oxidative stress, and ultimately cause intestinal dysfunction and injury (Mercer et al. 1996; Liu et al. 2009; Hou et al. 2010). Because plasma d-xylose level and DAO activity serve as an indicators of intestinal absorption function and integrity (Hou et al. 2012), respectively, our results that dietary NAC attenuated the decrease in plasma d-xylose level and the increase in plasma DAO activity induced by LPS indicated the improvement of intestinal absorption function and integrity by NAC supplementation. This notion was substantiated by the evidence that NAC increased the jejunal DAO activity and claudin-1 protein abundance. Additionally, NAC could improve the intestinal digestive function as indicated by our finding that NAC increased the duodenal sucrase and jejunal lactase activities in LPS-challenged piglets. Disaccharides are secreted by the intestinal epithelial cells, and their activities could indirectly reflect the intestinal villus development and epithelial integrity (Yi et al. 2016b). Therefore, increases in disaccharidase activity are consistent with the improvement of intestinal integrity by NAC. In addition, other intestinal indices, such as DNA concentrations, as well as RNA/DNA ratio and protein/DNA ratio, can be used to assess intestinal development (Hou et al. 2012). These indices were enhanced in the duodenum of NAC-supplemented pigs irrespective of LPS challenge. Collectively, NAC supplementation could improve intestinal absorption, digestion, and integrity of LPS-challenged piglets.
To elucidate the underlying mechanisms whereby NAC exerts beneficial effects on intestinal functions of LPS piglets, we first investigated the alterations of GSH and cysteine in the intestine. LPS reduced the duodenal GSH level, as well as duodenal and jejunal cysteine levels, which may partially be due to the oxidative stress induced by LPS. On the contrary, dietary NAC elevated the concentrations of GSH and cysteine in the duodenum, which was in accordance with our previous study on an intestinal epithelial cell model (Yi et al. 2016a). Therefore, it is reasonable to infer that dietary NAC provides cysteine for the synthesis of GSH, or spares other antioxidants such as superoxide dismutase and catalase (Yi et al. 2014), and consequently improves intestinal anti-oxidative capacity and attenuate intestinal oxidative stress.
It is also possible that NAC improved intestinal function possibly via regulating the expression of genes associated with enterocyte proliferation, intestinal barrier function, and nutrient transport. Specifically, LPS challenge down-regulated of Bcl-2, which is a key intrinsic blocker of apoptosis by preventing mitochondrial permeabilization (Steinle 2012) and was increased by NAC supplementation. The data also showed that NAC decreased caspase-3 protein abundance in LPS pigs (Fig. 1) and we speculated that NAC may inhibit the enterocyte apoptosis induced by LPS through up-regulating Bcl-2 gene expression and down-regulating caspase-3 protein expression. It is noteworthy that the villin mRNA level was reduced by LPS, and was restored to the control level by NAC supplementation. Villin is known as a major actin-modifying protein in gastrointestinal epithelium and its reduction may be related to disturbances in differentiation and maturation process in the intestinal epithelium of IBD patients (Wang et al. 2008b). Therefore, up-regulation of villin expression may be an alternative mechanism for improving intestinal integrity by NAC. Likewise, GJA1, also known as connexin 43, plays an important role in sustaining intestinal epithelial barrier function (Ey et al. 2009) and was increased by dietary NAC supplementation. Moreover, intestinal tight junction protein claudin-1 was elevated by NAC supplementation in LPS-challenged piglets; further substantiating that NAC could improve the intestinal barrier function in pigs. Of note, dietary NAC also increased the mRNA levels for pBD-1, which is an important antimicrobial peptide for protecting against bacterial infection in the intestine (Veldhuizen et al. 2009). Additionally, a previous study reported that MMP3 was expressed at high levels in the intestine of clinical IBD and celiac diseases (Li et al. 2004), which is consistent with our results that LPS challenge increased mRNA levels for MMP3 rather MMP9. The down-regulation of intestinal AQP3 and AQP10 by LPS may result in reductions in water absorption and water imbalance, and thus cause diarrhea in piglets. Patients with IBD disease who develop severe diarrhea have similar reductions in AQP4 and AQP8 expression (Yamamoto et al. 2007). Hou et al. (2013) reported that NAC did not affect the intestinal AQP8 expression. Interestingly, results of the present study indicated that NAC could up-regulate AQP3 and AQP10 expression in LPS piglets, indicating the specific regulation of NAC on intestinal aquaporin expression. LPS, rather than NAC, could regulate the expression of intestinal amino acid or peptide transporters. Specifically, LPS reduced the expression of b0,+AT and PepT1, but increased the expression of ASCT2 and SNAT2. There were many variable results concerning effects of LPS on the expression of amino acid transporters and peptide transporters. For instance, Shu et al. (2002) reported that LPS treatment significantly decreased the expression of mRNA for PepT1 in intestine, and Wittmann et al. (2015) also reported indicated that L-type amino acid transporter 1 (LAT1) mRNA was decreased in brain blood vessels in response to LPS. However, Inoue et al. (1995) showed the expression of both sodium-independent (y+ and b0,+) and -dependent (A, ASC, N) amino acid transport systems, rather than the L system, were up-regulated in liver, and Hsu et al. (2016) observed an increase in cationic amino acid transporter-2 (CAT2) in uveitis in response to LPS. Therefore, it seems that types of amino acid transporters and tissue specificity may be responsible for the inconsistency of LPS challenge.
