Abstract
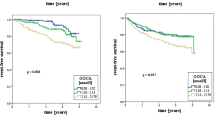
Renal transplant recipients (RTR) have an increased cardiovascular risk profile. Low levels of circulating homoarginine (hArg) are a novel risk factor for mortality and the progression of atherosclerosis. The kidney is known as a major source of hArg, suggesting that urinary excretion of hArg (UhArg) might be associated with mortality and graft failure in RTR. hArg was quantified by mass spectrometry in 24-h urine samples of 704 RTR (functioning graft ≥1 year) and 103 healthy subjects. UhArg determinants were identified with multivariable linear regression models. Associations of UhArg with all-cause mortality and graft failure were assessed using multivariable Cox regression analyses. UhArg excretion was significantly lower in RTR compared to healthy controls [1.62 (1.09–2.61) vs. 2.46 (1.65–4.06) µmol/24 h, P < 0.001]. In multivariable linear regression models, body surface area, diastolic blood pressure, eGFR, pre-emptive transplantation, serum albumin, albuminuria, urinary excretion of urea and uric acid and use of sirolimus were positively associated with UhArg, while donor age and serum phosphate were inversely associated (model R 2 = 0.43). During follow-up for 3.1 (2.7–3.9) years, 83 (12 %) patients died and 45 (7 %) developed graft failure. UhArg was inversely associated with all-cause mortality [hazard risk (HR) 0.52 (95 % CI 0.40–0.66), P < 0.001] and graft failure [HR 0.58 (0.42–0.81), P = 0.001]. These associations remained independent of potential confounders. High UhArg levels are associated with reduced all-cause mortality and graft failure in RTR. Kidney-derived hArg is likely to be of particular importance for proper maintenance of cardiovascular and renal systems.



Similar content being viewed by others
Abbreviations
- ADMA:
-
Asymmetric dimethylarginine
- BSA:
-
Body surface area
- CI:
-
Confidence interval
- DBP:
-
Diastolic blood pressure
- eGFR:
-
Estimated glomerular filtration rate
- FFQ:
-
Food frequency questionnaire
- hArg:
-
Homoarginine
- HbA1c :
-
Glycated hemoglobin
- HDL:
-
High-density lipoprotein
- HLA:
-
Human leukocyte antigen
- HR:
-
Hazard risk
- hsCRP:
-
High-sensitivity C-reactive protein
- IQR:
-
Interquartile range
- KTx:
-
Kidney transplantation
- LDL:
-
Low-density lipoprotein
- LOD:
-
Lower limit of detection
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- NT-pro-BNP:
-
N-terminal pro-hormone of brain natriuretic peptide
- PTH:
-
Parathyroid hormone
- QC:
-
Quality control
- RTR:
-
Renal transplant recipients
- SDMA:
-
Symmetric dimethylarginine
- UhArg:
-
Urinary homoarginine
References
Atzler D, Rosenberg M, Anderssohn M et al (2013) Homoarginine—an independent marker of mortality in heart failure. Int J Cardiol 168:4907–4909
Atzler D, Gore MO, Ayers CR et al (2014) Homoarginine and cardiovascular outcome in the population-based Dallas Heart Study. Arterioscler Thromb Vasc Biol 34:2501–2507
Bretscher LE, Li H, Poulos TL, Griffith OW (2003) Structural characterization and kinetics of nitric-oxide synthase inhibition by novel N5-(iminoalkyl)- and N5-(iminoalkenyl)-ornithines. J Biol Chem 278:46789–46797
Drechsler C, Meinitzer A, Pilz S et al (2011) Homoarginine, heart failure, and sudden cardiac death in haemodialysis patients. Eur J Heart Fail 13:852–859
Drechsler C, Kollerits B, Meinitzer A et al (2013) Homoarginine and progression of chronic kidney disease: results from the Mild to Moderate Kidney Disease Study. PLoS One 8:e63560
