Abstract
Background
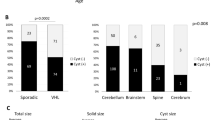
Hemangioblastomas (HB) are benign tumors of the central nervous system (CNS) that can appear sporadic or as part of von Hippel-Lindau (VHL) disease. It is often curable with surgical resection, but upon relapse, the disease exhibits a treatment-refractory course.
Case report
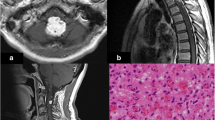
A patient treated for sporadic cerebellar HB relapsed 12 years post-surgery. She developed disseminated disease throughout the CNS, including leptomeningeal manifestations. Repeat surgery and craniospinal radiation therapy were unsuccessful.
Conclusion
This case is in line with previous publications on disseminated non-VHL HB. Available treatment options are inefficient, emphasizing the need for improved understanding of HB biology to identify therapeutic targets.




Similar content being viewed by others
References
Akimoto J, Fukuhara H, Suda T, Nagai K, Hashimoto R, Michihiro K (2014) Disseminated cerebellar hemangioblastoma in two patients without von Hippel-Lindau disease. Surg Neurol Int 5:145. https://doi.org/10.4103/2152-7806.142321
Amelot A, Bouazza S, Polivka M, George B, Bresson D (2015) Sporadically second localization of cerebellar hemangioblastoma in sella turcica mimicking a meningioma with no associated von Hippel-Lindau disease. Br J Neurosurg 29:589–591. https://doi.org/10.3109/02688697.2015.1016894
Böhling T, Plate K, Haltia M, Litalo K, Neumann H (2000) von Hippel-Lindau disease and capillary haemangioblastoma in World Health Organization Classification of Tumors Pathology, genetics of tumours of the nervous system. 223–6 edn., Lyon
Bruner J, Tien R, McLendon R (1998) Tumors of vascular origin. In Russel and Rubinstein’s pathology of tumors of the nervous system. 6th edn., London
Choyke PL, Glenn GM, Walther MM, Patronas NJ, Linehan WM, Zbar B (1995) von Hippel-Lindau disease: genetic, clinical, and imaging features. Radiology 194:629–642. https://doi.org/10.1148/radiology.194.3.7862955
Chung SY, Jeun SS, Park JH (2014) Disseminated hemangioblastoma of the central nervous system without von Hippel-Lindau disease. Brain Tumor Res Treat 2:96–101. https://doi.org/10.14791/btrt.2014.2.2.96
de la Monte SM, Horowitz SA (1989) Hemangioblastomas: clinical and histopathological factors correlated with recurrence. Neurosurgery 25:695–698
Gijtenbeek JM, Jacobs B, Sprenger SH, Eleveld MJ, van Kessel AG, Kros JM, Sciot R, van Calenbergh F, Wesseling P, Jeuken JW (2002) Analysis of von hippel-Lindau mutations with comparative genomic hybridization in sporadic and hereditary hemangioblastomas: possible genetic heterogeneity. J Neurosurg 97:977–982. https://doi.org/10.3171/jns.2002.97.4.0977
Girmens JF, Erginay A, Massin P, Scigalla P, Gaudric A, Richard S (2003) Treatment of von Hippel-Lindau retinal hemangioblastoma by the vascular endothelial growth factor receptor inhibitor SU5416 is more effective for associated macular edema than for hemangioblastomas. Am J Ophthalmol 136:194–196
Hande AM, Nagpal RD (1996) Cerebellar haemangioblastoma with extensive dissemination. Br J Neurosurg 10:507–511
Hasselblatt M, Jeibmann A, Gerss J, Behrens C, Rama B, Wassmann H, Paulus W (2005) Cellular and reticular variants of haemangioblastoma revisited: a clinicopathologic study of 88 cases. Neuropathol Appl Neurobiol 31:618–622
Kato M, Ohe N, Okumura A, Shinoda J, Nomura A, Shuin T, Sakai N (2005) Hemangioblastomatosis of the central nervous system without von Hippel-Lindau disease: a case report. J Neuro-Oncol 72:267–270. https://doi.org/10.1007/s11060-004-2244-7
Kim HR, Suh YL, Kim JW, Lee JI (2009) Disseminated hemangioblastomatosis of the central nervous system without von Hippel-Lindau disease: a case report. J Korean Med Sci 24:755–759. https://doi.org/10.3346/jkms.2009.24.4.755
Kruizinga RC, van Marion DM, den Dunnen WF, de Groot JC, Hoving EW, Oosting SF, Timmer-Bosscha H, Derks RP, Cornelissen C, van der Luijt RB, Links TP, de Vries EG, Walenkamp AM (2016) Difference in CXCR4 expression between sporadic and VHL-related hemangioblastoma. Familial Cancer 15:607–616. https://doi.org/10.1007/s10689-016-9879-3
Lee JY, Dong SM, Park WS, Yoo NJ, Kim CS, Jang JJ, Chi JG, Zbar B, Lubensky IA, Linehan WM, Vortmeyer AO, Zhuang Z (1998) Loss of heterozygosity and somatic mutations of the VHL tumor suppressor gene in sporadic cerebellar hemangioblastomas. Cancer Res 58:504–508
Lightfoot NJ, Lucas PG, Finnis ND (2007) Disseminated haemangioblastoma without evidence of the von Hippel-Lindau syndrome or haemangioblastomatosis--a case report and clinico-pathological correlation. Clin Neurol Neurosurg 109:305–310. https://doi.org/10.1016/j.clineuro.2006.12.007