Another mechanism for the effect of NAC in improving intestinal function may involve the expression of key genes associated with PI3K/Akt/mTOR, EGFR, TLR4/NF-κB, AMPK, and type I IFN cell signaling. mTOR is well known as a stimulator of protein synthesis (Suryawan et al. 2009), and its upstream molecules are Akt and PI3K. Dietary NAC supplementation increased mTOR and 4EBP1 mRNA levels, and attenuated the reductions in relative PI3K and Akt phosphorylation induced by LPS in the jejunum of piglets (Fig. 1). Our previous studies have also indicated that NAC enhanced the abundances of total and phosphorylated proteins for mTOR and P70S6K in enterocytes (Yi et al. 2016a). Therefore, NAC could improve intestinal cell protein synthesis via regulating PI3K/Akt/mTOR signaling. Similarly, the EGFR signaling pathway was regulated by both NAC and LPS (Fig. 1). The EGFR signaling pathway was reported to be associated with the damage and recovery of the small intestinal mucosa, and such key molecules as EGF and EGFR are critical for stimulating enterocyte proliferation and regeneration of intestinal epithelium (Hou et al. 2013). LPS induced down-regulation of EGFR mRNA and protein phosphorylation, as well as the downstream Erk1/2 phosphorylation in the jejunum. On the contrary, NAC increased both mRNA levels and protein phosphorylation of EGFR and Erk1/2 in the jejunal mucosa of piglets, indicating that NAC regulated the activities of these two proteins at both transcriptional and post-translational levels. Collectively, NAC improved intestinal growth and integrity possibly via activating the PI3K/Akt/mTOR and EGFR signaling pathways.
The TLR4/NF-κB signaling is well known to be involved in inflammation induced by LPS. TLR4 is a transmembrane receptor of LPS and its activation causes intestinal cell apoptosis (Tan et al. 2010) and enhanced intestinal permeability (Leaphart et al. 2007). Besides, TLR4 can induce NF-κB activation, which further results in the transcription of target genes for the inflammatory cytokines (Yi et al. 2014), as observed in the present study involving the administration of LPS into piglets. Of note, NAC supplementation could attenuate the up-regulation of genes encoding for inflammatory cytokines such as CXCL9, CXCL10, CXCL11, IL-1β, as well as HSPH1. Previous studies have shown that NAC reduced the NF-κB and HSP70 protein abundances, as well as mucosal tumor necrosis factor alpha (TNF-α) and IL-6 concentrations in the small intestine of LPS-challenged pigs (Hou et al. 2013) and in enterocytes (Ji et al. 2016). Therefore, dietary NAC may attenuate the intestinal inflammation and improve intestinal immune function via regulating the TLR4/NF-κB signaling pathway.
