Abstract
Background
The surgical removal of the infratemporal parapharyngeal lesions (IPL) is challenging due to its anatomical complexity. Previous surgical approaches have often been too invasive and necessitated sacrifice of normal function and anatomical structures, particularly in the retromandibular nerve region. Therefore, we sought to identify an approach corridor to this area that requires less sacrifice and report an innovative approach through a retromandibular fossa route to the IPL.
Methods
Five cadaveric specimens were dissected bilaterally with a trans-tympanic plate and styloid process approach. These specimens were investigated microanatomically and morphometrically to examine the extent of the approach in the parapharyngeal space. The clinical application of this approach was compared to previous approaches to the IPL used in our clinical series of 20 cases.
Results
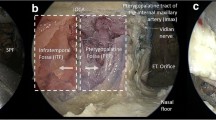
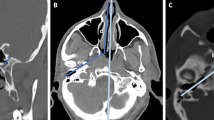
Using this novel approach, the inferior alveolar nerve was identified in all specimens, while the chorda tympani and lingual nerve were identified in 6 (60%) and 4 (40%) dissections, respectively. In all specimens, the petrous portion of the internal carotid artery and the exit of the lower cranial nerve were identified. The average length of the exposed lower cranial nerves was 16.6 ± 3.8 mm (range: 11–25 mm).
Conclusions
The described approach is feasible for accessing the IPL at the retromandibular nerve and is less invasive than conventionally used approaches.





Similar content being viewed by others
Abbreviations
- EAC:
-
External auditory canal
- FN:
-
Facial nerve
- ICA:
-
Internal carotid artery
- IPL:
-
Infratemporal parapharyngeal lesions
- ITF:
-
Infratemporal fossa
- ITR:
-
Inferior tympanic ring
- PS:
-
Parapharyngeal space
- SP:
-
Styloid process
- TMJ:
-
Temporomandibular joint
- TP:
-
Tympanic plate
- TTSA:
-
Trans-tympanic plate and styloid process approach
References
Ahn D, Sohn JH, Lee GJ (2018) Feasibility of a new V-shaped incision for parotidectomy: a preliminary report. Br J Oral Maxillofac Surg 56:406–410. https://doi.org/10.1016/j.bjoms.2018.03.014
Battaglia P, Turri-Zanoni M, Dallan I, Gallo S, Sica E, Padoan G, Castelnuovo P (2014) Endoscopic endonasal transpterygoid transmaxillary approach to the infratemporal and upper parapharyngeal tumors. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 150:696–702. https://doi.org/10.1177/0194599813520290
Beswick DM, Vaezi A, Caicedo-Granados E, Duvvuri U (2012) Minimally invasive surgery for parapharyngeal space tumors. Laryngoscope 122:1072–1078. https://doi.org/10.1002/lary.23244
Blumberg JM, Judson BL (2014) Surgical management of parapharyngeal space infections. Oper Tech Otolaryngol Head Neck Surg 25:304–309. https://doi.org/10.1016/j.otot.2014.04.014
Carrau RL, Myers EN, Johnson JT (1990) Management of tumors arising in the parapharyngeal space. Laryngoscope 100:583–589. https://doi.org/10.1288/00005537-199006000-00006
Cassetta M, Barchetti F, Pranno N, Barchetti G, Fioravanti C, Stagnitti A, Rubini A, Fioravanti E, Saccoliti E, Elia D, Rossignuolo M, Russo C, Cantisani V, D'Andrea V (2014) High resolution 3-T MR imaging in the evaluation of the facial nerve course. Il Giornale di chirurgia 35:15–19
Coste A, Dessi P, Serrano E (2012) Empty nose syndrome. Eur Ann Otorhinolaryngol Head Neck Dis 129:93–97. https://doi.org/10.1016/j.anorl.2012.02.001