Mandahl N (1992) Human cytogenetics - a practical approach: Vol. II. Malignancy and acquired abnormalities, vol II. IRL Press, Oxford
Mohan J, Brownell B, Oppenheimer DR (1976) Malignant spread of haemangioblastoma: report on two cases. J Neurol Neurosurg Psychiatry 39:515–525
Muscarella LA, Bisceglia M, Galliani CA, Zidar N, Ben-Dor DJ, Pasquinelli G, la Torre A, Sparaneo A, Fanburg-Smith JC, Lamovec J, Michal M, Bacchi CE (2018) Extraneuraxial hemangioblastoma: a clinicopathologic study of 10 cases with molecular analysis of the VHL gene. Pathol Res Pract 214:1156–1165. https://doi.org/10.1016/j.prp.2018.05.007
Niemela M, Maenpaa H, Salven P, Summanen P, Poussa K, Laatikainen L, Jaaskelainen J, Joensuu H (2001) Interferon alpha-2a therapy in 18 hemangioblastomas. Clin Cancer Res 7:510–516
Omar AI (2012) Bevacizumab for the treatment of surgically unresectable cervical cord hemangioblastoma: a case report. J Med Case Rep 6:238. https://doi.org/10.1186/1752-1947-6-238
Raghavan R, Krumerman J, Rushing EJ, White CL III, Chason DP, Watson ML, Coimbra C (2000) Recurrent (nonfamilial) hemangioblastomas involving spinal nerve roots: case report. Neurosurgery 47:1443–1448
Ramachandran R, Lee HS, Matthews B, Shatzel A, Tihan T (2008) Intradural extramedullary leptomeningeal hemangioblastomatosis and paraneoplastic limbic encephalitis diagnosed at autopsy: an unlikely pair. Arch Pathol Lab Med 132:104–108. https://doi.org/10.1043/1543-2165(2008)132[104:IELHAP]2.0.CO;2
Russell DS, Rubinstein LJ (1989) Pathology of tumours of the nervous system. 5th edn., London
Seystahl K, Weller M, Bozinov O, Reimann R, Rushing E (2014) Neuropathological characteristics of progression after prolonged response to bevacizumab in multifocal hemangioblastoma. Oncol Res Treat 37:209–212
International Standing Committee on Human Cytogenetic Nomenclature, Shaffer LG, Slovak ML, Campbell LJ (2009) ISCN 2009: an international system for human cytogenetic nomenclature. Karger, Basel; Unionville, CT
Shankar GM, Taylor-Weiner A, Lelic N, Jones RT, Kim JC, Francis JM, Abedalthagafi M, Borges LF, Coumans JV, Curry WT, Nahed BV, Shin JH, Paek SH, Park SH, Stewart C, Lawrence MS, Cibulskis K, Thorner AR, Van Hummelen P, Stemmer-Rachamimov AO, Batchelor TT, Carter SL, Hoang MP, Santagata S, Louis DN, Barker FG, Meyerson M, Getz G, Brastianos PK, Cahill DP (2014) Sporadic hemangioblastomas are characterized by cryptic VHL inactivation. Acta neuropathologica communications 2:167. https://doi.org/10.1186/s40478-014-0167-x
Taieb D, Barlier A, Yang C, Pertuit M, Tchoghandjian A, Rochette C, Zattara-Canoni H, Figarella-Branger D, Zhuang Z, Pacak K, Metellus P (2016) Somatic gain-of-function HIF2A mutations in sporadic central nervous system hemangioblastomas. J Neuro-Oncol 126:473–481. https://doi.org/10.1007/s11060-015-1983-y
Takayanagi S, Mukasa A, Tanaka S, Nomura M, Omata M, Yanagisawa S, Yamamoto S, Ichimura K, Nakatomi H, Ueki K, Aburatani H, Saito N (2017) Differences in genetic and epigenetic alterations between von Hippel-Lindau disease-related and sporadic hemangioblastomas of the central nervous system. Neuro-Oncology 19:1228–1236. https://doi.org/10.1093/neuonc/nox034
Tohyama T, Kubo O, Kusano R, Miura N, Himuro H (1990) A case of hemangioblastoma with subarachnoid dissemination. No Shinkei Geka 18:83–88
Weil RJ, Vortmeyer AO, Zhuang Z, Pack SD, Theodore N, Erickson RK, Oldfield EH (2002) Clinical and molecular analysis of disseminated hemangioblastomatosis of the central nervous system in patients without von Hippel-Lindau disease. Report of four cases. J Neurosurg 96:775–787. https://doi.org/10.3171/jns.2002.96.4.0775
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The patient has consented to the writing and submission of the case report. The interpretation and reporting of this case is the sole responsibility of the authors. The case report has been written in accordance with COPE guidelines and comply with the CARE statement. There are no conflicts of interests for any of the contributing authors. No portion of this case report has been presented or published previously.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain Tumors
Rights and permissions
About this article
Cite this article
Bains, S.J., Niehusmann, P.F., Meling, T.R. et al. Disseminated central nervous system hemangioblastoma in a patient with no clinical or genetic evidence of von Hippel-Lindau disease—a case report and literature review. Acta Neurochir 161, 343–349 (2019). https://doi.org/10.1007/s00701-019-03800-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-03800-z