We have reported that LPS alters intestinal energy metabolism and induces reductions in jejunal ATP concentration and elevations in the ratio of AMP to ATP (Hou et al. 2011). The possible explanation may be attributed to the up-regulation of UCP2 expression and down-regulation of ANT1 induced by LPS in the small intestine. UCP2 is commonly proposed to inhibit the mitochondrial production of reactive oxygen species (Mailloux and Harper 2011). Faggioni et al. (1998) reported that LPS increased UCP2 mRNA levels in the mouse liver (28-fold), skeletal muscle (fivefold), and white adipose tissue (fivefold). ANT1 can drive the exchange of ADP/ATP between the cytosol and mitochondria, and ANT1 knockdown cells exhibited a decrease in the mitochondrial respiration control ratio (Pan et al. 2015). Importantly, we found that dietary NAC supplementation reduced UCP2 mRNA levels and attenuated the decrease of the ANT1 transcripts in LPS-challenged piglets, indicating an improvement of intestinal energy metabolism. In addition, AMPK is a critical regulator of energy metabolism and activated when the cellular energy level is low (Jobgen et al. 2006). The current study indicated that AMPK expression was not affected by dietary NAC supplementation, although it was up-regulated by LPS challenge.
Finally, a salient finding of the present work is that NAC supplementation regulated the mRNA levels for genes related to the intestinal type I IFN signaling pathway. The cellular response to viral infection includes the induction of genes for type-I interferons, IFN-α and IFN-β, which are produced in most cell types and play a vital role in innate resistance to viral and bacterial infections (Takaoka and Yanai 2006). IFN-α/β can induce the expression of genes encoding antiviral proteins such as OASL, IFIT, MX, and PKR (García-Sastre and Biron 2006). Our results showed that NAC up-regulated the expression of genes encoding IFN-β and OASL, IFIT1, MX1, and PKR. In vitro studies also showed that NAC increased the expression of antiviral proteins and the viability of enterocytes infected with porcine epidemic diarrhea virus (unpublished data). Therefore, NAC may enhance intestinal antiviral function through activating type I signaling pathway. It remains to be determined whether NAC itself affects gene expression or acts indirectly through GSH synthesis or anti-oxidative signaling.
In conclusion, dietary NAC supplementation improved intestinal immune function (demonstrated by the reductions in plasma cortisol levels and intestinal mRNA levels for the TLR4/NF-κB signaling pathway), digestive and absorptive functions (indicated by the elevations of intestinal disaccharidase activities, plasma d-xylose concentration, and mRNA levels for AQP3 and AQP10), anabolic metabolism (shown by the increases in insulin activity, DNA levels, RNA/DNA ratio, and protein/DNA ratio, as well as up-regulations of the Bcl-2, villin, and PI3K/Akt/mTOR signaling pathways), barrier function (demonstrated by the reduction in plasma DAO concentration and elevations in mRNA levels for the pBD-1, JAM-A, GJA, and EGFR signaling pathways), inhibition of mitochondrial production of reactive oxygen species and improvement of energy metabolism (indicated by increased transcripts of UCP2 and ANT1), and antiviral capacity (shown by up-regulation of expression of genes for the type I IFN signaling pathway) in LPS-challenged piglets. Therefore, the beneficial effects of NAC on intestinal functions in piglets challenged with LPS were multifaceted and may be mediated by multiply signaling pathways involving TLR4/NF-κB, PI3K/Akt/mTOR, EGFR, AMPK, type I IFN signaling pathways.