Duek I, Sviri GE, Billan S, Gil Z (2018) Minimally invasive surgery for resection of parapharyngeal space tumors. J Neurol Surg B Skull Base 79:250–256. https://doi.org/10.1055/s-0037-1607315
Ferrari M, Schreiber A, Mattavelli D, Lombardi D, Rampinelli V, Doglietto F, Rodella LF, Nicolai P (2018) Surgical anatomy of the parapharyngeal space: a multiperspective, quantification-based study. Head & neck. https://doi.org/10.1002/hed.25378
Fisch U (1978) Infratemporal fossa approach to tumours of the temporal bone and base of the skull. J Laryngol Otol 92:949–967
He H, Yang Q, Gong J, Luo L, Huang T, Chen Z, Guo Y, Li W (2018) Endoscopic transvestibular transmandibular approach for trigeminal schwannoma in infratemporal fossa and parapharyngeal space. World neurosurgery 118:172–176. https://doi.org/10.1016/j.wneu.2018.07.087
Izci Y, Moftakhar R, Pyle M, Baskaya MK (2008) Retromandibular fossa approach to the high cervical internal carotid artery: an anatomic study. Neurosurgery 62:ONS363–ONS369; discussion 369-370. https://doi.org/10.1227/01.neu.0000326020.07187.6b
Joseph ST, Sharankumar S, Sandya CJ, Sivakumar V, Sherry P, Krishnakumar T, Subramania I (2015) Easy and safe method for facial nerve identification in parotid surgery. J Neurol Surg B Skull Base 76:426–431. https://doi.org/10.1055/s-0035-1549001
Judson BL, Adam SI, Lowlicht R, Bulsara KR (2012) Transcervical double mandibular osteotomy approach to the infratemporal fossa. World neurosurgery 78(715):e711–e715. https://doi.org/10.1016/j.wneu.2011.12.015
Kawakami S, Tsukada S, Taniguchi W (1994) The superficial temporal and retromandibular veins as guides to expose the facial nerve branches. Ann Plast Surg 32:295–299
Kiya N, Sawamura Y, Dureza C, Fukushima T (2000) Minimally invasive surgical exposure of the extreme high cervical internal carotid artery: anatomical study. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 7:438–444. https://doi.org/10.1054/jocn.1999.0241
Kohno S, Kohno T, Medina RU (2001) Rotational head motion concurrent to rhythmical mandibular opening movements. J Oral Rehabil 28:740–747
Kuet ML, Kasbekar AV, Masterson L, Jani P (2015) Management of tumors arising from the parapharyngeal space: a systematic review of 1,293 cases reported over 25 years. Laryngoscope 125:1372–1381. https://doi.org/10.1002/lary.25077
Kwak HH, Park HD, Youn KH, Hu KS, Koh KS, Han SH, Kim HJ (2004) Branching patterns of the facial nerve and its communication with the auriculotemporal nerve. Surgical and radiologic anatomy : SRA 26:494–500. https://doi.org/10.1007/s00276-004-0259-6
Levitt GW (1970) Cervical fascia and deep neck infections. Laryngoscope 80:409–435. https://doi.org/10.1288/00005537-197003000-00004
Li C, Li Y, Zhang D, Yang Z, Wu L (2012) 3D-FIESTA MRI at 3 T demonstrating branches of the intraparotid facial nerve, parotid ducts and relation with benign parotid tumours. Clin Radiol 67:1078–1082. https://doi.org/10.1016/j.crad.2012.03.014
Martinez Pascual P, Maranillo E, Vazquez T, Simon de Blas C, Lasso JM, Sanudo JR (2018) Extracranial Course of the Facial Nerve Revisited. Anatomical record (Hoboken, NJ : 2007). doi:https://doi.org/10.1002/ar.23825
Nonaka Y, Fukushima T, Watanabe K, Sakai J, Friedman AH, Zomorodi AR (2016) Middle infratemporal fossa less invasive approach for radical resection of parapharyngeal tumors: surgical microanatomy and clinical application. Neurosurg Rev 39:87–96; discussion 96-87. https://doi.org/10.1007/s10143-015-0655-x