Frenay AR, van den Berg E, de Borst MH, Beckmann B, Tsikas D, Feelisch M, Navis G, Bakker SJ, van Goor H (2015) Plasma ADMA associates with all-cause mortality in renal transplant recipients. Amino Acids. doi:10.1007/s00726-015-2023-0
Hecker M, Walsh DT, Vane JR (1991) On the substrate specificity of nitric oxide synthase. FEBS Lett 294:221–224
Israni AK, Leduc R, Jacobson PA et al (2013) Inflammation in the setting of chronic allograft dysfunction post-kidney transplant: phenotype and genotype. Clin Transplant 27:348–358
Jones SP, Bolli R (2006) The ubiquitous role of nitric oxide in cardioprotection. J Mol Cell Cardiol 40:16–23
Kasiske BL (2000) Cardiovascular disease after renal transplantation. Semin Nephrol 20:176–187
Kayacelebi AA, Nguyen TH, Neil C et al (2014a) Homoarginine and 3-nitrotyrosine in patients with takotsubo cardiomyopathy. Int J Cardiol 173:546–547
Kayacelebi AA, Beckmann B, Gutzki FM, Jordan J, Tsikas D (2014b) GC-MS and GC-MS/MS measurement of the cardiovascular risk factor homoarginine in biological samples. Amino Acids 46:2205–2217
Khalil AA, Tsikas D, Akolekar R et al (2013) Asymmetric dimethylarginine, arginine and homoarginine at 11–13 weeks’ gestation and preeclampsia: a case-control study. J Hum Hypertens 27:38–43
Kopple JD, Greene T, Chumlea WC et al (2000) Relationship between nutritional status and the glomerular filtration rate: results from the MDRD study. Kidney Int 57:1688–1703
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Mallon DH, Summers DM, Bradley JA, Pettigrew GJ (2013) Defining delayed graft function after renal transplantation: simplest is best. Transplantation 96:885–889
Marescau B, Nagels G, Possemiers I, De Broe ME, Becaus I, Billiouw JM, Lornoy W, De Deyn PP (1997) Guanidino compounds in serum and urine of nondialyzed patients with chronic renal insufficiency. Metabolism 46:1024–1031
März W, Meinitzer A, Drechsler C et al (2010) Homoarginine, cardiovascular risk, and mortality. Circulation 122:967–975
Moali C, Boucher JL, Sari MA et al (1998) Substrate specificity of NO synthases: detailed comparison of l-arginine, homo-l-arginine, their N omega-hydroxy derivatives, and N omega-hydroxynor-l-arginine. Biochemistry 37:10453–10460
Molnar MZ, Kovesdy CP, Bunnapradist S et al (2011) Associations of pretransplant serum albumin with post-transplant outcomes in kidney transplant recipients. Am J Transplant 11:1006–1015
Moncada S, Higgs A (1993) The l-arginine-nitric oxide pathway. N Engl J Med 329:2002–2012
O’Connor PM, Cowley AW Jr (2010) Modulation of pressure-natriuresis by renal medullary reactive oxygen species and nitric oxide. Curr Hypertens Rep 12:86–92
Ojo AO, Hanson JA, Wolfe RA et al (2000) Long-term survival in renal transplant recipients with graft function. Kidney Int 57:307–313
Passauer J, Pistrosch F, Bussemaker E (2005) Nitric oxide in chronic renal failure. Kidney Int 67:1665–1667
Pilz S, Meinitzer A, Tomaschitz A et al (2011a) Low homoarginine concentration is a novel risk factor for heart disease. Heart 97:1222–1227
Pilz S, Tomaschitz A, Meinitzer A et al (2011b) Low serum homoarginine is a novel risk factor for fatal strokes in patients undergoing coronary angiography. Stroke 42:1132–1134
Pilz S, Edelmann F, Meinitzer A et al (2014) Associations of methylarginines and homoarginine with diastolic dysfunction and cardiovascular risk factors in patients with preserved left ventricular ejection fraction. J Card Fail 20:923–930
Ravani P, Maas R, Malberti F et al (2013) Homoarginine and mortality in pre-dialysis chronic kidney disease (CKD) patients. PLoS One 8:e72694