Abbreviations
- Akt:
-
Protein kinase B
- AMPK:
-
Adenosine 5′-monophosphate-activated protein kinase
- ANT1:
-
ADP/ATP translocase 1
- AQP3:
-
Aquaporin 3
- ASCT2:
-
Sodium-dependent neutral amino acid transporter 2
- Bax:
-
Bcl-2 associated X protein
- Bcl-2:
-
B cell lymphoma 2
- b0,+AT:
-
Sodium-independent amino acid transporter
- CXCL9:
-
Chemokine (C-X-C motif) ligand 9
- EGFR:
-
Epithelial growth factor receptor
- Erk1/2:
-
Extracellular signal-regulated kinase ½
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- GJA1:
-
Gap junction alpha-1
- HPRT1:
-
Hypoxanthine phosphoribosyltransferase 1
- HSPH1:
-
Heat shock protein 105 kDa
- IFIT1:
-
Interferon-induced protein with tetratricopeptide repeats 1
- IFN:
-
Interferon
- MMP3:
-
Matrix metalloproteinase-3
- JAM-A:
-
Junctional adhesion molecule A
- mTOR:
-
Mammalian target of rapamycin
- MX1:
-
Myxovirus resistance 1
- NAC:
-
N-Acetylcysteine
- NF-κB:
-
Nuclear factor-kappa B
- NOD2:
-
Nucleotide binding oligomerization domain containing 2
- OASL:
-
2′-5′-Oligoadenylate synthetase-like protein
- pBD-1:
-
Porcine β-defense 1
- PepT1:
-
Peptide transporter 1
- PI3K:
-
Phosphatidylinositol-3-kinase
- PKR:
-
DsRNA dependent protein kinase R
- P70S6K:
-
Ribosomal protein S6 kinase
- RPL4:
-
Ribosomal protein L4
- SNAT2:
-
Sodium-coupled neutral amino acid transporter 2
- TLR4:
-
Toll-like receptor 4
- UCP2:
-
Uncoupling protein 2
- 4EBP1:
-
4E-binding protein-1
References
Berkes J, Viswanathan VK, Savkovic SD et al (2003) Intestinal epithelial responses to enteric pathogens: effects on the tight junction barrier, ion transport, and inflammation. Gut 52:439–451
Campbell JM, Crenshaw JD, Polo J (2013) The biological stress of early weaned piglets. J Anim Sci Biotechnol 4:19
Chatterton DE, Nguyen DN, Bering SB et al (2013) Anti-inflammatory mechanisms of bioactive milk proteins in the intestine of newborns. Int J Biochem Cell Biol 45:1730–1747
Chen S, Liu Y, Wang X et al (2016) Asparagine improves intestinal integrity, inhibits TLR4 and NOD signaling, and differently regulates p38 and ERK1/2 signaling in weanling piglets after LPS challenge. Innate Immun. doi:10.1177/1753425916664124
Ey B, Eyking A, Gerken G et al (2009) TLR2 mediates gap junctional intercellular communication through connexin-43 in intestinal epithelial barrier injury. J Biol Chem 284:22332–22342
Faggioni R, Shigenaga J, Moser A et al (1998) Induction of UCP2 gene expression by LPS: a potential mechanism for increased thermogenesis during infection. Biochem Biophys Res Commun 244:75–78
García-Sastre A, Biron CA (2006) Type 1 interferons and the virus-host relationship: a lesson in Détente. Science 312:879–882
Hou YQ, Wang L, Ding BY et al (2010) Dietary α-ketoglutarate supplementation ameliorates intestinal injury in lipopolysaccharide-challenged piglets. Amino Acids 39:555–564
Hou YQ, Yao K, Wang L et al (2011) Effects of α-ketoglutarate on energy status in the intestinal mucosa of weaned piglets chronically challenged with lipopolysaccharide. Br J Nutr 106:357–363
Hou YQ, Wang L, Zhang W et al (2012) Protective effects of N-acetylcysteine on intestinal functions of piglets challenged with lipopolysaccharide. Amino Acids 43:1233–1242
Hou YQ, Wang L, Yi D et al (2013) N-acetylcysteine reduces inflammation in the small intestine by regulating redox, EGF and TLR4 signaling. Amino Acids 45:513–522
Hsu YR, Chang SW, Yang CH et al (2016) Expression profile of cationic amino acid transporters in rats with endotoxin-induced uveitis. Mediat Inflamm 2016:6586857
Inoue Y, Bode BP, Abcouwer S et al (1995) Attenuation of the endotoxin-stimulated increase in hepatic amino acid transport with a glucocorticoid receptor antagonist. J Surg Res 58:693–701
Ji Y, Dai ZL, Wu G et al (2016) 4-Hydroxy-2-nonenal induces apoptosis by activating ERK1/2 signaling and depleting intracellular glutathione in intestinal epithelial cells. Sci Rep 6:32929
