Abstract
Background
Dynamic magnetic resonance imaging (MRI)-based criteria for diagnosing magnitude of tethered cord syndrome (TCS) in occult spinal dysraphism are proposed.
Methods
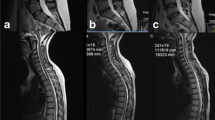
In this prospective, case-control design study, MRI lumbosacral spine was performed in 51 subjects [pilot group (n = 10) without TCS (for defining radiological parameters), control group (n = 10) without TCS (for baseline assessment), and study group (n = 31) with spinal dysraphism (thick filum terminale [n = 12], lumbar/lumbosacral meningomyelocoele [n = 6], and lipomyelomeningocoele [n = 13])]. The parameters compared in control and study groups included oscillatory frequency (OF), difference in ratio, in supine/prone position, of distance between posterior margin of vertebral body and anterior margin of spinal cord (oscillatory distance [OD]), with canal diameter, at the level of conus as well as superior border of contiguous two vertebrae above that level; delta bending angle (ΔBA), difference, in supine/prone position, of angle between longitudinal axis of conus and that of lower spinal cord; and sagittal and axial root angles, subtended between exiting ventral nerve roots and longitudinal axis of cord. An outcome assessment at follow-up was also done.
Results
In the study group (cord tethered), significantly less movement at the level of conus (OF0, p = 0.013) and one level above (OF1, p = 0.03) and significant difference in ΔBA (p = 0.0) were observed in supine and prone positions, compared to controls. Ventral nerve root stretching resulted in sagittal/axial root angle changes. Median OF (0.04) in the lipomyelomeningocoele group was significantly less than that in control group (0.23). Median OF was also lesser in patients with thick filum terminale or meningomyelocele. Difference in median sagittal and axial root angles among the study and control groups was statistically significant (p = 0.00).
Conclusion
New dynamic MRI-based parameters to establish the presence and magnitude of TCS have been defined. OF measured the extent of loss of translational cord displacement in supine and prone positions; ΔBA defined the relative angulation of conus with lower spinal cord, and sagittal and axial root angles represented ventral nerve root stretching. The difference in OF or ΔBA was minimum in the group with thick filum terminale and progressively increased in the groups with lipomyelomeningocele and meningomyelocele.







Similar content being viewed by others
References
Akgun B, Ozturk S, Ucer O, Erol FS (2017) Intradural sacral mature teratoma associated with a low-lying conus. Neurol India 65(1):216–217
Alamdaran SA, Mohammadpanah N, Zabihian S, Esmaeeli M, Ghane F, Feyzi A (2017) Diagnostic value of ultrasonography in spinal abnormalities among children with neurogenic bladder. Electronic Physician 9(6):4571–4576
Brunelle F, Sebag G, Baraton J, Carteret M, Martinat P, Pierre-Kahn A (1996) Lumbar spinal cord motion measurement with phase-contrast MR imaging in normal children and in children with spinal lipomas. Pediatr Radiol 26(4):265–270
Dadlani R, Atal AA (2017) Occult sacral meningocoele associated with spinal dysraphism: report of an unusual case and a review of literature. Neurol India 65(2):414–416
Filippidis AS, Kalani MY, Theodore N, Rekate HL (2010) Spinal cord traction, vascular compromise, hypoxia, and metabolic derangements in the pathophysiology of tethered cord syndrome. Neurosurg Focus 29(1):E9
Garg K, Tandon V, Kumar R, Sharma BS, Mahapatra AK (2014) Management of adult tethered cord syndrome: our experience and review of literature. Neurol India 62(2):137–143
