Abstract
Objective
This study aimed to identify factors affecting proptosis recovery in spheno-orbital meningioma (SOM) surgery and assess functional and oncological outcomes.
Methods
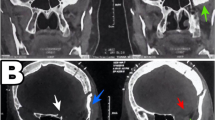
Data from 32 consecutive SOM surgery cases (2002–2021) were analyzed. Clinical, radiological, operative, and oncological parameters were examined. Proptosis was assessed using the exophthalmos index (EI) on MRI or CT scans. Statistical analyses were performed to identify predictive factors for proptosis recovery.
Results
Proptosis improved in 75% of patients post-surgery (EI decreased from 1.28 ± 0.16 to 1.20 ± 0.13, p = 0.048). Patients with stable or worsened EI had higher body mass index (28.5 ± 7.9 vs. 24.1 ± 4.7, p = 0.18), Simpson grade (IV 75% vs. 65%, p = 0.24), and middle sphenoid wing epicenter involvement (63% vs. 38%, p = 0.12), but no significant factors were associated with unfavorable exophthalmos outcomes. The improvement group had higher en plaque morphology, infratemporal fossa invasion, and radiation treatment for cavernous sinus residual tumor (88% vs. 75%, p = 0.25; 51% vs. 25%, p = 0.42; 41% vs. 25%, p = 0.42, respectively), but without statistical significance. Visual acuity remained stable in 78%, improved in 13%, and worsened in 9% during follow-up. Surgery had a positive impact on preoperative oculomotor nerve dysfunction in 3 of 4 patients (75%). Postoperative oculomotor nerve dysfunction was observed in 25%, of which 75% fully recovered. This occurrence was significantly associated with irradiation of an orbital tumor residue (p = 0.04). New postoperative trigeminal hypoesthesia was observed in 47%, of which 73% recovered. All SOMs were classified as WHO grade 1, and complementary treatments achieved oncological control, requiring gamma-knife radiosurgery in 53% and standard radiotherapy in 6%.
Conclusions
Surgery effectively improves proptosis in SOM, though complete resolution is rare. The absence of predictive factors suggests multifactorial causes, including body mass index and tumor resection grade. Postoperative oculomotor nerve dysfunction and trigeminal hypoesthesia are common but often recover. Gamma-knife radiosurgery maintains long-term oncological control for evolving tumor residue.





Similar content being viewed by others
Data availability
All data and materials used in this study are available upon reasonable request from the corresponding author.
Code availability
Any custom code or software developed for this research is available upon request from the corresponding author.
Abbreviations
- ASA:
-
American society of anesthesiologists
- BMI:
-
Body mass index
- EI:
-
Exophthalmos index
- OO:
-
Orbital opening
- SOM:
-
Spheno-orbital meningioma
- VA:
-
Visual acuity
References
Apra C, Roblot P, Alkhayri A, Le Guérinel C, Polivka M, Chauvet D (2020) Female gender and exogenous progesterone exposition as risk factors for spheno-orbital meningiomas. J Neurooncol 149(1):95–101. https://doi.org/10.1007/s11060-020-03576-8
Baucher G, Bernard F, Graillon T, Dufour H (2019) Interfascial approach for pterional craniotomy: technique and adjustments to prevent cosmetic complications. Acta Neurochirurgica.https://doi.org/10.1007/s00701-019-04058-1
Baucher G, Troude L, Roche PH (2022) Spheno-orbital meningiomas. In: Skull base surgery [Working Title]. IntechOpen. https://doi.org/10.5772/intechopen.101983
Baucher G, Troude L, Roux A, et al (2022) Predictors of visual function after resection of skull base meningiomas with extradural anterior clinoidectomy. Neurosurg Rev. https://doi.org/10.1007/s10143-021-01716-w
Bowers CA, Sorour M, Patel BC, Couldwell WT (2016) Outcomes after surgical treatment of meningioma-associated proptosis. J Neurosurg 125(3):544–550. https://doi.org/10.3171/2015.9.JNS15761