Jobgen WS, Fried SK, Fu WJ et al (2006) Regulatory role for the arginine-nitric oxide pathway in metabolism of energy substrates. J Nutr Biochem 17:571–588
Kamimura S, Tsukamoto H (1995) Cytokine gene expression by Kupffer cells in experimental alcoholic liver disease. Hepatology 22:1304–1309
Kang P, Xiao HL, Hou YQ et al (2010) Effects of Astragalus polysaccharides, Achyranthes bidentata polysaccharides, and Acantbepanax senticosus paponin on the performance and immunity in weaned pigs. Asian Aust J Anim Sci 23:750–756
Kang P, Zhang LL, Hou YQ et al (2014) Effects of l-proline on the growth performance, and blood parameters in weaned lipopolysaccharide (LPS)-challenged pigs. Asian Aust J Anim Sci 27:1150–1156
Kim KY, Rhim T, Choi I et al (2001) N-acetylcysteine induces cell cycle arrest in hepatic stellate cells through its reducing activity. J Biol Chem 276:40591–40598
Leaphart CL, Cavallo J, Gribar SC et al (2007) A critical role for TLR4 in the pathogenesis of necrotizing enterocolitis by modulating intestinal injury and repair. J Immunol 179:4808–4820
Li CK, Pender SL, Pickard KM et al (2004) Impaired immunity to intestinal bacterial infection in stromelysin-1 (matrix metalloproteinase-3)-deficient mice. J Immunol 173:5171–5179
Liu Y, Han J, Huang J et al (2009) Dietary l-arginine supplementation improves intestinal function in weaned pigs after an Escherichia coli lipopolysaccharide challenge. Asian Aust J Anim Sci 22:1667–1675
Liu Y, Chen F, Odle J et al (2012) Fish oil enhances intestinal integrity and inhibits TLR4 and NOD2 signaling pathways in weaned pigs after LPS challenge. J Nutr 142:2017–2024
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2−∆∆CT method. Methods 25:402–408
Lowry OH, Rosebrough NJ, Farr AL (1951) Protein measurement with the folin phenol reagent. J Biol Chem 193:265–275
Mailloux RJ, Harper ME (2011) Uncoupling proteins and the control of mitochondrial reactive oxygen species production. Free Radic Biol Med 51:1106–1115
Marc Rhoads J, Wu G (2009) Glutamine, arginine, and leucine signaling in the intestine. Amino Acids 37:111–222
McClain C, Hill D, Schmidt J et al (1993) Cytokines and alcoholic liver disease. Semin Liver Dis 13:170–182
Mercer DW, Smith GS, Cross JM et al (1996) Effects of lipopolysaccharide on intestinal injury: potential role of nitric oxide and lipid peroxidation. J Surg Res 63:185–192
Meurens F, Berri M, Auray G et al (2009) Early immune response following Salmonella enterica subspecies enterica serovar Typhimurium infection in porcine jejunal gut loops. Vet Res 40:5
Munro HN, Fleck A (1969) Analysis of tissues and body fluids for nitrogenous constituents. In: Munro HN (ed) Mammalian protein metabolism. Academic Press, NY, pp 465–483
Nygard A, Jørgensen CB, Cirera S et al (2007) Selection of reference genes for gene expression studies in pig tissues using SYBR green qPCR. BMC Mol Biol 8:67
Pan S, Wang N, Bisetto S et al (2015) Downregulation of adenine nucleotide translocator 1 exacerbates tumor necrosis factor-α-mediated cardiac inflammatory responses. Am J Physiol Heart Circ Physiol 308:H39–H48
Prasad AS, DeMouchelle E, Koniuchi D (1972) A simple fluorimetric method for the determination of RNA and DNA in tissue. J Lab Clin Med 80:598–601
Samuni Y, Goldstein S, Dean OM et al (2013) The chemistry and biological activities of N-acetylcysteine. Biochim Biophys Acta 1830:4117–4129
Samuvel DJ, Shunmugavel A, Singh AK et al (2016) S-Nitrosoglutathione ameliorates acute renal dysfunction in a rat model of lipopolysaccharide-induced sepsis. J Pharm Pharmacol 68:1310–1319
Shu HJ, Takeda H, Shinzawa H et al (2002) Effect of lipopolysaccharide on peptide transporter 1 expression in rat small intestine and its attenuation by dexamethasone. Digestion 65:21–29
Söderholm JD, Perdue MH (2001) Stress and gastrointestinal tract. II. Stress and intestinal barrier function. Am J Physiol Gastrointest Liver Physiol 280:G7–G13
Steinle JJ (2012) Retinal endothelial cell apoptosis. Apoptosis 17:1258–1260
