Abstract
Background
Vancomycin and meropenem are frequently used as empiric treatment for ventriculitis. Penetration into the cerebrospinal fluid (CSF) depends on various factors with a high inter-individual variability. Because attaining and maintaining adequate concentrations of meropenem and vancomycin in the CSF is crucial for their bactericidal effect, we introduced a routine therapeutic drug monitoring (TDM) from CSF and serum for both antibiotics. We studied the antibiotic penetration into the CSF.
Methods
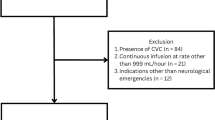
Patient data including serum and CSF concentrations for meropenem and vancomycin were collected in a retrospective fashion. Antibiotic CSF penetration ratio was calculated for each patient. Antibiotics were administered by continuous infusion aiming for serum target concentrations of 20–30 mg/L for vancomycin and 16–32 mg/L for meropenem.
Results
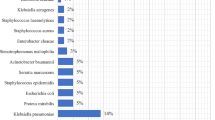
Twenty-two patients with 36 CSF/serum pairs for meropenem and 43 pairs for vancomycin were studied. No patient suffered from renal or liver insufficiency. Mean vancomycin serum concentration was 22 ± 8 mg/L and the mean CSF concentration 4.5 ± 2.6 mg/L. CSF penetration was 20 ± 11% (coefficient of determination (R2) 0.02). For meropenem, the mean serum concentration was 30.7 ± 14.9 mg/L, mean CSF concentration 5.5 ± 5.2 mg/L, and a penetration of 18 ± 12%, R2 = 0.42.
Conclusion
Penetration of meropenem and vancomycin into the CSF is low while showing a high interindividual variability. Various patients in our study cohort were at risk for insufficient target attainment in CSF. Continuous administration of antibiotics under routine TDM appears to be a feasible and reasonable approach for optimization of intrathecal drug levels in patients suffering from ventriculitis. TDM might guide individual dosing adaptation and efforts to predict the CSF penetration of meropenem and vancomycin in cases of ventriculitis.


Similar content being viewed by others
Abbreviations
- ALAT:
-
Alanine aminotransferase
- ASAT:
-
Aspartate aminotransferase
- CRP:
-
C-reactive protein
- CSF:
-
Cerebrospinal fluid
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- EVD:
-
External ventricular drain
- GGT:
-
Gamma glutamyl transpeptidase
- GOS:
-
Glasgow Outcome Scale
- HPLC-UV:
-
High-performance liquid chromatography with ultra violet detection
- MIC:
-
Minimal inhibitory concentration
- SAPS II:
-
Simplified Acute Physiology Score II
- TDM:
-
Therapeutic drug monitoring
References
Albanese J, Leone M, Bruguerolle B, Ayem ML, Lacarelle B, Martin C (2000) Cerebrospinal fluid penetration and pharmacokinetics of vancomycin administered by continuous infusion to mechanically ventilated patients in an intensive care unit. Antimicrob Agents Chemother 44:1356–1358
Beach JE, Perrott J, Turgeon RD, Ensom MHH (2017) Penetration of vancomycin into the cerebrospinal fluid: a systematic review. Clin Pharmacokinet 56:1479–1490. https://doi.org/10.1007/s40262-017-0548-y
Blassmann U, Roehr AC, Frey OR, Vetter-Kerkhoff C, Thon N, Hope W, Briegel J, Huge V (2016) Cerebrospinal fluid penetration of meropenem in neurocritical care patients with proven or suspected ventriculitis: a prospective observational study. Crit Care 20:343. https://doi.org/10.1186/s13054-016-1523-y
Cataldo MA, Tacconelli E, Grilli E, Pea F, Petrosillo N (2012) Continuous versus intermittent infusion of vancomycin for the treatment of gram-positive infections: systematic review and meta-analysis. J Antimicrob Chemother 67:17–24. https://doi.org/10.1093/jac/dkr442
CDC/NHSN (2018) CDC/NHSN surveillance definitions for specific types of infections. https://www.cdc.gov/nhsn/PDFs/pscManual/17pscNosInfDef_current.pdf. Accessed August 3, 2018
Chen K, Wu Y, Wang Q, Wang J, Li X, Zhao Z, Zhou J (2015) The methodology and pharmacokinetics study of intraventricular administration of vancomycin in patients with intracranial infections after craniotomy. J Crit Care 30:218.e211–218.e215. https://doi.org/10.1016/j.jcrc.2014.09.020
Dulhunty JM, Roberts JA, Davis JS, Webb SA, Bellomo R, Gomersall C, Shirwadkar C, Eastwood GM, Myburgh J, Paterson DL, Starr T, Paul SK, Lipman J (2015) A multicenter randomized trial of continuous versus intermittent beta-lactam infusion in severe sepsis. Am J Respir Crit Care Med 192:1298–1305. https://doi.org/10.1164/rccm.201505-0857OC
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Ichie T, Urano K, Suzuki D, Okada T, Kobayashi N, Hayashi H, Sugiura Y, Yamamura K, Sugiyama T (2015) Influence of cerebral fluid drainage on the pharmacokinetics of vancomycin in neurosurgical patients. Pharmazie 70:404–409
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet 1:480–484
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Li C, Du X, Kuti JL, Nicolau DP (2007) Clinical pharmacodynamics of meropenem in patients with lower respiratory tract infections. Antimicrob Agents Chemother 51:1725–1730. https://doi.org/10.1128/aac.00294-06