Cushing H (1922) The menigiomas (dural endotheliomas): their source, and favoured seats of origin. Brain 45(2):282–316. https://doi.org/10.1093/brain/45.2.282
Cushing H, Eisenhardt L (1938) Meningiomas. Their classification, regional behaviour, life history, and surgical end results. Bull Med Libr Assoc 27(2):185–185
DeMonte F, McDermott MW, Al-Mefty O, eds (2011) Al-Mefty’s Meningiomas. Georg Thieme Verlag. https://doi.org/10.1055/b-002-80424
Elborady MA, Nazim WM (2021) Spheno-orbital meningiomas: surgical techniques and results. Egypt J Neurol Psychiatry Neurosurg 57(1):18. https://doi.org/10.1186/s41983-021-00276-6
Fisher FL, Zamanipoor Najafabadi AH, Schoones JW, Genders SW, Furth WR (2021) Surgery as a safe and effective treatment option for spheno-orbital meningioma: a systematic review and meta-analysis of surgical techniques and outcomes. Acta Ophthalmol 99(1):26–36. https://doi.org/10.1111/aos.14517
Freeman JL, Davern MS, Oushy S et al (2017) Spheno-orbital meningiomas: a 16-year surgical experience. World Neurosurgery 99:369–380. https://doi.org/10.1016/j.wneu.2016.12.063
Girkin CA, Comey CH, Lunsford LD, Goodman ML, Kline LB (1997) Radiation optic neuropathy after stereotactic radiosurgery. Ophthalmology 104(10):1634–1643. https://doi.org/10.1016/S0161-6420(97)30084-0
Goldbrunner R, Minniti G, Preusser M et al (2016) EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol 17(9):e383–e391. https://doi.org/10.1016/S1470-2045(16)30321-7
Hiniker SM, Modlin LA, Choi CY et al (2016) Dose-response modeling of the visual pathway tolerance to single-fraction and hypofractionated stereotactic radiosurgery. Semin Radiat Oncol 26(2):97–104. https://doi.org/10.1016/j.semradonc.2015.11.008
Kim RB, Fredrickson VL, Couldwell WT (2022) Visual outcomes in spheno-orbital meningioma: a 10-year experience. World Neurosurg 158:e726–e734. https://doi.org/10.1016/j.wneu.2021.11.048
Kiyofuji S, Casabella AM, Graffeo CS, Perry A, Garrity JA, Link MJ (2021) Sphenoorbital meningioma: a unique skull base tumor. Surgical technique and results. J Neurosurg 133(4):1044–1051. https://doi.org/10.3171/2019.6.JNS191158
Leroy HA, Leroy-Ciocanea CI, Baroncini M et al (2016) Internal and external spheno-orbital meningioma varieties: different outcomes and prognoses. Acta Neurochir 158(8):1587–1596. https://doi.org/10.1007/s00701-016-2850-0
Masalha W, Heiland DH, Steiert C et al (2021) Progression-free survival, prognostic factors, and surgical outcome of spheno-orbital meningiomas. Front Oncol 11:672228. https://doi.org/10.3389/fonc.2021.672228
Menon S, Sandesh O, Anand D, Menon G (2020) Spheno-orbital meningiomas: optimizing visual outcome. J Neurosci Rural Pract 11(03):385–394. https://doi.org/10.1055/s-0040-1709270
Nagahama A, Goto T, Nagm A et al (2019) Spheno-Orbital meningioma: surgical outcomes and management of recurrence. World Neurosurg 126:e679–e687. https://doi.org/10.1016/j.wneu.2019.02.123
Oya S, Sade B, Lee JH (2011) Sphenoorbital meningioma: surgical technique and outcome: clinical article. JNS 114(5):1241–1249. https://doi.org/10.3171/2010.10.JNS101128
Peyster R, Ginsberg F, Silber J, Adler L (1986) Exophthalmos caused by excessive fat: CT volumetric analysis and differential diagnosis. Am J Roentgenol 146(3):459–464. https://doi.org/10.2214/ajr.146.3.459
Rawanduzy CA, Budohoski KP, Rennert RC, Winkler-Schwartz A, Couldwell WT (2023) Spheno-orbital meningiomas. Neurosurg Clin N Am 34(3):417–423. https://doi.org/10.1016/j.nec.2023.02.006
Van Rij AM, De Alwis CS, Jiang P et al (2008) Obesity and impaired venous function. Eur J Vasc Endovasc Surg 35(6):739–744. https://doi.org/10.1016/j.ejvs.2008.01.006
Ringel F, Cedzich C, Schramm J (2007) Microsurgical technique and results of a series of 63 spheno-orbital meningiomas. Operative Neurosurgery 60:214–222. https://doi.org/10.1227/01.NEU.0000255415.47937.1A