Suryawan A, O’Connor PMJ, Bush JA et al (2009) Differential regulation of protein synthesis by amino acids and insulin in peripheral and visceral tissues of neonatal pigs. Amino Acids 37:105–110
Takaoka A, Yanai H (2006) Interferon signalling network in innate defence. Cell Microbiol 8:907–922
Tan BE, Yin YL, Kong XF et al (2010) L-arginine stimulates proliferation and prevents endotoxin-induced death of intestinal cells. Amino Acids 38:1227–1235
Veldhuizen EJA, Koomen I, Ultee T et al (2009) Salmonella serovar specific upregulation of porcine defensins 1 and 2 in a jejuna epithelial cell line. Vet Microbial 136:69–75
Wang J, Chen L, Li D et al (2008a) Intrauterine growth restriction affects the proteomes of the small intestine, liver and skeletal muscle in newborn pigs. J Nutr 138:60–66
Wang Y, Srinivasan K, Siddiqui MR et al (2008b) A novel role for villin in intestinal epithelial cell survival and homeostasis. J Biol Chem 283:9454–9464
Wang QJ, Hou YQ, Yi D et al (2013) Protective effects of N-acetylcysteine on acetic acid-induced colitis in a porcine model. BMC Gastroenterol 13:133
Wang W, Dai Z, Wu Z et al (2014) Glycine is a nutritionally essential amino acid for maximal growth of milk-fed young pigs. Amino Acids 46:2037–2045
Wang L, Hou YQ, Yi D et al (2015) Dietary supplementation with glutamate precursor α-ketoglutarate attenuates lipopolysaccharide-induced liver injury in young pigs. Amino Acids 47:1309–1318
Wittmann G, Mohácsik P, Balkhi MY et al (2015) Endotoxin-induced inflammation down-regulates L-type amino acid transporter 1 (LAT1) expression at the blood-brain barrier of male rats and mice. Fluids Barriers CNS 12:21
Wu G, Fang YZ, Yang S et al (2004) Glutathione metabolism and its implications for health. J Nutr 134:489–492
Yamamoto T, Kuramoto H, Kadowaki M (2007) Downregulation in aquaporin 4 and aquaporin 8 expression of the colon associated with the induction of allergic diarrhea in a mouse model of food allergy. Life Sci 81:115–120
Yi D, Hou YQ, Wang L et al (2014) Dietary N-acetylcysteine supplementation alleviates liver injury in lipopolysaccharide-challenged piglets. Br J Nutr 111:46–54
Yi D, Hou Y, Wang L et al (2016a) N-acetylcysteine stimulates protein synthesis in enterocytes independently of glutathione synthesis. Amino Acids 48:523–533
Yi D, Hou YQ, Tan LL et al (2016b) N-acetylcysteine improves the growth performance and intestinal function in the heat-stressed broilers. Anim Feed Sci Technol 220:83–92
Zhou Y, Li Y, Zhou B et al (2016) Inflammation and apoptosis: dual mediator role for Toll-like receptor 4 in the development of necrotizing enterocolitis. Inflamm Bowel Dis. doi:10.1097/MIB.0000000000000961
Acknowledgements
This research was jointly supported by National Natural Science Foundation of China (31372319, 31572416, 31402084), the Hubei Provincial Key Project for Scientific and Technical Innovation (2014ABA022), Hubei Provincial Research and Development Program (2010BB023), Hubei Provincial Technology and Innovation Program (2016ABA121), Natural Science Foundation of Hubei Province (2016CFA070), Research and Innovation Initiatives of WHPU (2016J08), the Hubei Hundred Talent Program, Agriculture and Food Research Initiative Competitive Grants (2014-67015-21770) of the USDA National Institute of Food and Agriculture, and Texas AgriLife Research (H-82000).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statement
All experimental procedures were approved by the Institutional Animal Care and Use Committee at Wuhan Polytechnic University.
Additional information
Handling Editor: C.-A. A. Hu, Y. Yin, Y. Hou, G. Wu, Y. Teng.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yi, D., Hou, Y., Xiao, H. et al. N-Acetylcysteine improves intestinal function in lipopolysaccharides-challenged piglets through multiple signaling pathways. Amino Acids 49, 1915–1929 (2017). https://doi.org/10.1007/s00726-017-2389-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-017-2389-2