Rettkowski O, Wienke A, Hamza A et al (2007) Low body mass index in kidney transplant recipients: risk or advantage for long-term graft function? Transplant Proc 39:1416–1420
Smith GL, Lichtman JH, Bracken MB, Shlipak Phillips CO, DiCapua P et al (2006) Renal impairment and outcomes in heart failure: systematic review and meta-analysis. J Am Coll Cardiol 47:1987–1996
Takahashi T, Harris RC (2014) Role of endothelial nitric oxide synthase in diabetic nephropathy: lessons from diabetic eNOS knockout mice. J Diabetes Res 2014:590541
The Hague (2006) Dutch food composition table (NEVO 2006) NEVO table 2006 (dutch nutrient databank: NEVO table 2006)
Tomaschitz A, Meinitzer A, Pilz S et al (2014) Homoarginine, kidney function and cardiovascular mortality risk. Nephrol Dial Transplant 29:663–671
Tomaschitz A, Verheyen N, Gaksch M, Meinitzer A, Pieske B, Kraigher-Krainer E, Colantonio C, März W, Schmidt A, Belyavskiy E, Rus-Machan J, van Ballegooijen AJ, Stiegler C, Amrein K, Ritz E, Fahrleitner-Pammer A, Pilz S (2015) Homoarginine in patients with primary hyperparathyroidism. Am J Med Sci 349:306–311
Valtonen P, Laitinen T, Lyyra-Laitinen T et al (2008) Serum l-homoarginine concentration is elevated during normal pregnancy and is related to flow-mediated vasodilatation. Circ J 72:1879–1884
van den Berg E, Engberink MF, Brink EJ et al (2012a) Dietary acid load and metabolic acidosis in renal transplant recipients. Clin J Am Soc Nephrol 7:1811–1818
van den Berg E, Geleijnse JM, Brink EJ et al (2012b) Sodium intake and blood pressure in renal transplant recipients. Nephrol Dial Transplant 27:3352–3359
van den Berg E, Engberink MF, Brink EJ et al (2013) Dietary protein, blood pressure and renal function in renal transplant recipients. Br J Nutr 109:1463–1470
van den Berg E, Pasch A, Westendorp WH et al (2014) Urinary sulfur metabolites associate with a favorable cardiovascular risk profile and survival benefit in renal transplant recipients. J Am Soc Nephrol 25:1303–1312
Wu G, Bazer FW, Davis TA et al (2009) Arginine metabolism and nutrition in growth, health and disease. Amino Acids 37:153–168
Wyss M, Kaddurah-Daouk R (2000) Creatine and creatinine metabolism. Physiol Rev 80:1107–1213
Xia Z, Vanhoutte PM (2011) Nitric oxide and protection against cardiac ischemia. Curr Pharm Des 17:1774–1782
Yang Z, Ming XF (2006) Endothelial arginase: a new target in atherosclerosis. Curr Hypertens Rep 8:54–59
Zoccali C (2006) Traditional and emerging cardiovascular and renal risk factors: an epidemiologic perspective. Kidney Int 70:26–33
Acknowledgments
This work was supported by Grants from the Dutch Kidney Foundation (NSN C08-2254, P13-114), by COST Action BM1005: ENOG: European Network on Gasotransmitters (www.gasotransmitters.eu), and by the Top Institute Food and Nutrition (A-1003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
The Institutional Review Board approved the study protocol (METc 2008/186) which was in adherence to the Declaration of Helsinki.
Conflict of interest
All authors report no conflicts of interest.
Additional information
A.-R. S. Frenay and A. A. Kayacelebi have contributed equally to this work and are both first authors.
S. J. L. Bakker and D. Tsikas are both senior authors.
Rights and permissions
About this article
Cite this article
Frenay, AR.S., Kayacelebi, A.A., Beckmann, B. et al. High urinary homoarginine excretion is associated with low rates of all-cause mortality and graft failure in renal transplant recipients. Amino Acids 47, 1827–1836 (2015). https://doi.org/10.1007/s00726-015-2038-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-015-2038-6