Abstract
Objective
The purpose of this study was to compare the effects of single and dual nerve transfer for the repair of shoulder abduction in patients with upper or upper and middle trunk root avulsion.
Methods
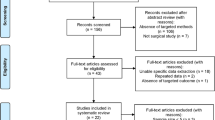
We carried out a retrospective analysis of 20 patients with C5-C6 or C5-C7 root avulsion treated by nerve transfer in our hospital. The patients were divided into two groups according to the different operation methods. In group A, ten patients had transferred the spinal accessory nerve to the suprascapular nerve. Ten patients in group B underwent dual nerve transfer to reconstruct shoulder abduction, including the spinal accessory nerve transfer to the suprascapular nerve and two intercostal nerves or the long head of triceps nerve branch transfer to the anterior branch of the axillary nerve. There was no difference in age, preoperative interval, follow-up time, and injury type between the two groups. We used shoulder abduction strength, shoulder abduction angle, and Samardzic’s shoulder joint evaluation standard as the postoperative evaluation index. Shoulder abductor muscle strength equals or above M3 was considered to be an effective recovery.
Results
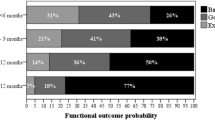
Of the 20 cases, 15 obtained equals or more M3 of shoulder abduction strength, and the overall effective rate was 75%. The effective rate of shoulder abduction power in group A was 60% (6/10) while group B was 90% (9/10); however, the difference was not statistically significant (p > 0.05). The average shoulder abduction angle was 55° (SD = 19.29) in group A and 77° (SD = 20.44) in group B; the angle was significantly better in group B than that in group A (p < 0.05). Based on Samardzic’s standard, the excellent and good rate of group A was 90% and in group B was 50%. The difference was statistically significant (p < 0.05).
Conclusion
For patients with nerve root avulsion of C5-C6 or C5-C7, repairing suprascapular nerve and axillary nerve at the same time is more effective than repairing suprascapular nerve alone in terms of shoulder abduction angle and excellent rate of functional recovery of the shoulder joint. Therefore, we recommend the repair of the suprascapular nerve and the axillary nerve simultaneously if conditions permit.
Similar content being viewed by others
References
Baltzer HL, Wagner ER, Kircher MF, Spinner RJ, Bishop AT, Shin AY (2017) Evaluation of infraspinatus reinnervation and function following spinal accessory nerve to suprascapular nerve transfer in adult traumatic brachial plexus injuries. Microsurgery 37:365–370
Bertelli JA, Tacca CP, Winkelmann DE, Ghizoni MF, Duarte H (2011) Transfer of axillary nerve branches to reconstruct elbow extension in tetraplegics: a laboratory investigation of surgical feasibility. Microsurgery 31:376–381
Cardenas-Mejia A, O’Boyle CP, Chen KT, Chuang DC (2008) Evaluation of single-, double-, and triple-nerve transfers for shoulder abduction in 90 patients with supraclavicular brachial plexus injury. Plast Reconstr Surg 122:1470–1478
Chu B, Wang H, Chen L, Gu Y, Hu S (2016) Dual nerve transfers for restoration of shoulder function after brachial plexus avulsion injury. Ann Plast Surg 76:668–673
Chuang DC (2009) Adult brachial plexus reconstruction with the level of injury: review and personal experience. Plast Reconstr Surg 124:e359–e369
Emamhadi M, Alijani B, Andalib S (2016) Long-term clinical outcomes of spinal accessory nerve transfer to the suprascapular nerve in patients with brachial plexus palsy. Acta Neurochir 158:1801–1806
Gao KM, Hu JJ, Lao J, Zhao X (2018) Evaluation of nerve transfer options for treating total brachial plexus avulsion injury: a retrospective study of 73 participants. Neural Regen Res 13:470–476
Gillis JA, Khouri JS, Kircher MF, Spinner RJ, Bishop AT, Shin AY (2018) Outcomes of shoulder abduction after nerve surgery in patients over 50 years following traumatic brachial plexus injury. J Plast Reconstr Aesthet Surg
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected] The Upper Extremity Collaborative Group (UECG). Am J Ind Med 29:602–608
Leechavengvongs S, Malungpaishorpe K, Uerpairojkit C, Ng CY, Witoonchart K (2016) Nerve transfers to restore shoulder function. Hand Clin 32:153–164
Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P (2003) Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part II: a report of 7 cases. J Hand Surg Am 28:633–638
Malungpaishrope K, Leechavengvongs S, Witoonchart K, Uerpairojkit C, Boonyalapa A, Janesaksrisakul D (2012) Simultaneous intercostal nerve transfers to deltoid and triceps muscle through the posterior approach. J Hand Surg Am 37:677–682
Merrell GA, Barrie KA, Katz DL, Wolfe SW (2001) Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg Am 26:303–314
Samardzic M, Grujicic D, Rasulic L, Bacetic D (2002) Transfer of the medial pectoral nerve: myth or reality? Neurosurgery 50:1277–1282
Schreiber JJ, Byun DJ, Khair MM, Rosenblatt L, Lee SK, Wolfe SW (2015) Optimal axon counts for brachial plexus nerve transfers to restore elbow flexion. Plast Reconstr Surg 135:135e–141e
Terzis JK, Barmpitsioti A (2010) Axillary nerve reconstruction in 176 posttraumatic plexopathy patients. Plast Reconstr Surg 125:233–247
Vanaclocha V, Herrera JM, Rivera-Paz M, Martinez-Gomez D, Vanaclocha L (2018) Radial to axillary nerve transfer. Neurosurg Focus 44:V1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Comments
The authors reviewed their results in restoring shoulder abduction in 20 patients with upper brachial plexus injuries. 10 of the patients were treated with spinal accessory to suprascapular nerve transfers and 10 of the patients had spinal accessory to suprascapular nerve transfers along with neurotization of the anterior branch of the axillary nerve. The authors found that the double repair provided superior results. I don’t think that these findings are particularly surprising to surgeons who regularly do brachial plexus repair surgery. Neurotization of the axillary nerve using a branch of the radial nerve to the long head of the triceps has been a part of the surgeon’s armanentarium for some time. I did find it very interesting that the patients seem to be afforded a good result from transferring intercostal nerves to the axillary nerve. In my practice if the patient did not have sufficient triceps strength, abduction of the shoulder was treated with a single anastomosis from the spinal accessory nerve to the suprascapular nerve. The next time I see such a patient I will supplement that single anastomosis with an intercostal to axillary nerve anastomosis.
Allan Friedman
NC, USA
There is an extensive literature demonstrating that repairing both the suprascapular and axillary nerves to restore function to the supraspinatus and deltoid muscles respectively, the major abductors of the arm at the shoulder, results in improved function as opposed to one or the other. This article confirms this observation in the setting of patients with brachial plexus nerve root avulsion injuries involving either the C5 and C6 levels or the C5, C6, and C7 levels using nerve transfers. In one group of 10 patients (single transfer), only the suprascapular nerve was repaired by directly transferring the distal spinal accessory nerve. In the other group of 10 patients (double transfer) in addition the anterior branch of the axillary nerve was repaired using a direct transfer of the radial branch to the long of the triceps muscle in cases of C5 and C6 avulsions or two intercostal nerves in the setting of C5-7 avulsions. The results comparing these two groups when motor strength was assessed by the MRC grading scale did show an advantage for the double transfer group that was not statistically significant. Better range of arm abduction when measured in degrees was seen with the double transfer compared to the single transfer procedure that was statistically significant when assessed using the evaluation criteria of the shoulder joint proposed by Samardzic et al. Although other studies have shown a similar result and this is a retrospective study with relatively small numbers, it nonetheless provides useful confirmatory information on patients operated on by a single group.
Michel Kliot
CA, USA
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Peripheral Nerves
Rights and permissions
About this article
Cite this article
Xiao, F., Zhao, X. & Lao, J. Comparative study of single and dual nerve transfers for repairing shoulder abduction. Acta Neurochir 161, 673–678 (2019). https://doi.org/10.1007/s00701-019-03847-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-03847-y