Abstract
Background
Bleeding of brainstem cavernous malformations (BSCM) cause high morbidity and should be treated surgically whenever possible.
Method
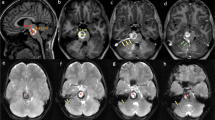
We present a 56-year-old man, who was diagnosed with a BSCM at right pons, which caused functional impairments of dorsal column, spinothalamic tract, cochlear nucleus, and middle cerebellar peduncle. A transmastoid presigmoid retorlabyrinthine approach via the lateral pontine zone (LPZ), with an assistance of imaging guidance and intraoperative neurophysiological monitoring, was performed to completely resect the BSCM. The patient recovered despite a transient worsening of cerebellar sign and hemiparesthesia for 1 week, without surgical complications.
Conclusions
A transmastoid presigmoid retrolabyrinthine approach through LPZ is safe and effective for lateral pontine BSCM resection.




Similar content being viewed by others
Abbreviations
- BSCM:
-
Brainstem cavernous malformation
- CPA:
-
Cerebellopontine angle
- CSF:
-
Cerebrospinal fluid
- CN:
-
Cranial nerve
- CT:
-
Computed tomography
- IONM:
-
Intraoperative neurophysiological monitoring
- LPZ:
-
Lateral pontine zone
- MRI:
-
Magnetic resonance imaging
- SCC:
-
Semicircular canal
References
Agrawal SK, Parnes LS (2008) Transmastoid superior semicircular canal occlusion. Otol Neurotol 29:363–367. https://doi.org/10.1097/mao.0b013e3181616c9d
Bento RF, De Brito RV, Sanchez TG, Miniti A (2002) The transmastoid retrolabyrinthine approach in vestibular schwannoma surgery. Otolaryngol Head Neck Surg 127:437–441. https://doi.org/10.1067/mhn.2002.129824
Cavalcanti DD, Preul MC, Kalani MY, Spetzler RF (2016) Microsurgical anatomy of safe entry zones to the brainstem. J Neurosurg 124:1359–1376. https://doi.org/10.3171/2015.4.JNS141945
Garcia RM, Ivan ME, Lawton MT (2015) Brainstem cavernous malformations: surgical results in 104 patients and a proposed grading system to predict neurological outcomes. Neurosurgery 76:265–277; discussion 277-268. https://doi.org/10.1227/NEU.0000000000000602
Giliberto G, Lanzino DJ, Diehn FE, Factor D, Flemming KD, Lanzino G (2010) Brainstem cavernous malformations: anatomical, clinical, and surgical considerations. Neurosurg Focus 29:E9. https://doi.org/10.3171/2010.6.FOCUS10133
Kalani MY, Yagmurlu K, Martirosyan NL, Cavalcanti DD, Spetzler RF (2016) Approach selection for intrinsic brainstem pathologies. J Neurosurg 125:1596–1607. https://doi.org/10.3171/2016.6.JNS161043
Kearns KN, Chen CJ, Tvrdik P, Park MS, Kalani MYS (2019) Outcomes of surgery for brainstem cavernous malformations: a systematic review. Stroke 50:2964–2966. https://doi.org/10.1161/STROKEAHA.119.026120
Rhoton AL (2003) Rhoton cranial anatomy and surgical approaches. Lippincott Williams & Wilkins, Philadelphia
Wong AK, Stamates MM, Bhansali AP, Shinners M, Wong RH (2017) Radiographic assessment of the presigmoid retrolabyrinthine approach. Surg Neurol Int 8:129. https://doi.org/10.4103/sni.sni_243_16
Xie MG, Li D, Guo FZ, Zhang LW, Zhang JT, Wu Z, Meng GL, Xiao XR (2018) Brainstem cavernous malformations: surgical indications based on natural history and surgical outcomes. World Neurosurg 110:55–63. https://doi.org/10.1016/j.wneu.2017.10.121
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Patient consent
The patient has consented to the submission of this How I Do It for submission to the journal.
Additional information
Summary of 10 Key Points
1. Transmastoid presigmoid retrolabyrinthine approach is the shortest route and provide direct approach to lateral pontine zone of brainstem.
2. Lateral pontine zone is a safe entry zone to resect lateral pontine lesions.
3. Transmastoid approach without a need of craniotomy is efficient and effective in selected cases.
4. Neuronavigation system incorporating with high resolution CT (temporal bone) and brain MRI provides valuable anatomical information in petrosal approach for BSCMs.
5. Intraoperative neurophysiological monitoring provides valuable physiological information before, during, and after BSCM removal.
6. Temporalis fascia graft is useful to close presigmoid dura defect.
7. Tissue glue provides extra-support to prevent CSF leakage.
8. Bone wax should be used to cover the drilled rough surface of petrous bone.
9. A generous fat graft should be harvested to plug into the drilled aeration dead space, which provides support to dura graft and decreases risk of CSF leakage and CNS infection.
10. A cosmetic mastoid cortical bone reconstruction is suggested.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgical technique evaluation
Electronic supplementary material
ESM 1
Photos taken by neuronavigation system after dura was opened. (A) Bone window of brain CT confirmed the location of semicircular canal and a retrolabyrinthe approach. (B) Brain MRI confirmed the LPZ, which provides the shortest distance to the cavernoma. (PNG 984 kb)
ESM 2
Subcortical motor evoked potential for detecting fiber tracts of CN6,7 (upper 2 rows), upper limbs (middle 2 rows) and lower limbs (lower 2 rows). No active response could be generated by 3 mA stimulation; while all except anterior tibialis muscle response could be generated by 5 mA stimulation. (PNG 495 kb)
ESM 3
Left upper limb somatosensory evoked potential did not change through the whole surgery (upper graph). Bilateral auditory brainstem response (ABR) shows a decline of ABR at right side before entering into pons, suggesting a decrease of cochlear function resulted from bleeding cavernoma, and the waveform did not change bilaterally through the whole surgery (lower graph). (PNG 558 kb)
Rights and permissions
About this article
Cite this article
Yeh, YC., Wei, KC. & Chen, KT. Transmastoid presigmoid retrolabyrinthine approach for removal of pontine cavernous malformation: how I do it. Acta Neurochir 162, 1131–1135 (2020). https://doi.org/10.1007/s00701-020-04263-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04263-3