Roser F, Nakamura M, Jacobs C, Vorkapic P, Samii M (2005) Sphenoid wing meningiomas with osseous involvement. Surg Neurol 64(1):37–43. https://doi.org/10.1016/j.surneu.2004.08.092
Saeed P, van Furth WR, Tanck M et al (2011) Natural history of spheno-orbital meningiomas. Acta Neurochir 153(2):395–402. https://doi.org/10.1007/s00701-010-0878-0
Scarone P, Leclerq D, Héran F, Robert G (2009) Long-term results with exophthalmos in a surgical series of 30 sphenoorbital meningiomas: Clinical article. JNS 111(5):1069–1077. https://doi.org/10.3171/2009.1.JNS081263
Shrivastava RK, Sen C, Costantino PD, Della RR (2005) Sphenoorbital meningiomas: surgical limitations and lessons learned in their long-term management. J Neurosurg 103(3):491–497. https://doi.org/10.3171/jns.2005.103.3.0491
Smolders MH, Graniewski-Wijnands HS, Meinders AE, Fogteloo AJ, Pijl H, De Keizer RJW (2004) Exophthalmos in obesity. Ophthalmic Res 36(2):78–81. https://doi.org/10.1159/000076885
Terrier LM, Bernard F, Fournier HD et al (2018) Spheno-orbital meningiomas surgery: multicenter management study for complex extensive tumors. World Neurosurg 112:e145–e156. https://doi.org/10.1016/j.wneu.2017.12.182
Troude L, Bernard F, Bauchet G, De La Rosa MS, Roche PH (2017) Extradural resection of the anterior clinoid process: how I do it. Neurochirurgie 63(4):336–340. https://doi.org/10.1016/j.neuchi.2017.03.001
Vandenbroucke JP, von Elm E, Altman DG et al (2007) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 4(10):e297. https://doi.org/10.1371/journal.pmed.0040297
Author information
Authors and Affiliations
Contributions
The contributions of each author to this study are as follows:
Guillaume Baucher: design, data collecting, statistics, writing.
Lucas Troude: design, proofreading.
Talal Al-Shabibi: proofreading.
Valentin Avinens: proofreading.
Sara Fernandes: statistics, proofreading.
Pierre-Hugues Roche: design, supervision, proofreading.
Corresponding author
Ethics declarations
Ethics approval
The protocol has been approved by the ethics committee of the French College of Neurosurgery (IRB00011687 #1: 2022/33).
Consent to participate
Informed and signed consent was obtained from all patients included in this study.
Consent for publication
All authors have given their consent for the publication of this research article.
Conflict of interest
The authors declare no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comments
The authors have undertaken a review of 32 cases of patients with spheno-orbital meningiomas at their institution over a 20-year period. They note in particular the evolution of proptosis following treatment in these cases. Proptosis improvement was seen in 75% of cases with worsening in a minority. The authors have made an important observation and identified BMI as a risk for lack of improvement (although not statistically significant) in proptosis which indicates multifactorial factors resulting in proptosis in these patients. Ultimately, the most important cause of proptosis is the reduction in orbital volume as a result of tumor invasion or compression of the orbit, and likely venous hypertension which may be the result of orbital involvement and cavernous sinus involvement. Adequate surgical resection thus may not result in reversal of proptosis. The authors should be commended for sharing their insights and experience with these difficult tumors.
William T. Couldwell
Salt Lake City, UT.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baucher, G., Troude, L., Al-Shabibi, T. et al. Predictive factors of the postoperative proptosis recovery in surgery of spheno-orbital meningiomas. Acta Neurochir 166, 164 (2024). https://doi.org/10.1007/s00701-024-06053-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06053-7