Hertzler DA, DePowell JJ, Stevenson CB, Mangano FT (2010) Tethered cord syndrome: a review of the literature from embryology to adult presentation. Neurosurg Focus 29(1):E1. https://doi.org/10.3171/2010.3.FOCUS1079
Hricak H, Amparo EG (1984) Body MRI: alleviation of claustrophobia by prone positioning. Radiology 152(3):819
Huang SL, Peng J, Yuan GL, Ding XY, He XJ, Lan BS (2015) A new model of tethered cord syndrome produced by slow traction. Sci Rep 13(5):9116. https://doi.org/10.1038/srep09116
Jokich PM, Rubin JM, Dohrmann GJ (1984) Intraoperative ultrasonic evaluation of spinal cord motion. J Neurosurg 60:707–711
Khoury AE, Hendrick EB, McLorie GA, Kulkarni A, Churchill BM (1990) Occult spinal dysraphism: clinical and urodynamic outcome after division of the filum terminale. J Urol 144:426–429
Krishnan P, Kartikueyan R, Chowdhury D, Saha M (2013) Ventral herniation of the dorsal spinal cord: a rare cause of myelopathy. Neurol India 61:453–454
Nakanishi K, Tanaka N, Kamei N, Nakamae T, Izumi B, Ohta R, Fujioka Y, Ochi M (2013) Use of prone position magnetic resonance imaging for detecting the terminal filum in patients with occult tethered cord syndrome. J Neurosurg Spine 18(1):76–84
Niggemann P, Sarikaya-Seiwert S, Beyer HK, Sobottke R (2011) Features of positional magnetic resonance imaging in tethered cord syndrome. Clin Neuroradiol 21(1):11–15
Raghavan N, Barkovich A, Edwards M, Norman D (1989) MR imaging in the tethered spinal cord syndrome. AJNR Am J Neuroradiol 10:27–36
Ranger MR, Irwin GJ, Bunbury KM, Peutrell JM (2008) Changing body position alters the location of the spinal cord within the vertebral canal: a magnetic resonance imaging study. Br J Anaesth 101(6):804–809
Rohrschneider WK, Forsting M, Darge K, Tröger J (1996) Diagnostic value of spinal US: comparative study with MR imaging in pediatric patients. Radiology 200(2):383–388
Sarwar M, Crelin ES, El K, Virapongse C (1983) Experimental cord stretchability and the tethered cord syndrome. AJNR 4:641–643
Schmidt DM, Robinson B, Jones DA (1990) The tethered spinal cord Etiology and clinical manifestations. Orthop Rev 19(10):870–876
Singh S, Kline-Fath B, Bierbrauer K, Racadio JM, Salisbury S, Macaluso M, Jackson EC, Egelhoff JC (2012) Comparison of standard, prone and cine MRI in the evaluation of tethered cord. Pediatr Radiol 42(6):685–691
Stamates MM, Frim DM, Yang CW, Katzman GL, Ali S (2018) Magnetic resonance imaging in the prone position and the diagnosis of tethered spinal cord. J Neurosurg Pediatr 21(1):4–10
Takiguchi T, Shigeki Y, Tezuka M, Kitajima T (2009) Measurement of shift of the cauda equina in the subarachnoid space by changing position. Reg Anesth Pain Med 34(4):326–329
Vernet O, O’Gorman AM, Farmer JP, McPhillips M, Montes JL (1996) Use of the prone position in the MRI evaluation of spinal cord retethering. Pediatr Neurosurg 25(6):286–294
Wilson DA, Prince JR (1989) MR imaging determination of the location of the normal conus medullaris throughout childhood. AJR Am J Roentgenol 152(5):1029–1032
Winklhofer S, Schoth F, Stolzmann P, Krings T, Mull M, Wiesmann M, Stracke CP (2014) Spinal cord motion: influence of respiration and cardiac cycle. RöFo 186(11):1016–1021
Yamada S, Won DJ (2007) What is the true tethered cord syndrome? Childs Nerv Syst 23:371–375
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Additional information
This article is part of the Topical Collection on Spine - Other
Rights and permissions
About this article
Cite this article
Singh, S., Behari, S., Singh, V. et al. Dynamic magnetic resonance imaging parameters for objective assessment of the magnitude of tethered cord syndrome in patients with spinal dysraphism. Acta Neurochir 161, 147–159 (2019). https://doi.org/10.1007/s00701-018-3721-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3721-7