Ohue S, Fukushima T, Kumon Y, Ohnishi T, Friedman AH (2012) Preauricular transzygomatic anterior infratemporal fossa approach for tumors in or around infratemporal fossa lesions. Neurosurg Rev 35:583–592; discussion 592. https://doi.org/10.1007/s10143-012-0389-y
Olsen KD (1994) Tumors and surgery of the parapharyngeal space. Laryngoscope 104:1–28
Pilolli F, Giordano L, Galli A, Bussi M (2016) Parapharyngeal space tumours: video-assisted minimally invasive transcervical approach. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale 36:259–264. https://doi.org/10.14639/0392-100x-709
Pradhan P, Preetam C, Parida PK, Samal S, Samal DK (2018) Surgical management of parapharyngeal space tumours in a single tertiary care center. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India 70:531–537. https://doi.org/10.1007/s12070-018-1447-8
Prasad SC, Piccirillo E, Chovanec M, La Melia C, De Donato G, Sanna M (2015) Lateral skull base approaches in the management of benign parapharyngeal space tumors. Auris Nasus Larynx 42:189–198. https://doi.org/10.1016/j.anl.2014.09.002
Schwartz TR, Colletta MD, McCormick ME (2018) Transcanal incision and drainage of a parapharyngeal abscess in a pediatric patient: a novel technique. Int J Pediatr Otorhinolaryngol 112:80–81. https://doi.org/10.1016/j.ijporl.2018.06.033
Smith RJ (1985) Functions of condylar translation in human mandibular movement. Am J Orthod 88:191–202
Sun X, Yan B, Truong HQ, Borghei-Razavi H, Snyderman CH, Fernandez-Miranda JC (2018) A comparative analysis of endoscopic-assisted transoral and transnasal approaches to parapharyngeal space: a cadaveric study. J Neurol Surg B Skull Base 79:229–240. https://doi.org/10.1055/s-0037-1606551
Takezawa K, Townsend G, Ghabriel M (2018) The facial nerve: anatomy and associated disorders for oral health professionals. Odontology 106:103–116. https://doi.org/10.1007/s10266-017-0330-5
Terasaka S, Sawamura Y, Goto S, Fukushima T (1999) A lateral transzygomatic-transtemporal approach to the infratemporal fossa: technical note for mobilization of the second and third branches of the trigeminal nerve. Skull base surgery 9:277–287
Valentini V, Giovannetti F, Priore P, Raponi I, Terenzi V, Cassoni A (2015) Mini invasive transoral approach to the glenoid fossa: benign lesion removal using endoscopy. Laryngoscope 125:2054–2057. https://doi.org/10.1002/lary.25191
Vrionis FD, Cano WG, Heilman CB (1996) Microsurgical anatomy of the infratemporal fossa as viewed laterally and superiorly. Neurosurgery 39:777–785 discussion 785-776
Acknowledgments
The authors thank Mrs. Lori Radcliffe for managing our investigation and Prof. Allan H. Friedman and Prof. John H. Sampson for providing the research opportunity. We would like to thank Mr. Shawn Mullin and Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgical Anatomy
Electronic supplementary material
Video 1
Illustration of the steps involved in the cadaveric dissection. CN IX = glossopharyngeal nerve; CN X = vagus nerve; XI = accessory nerve; EAC = external auditory canal; FN = facial nerve; PS = parapharyngeal space (MOV 282491 kb)
Rights and permissions
About this article
Cite this article
Sato, H., Nonaka, Y., Bawornvaraporn, U. et al. Preauricular retromandibular trans tympanic plate and styloid process keyhole approach to parapharyngeal lesions: a laboratory study. Acta Neurochir 162, 661–669 (2020). https://doi.org/10.1007/s00701-020-04217-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04217-9