Lin Wu FL, Liu SS, Yang TY, Win MF, Lin SW, Huang CF, Wang KC, Shen LJ (2015) A larger dose of vancomycin is required in adult neurosurgical intensive care unit patients due to augmented clearance. Ther Drug Monit 37:609–618. https://doi.org/10.1097/ftd.0000000000000187
Lonsdale DO, Udy AA, Roberts JA, Lipman J (2013) Antibacterial therapeutic drug monitoring in cerebrospinal fluid: difficulty in achieving adequate drug concentrations. J Neurosurg 118:297–301. https://doi.org/10.3171/2012.10.Jns12883
McKinnon PS, Paladino JA, Schentag JJ (2008) Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T>MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents 31:345–351. https://doi.org/10.1016/j.ijantimicag.2007.12.009
Mounier R, Lobo D, Hulin A, Nebbad B, Cook F, Dhonneur G (2017) Is first-line vancomycin still the best option to treat Staphylococcus health care-associated meningitis? World Neurosurg 99:812.e811–812.e815. https://doi.org/10.1016/j.wneu.2016.12.076
Nau R, Sorgel F, Eiffert H (2010) Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin Microbiol Rev 23:858–883. https://doi.org/10.1128/cmr.00007-10
No Authors (2000) The management of neurosurgical patients with postoperative bacterial or aseptic meningitis or external ventricular drain-associated ventriculitis. Infection in Neurosurgery Working Party of the British Society for Antimicrobial Chemotherapy. Br J Neurosurg 14:7–12
Pujal M, Soy D, Codina C, Ribas J (2006) Are higher vancomycin doses needed in ventricle-external shunted patients? Pharm World Sci 28:215–221. https://doi.org/10.1007/s11096-006-9037-3
Roberts JA, Lipman J (2009) Pharmacokinetic issues for antibiotics in the critically ill patient. Crit Care Med 37:840–851
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, Kaukonen KM, Koulenti D, Martin C, Montravers P, Rello J, Rhodes A, Starr T, Wallis SC, Lipman J (2014) DALI: defining antibiotic levels in intensive care unit patients: are current beta-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis 58:1072–1083. https://doi.org/10.1093/cid/ciu027
Roberts JA, Abdul-Aziz MH, Davis JS, Dulhunty JM, Cotta MO, Myburgh J, Bellomo R, Lipman J (2016) Continuous versus intermittent beta-lactam infusion in severe sepsis. A meta-analysis of individual patient data from randomized trials. Am J Respir Crit Care Med 194:681–691. https://doi.org/10.1164/rccm.201601-0024OC
Rybak M, Lomaestro B, Rotschafer JC, Moellering R Jr, Craig W, Billeter M, Dalovisio JR, Levine DP (2009) Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm 66:82–98. https://doi.org/10.2146/ajhp080434
Shah SS, Ohlsson A, Shah VS (2012) Intraventricular antibiotics for bacterial meningitis in neonates. Cochrane Database Syst Rev:Cd004496. https://doi.org/10.1002/14651858.CD004496.pub3
Smetana KS, Cook AM (2018) Cerebrospinal fluid vancomycin dosing and monitoring: the quandary posed by guideline recommendations. Clin Infect Dis. https://doi.org/10.1093/cid/ciy189
Sorgel F, Hohl R, Glaser R, Stelzer C, Munz M, Vormittag M, Kinzig M, Bulitta J, Landersdorfer C, Junger A, Christ M, Wilhelm M, Holzgrabe U (2017) Pharmacokinetics and pharmacodynamics of antibiotics in intensive care. Med Klin Intensivmed Notfmed 112:11–23. https://doi.org/10.1007/s00063-016-0185-5
Tangden T, Enblad P, Ullberg M, Sjolin J (2011) Neurosurgical gram-negative bacillary ventriculitis and meningitis: a retrospective study evaluating the efficacy of intraventricular gentamicin therapy in 31 consecutive cases. Clin Infect Dis 52:1310–1316. https://doi.org/10.1093/cid/cir197
Testing ECoAS (2018) Clinical breakpoints - bacteria (v8.1). http://www.eucast.org/clinical_breakpoints/. Accessed June 7, 2018
Tunkel AR, Hasbun R, Bhimraj A, Byers K, Kaplan SL, Michael Scheld W, van de Beek D, Bleck TP, Garton HJ, Zunt JR (2017) 2017 Infectious Diseases Society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis. https://doi.org/10.1093/cid/ciw861
van de Beek D, Drake JM, Tunkel AR (2010) Nosocomial bacterial meningitis. N Engl J Med 362:146–154. https://doi.org/10.1056/NEJMra0804573
Wang JH, Lin PC, Chou CH, Ho CM, Lin KH, Tsai CT, Wang JH, Chi CY, Ho MW (2014) Intraventricular antimicrobial therapy in postneurosurgical gram-negative bacillary meningitis or ventriculitis: a hospital-based retrospective study. J Microbiol Immunol Infect 47:204–210. https://doi.org/10.1016/j.jmii.2012.08.028
Wen DY, Bottini AG, Hall WA, Haines SJ (1992) Infections in neurologic surgery. The intraventricular use of antibiotics. Neurosurg Clin N Am 3:343–354
Wolff M, Regnier B, Garaud JJ, Faurisson F (1983) Intracisternal concentrations of vancomycin and amikacin after lumbar injections. Presse Med 12:2185
Author information
Authors and Affiliations
Contributions
MMM helped to design the study and to write the manuscript and acquired the data. PC helped to design the study and helped with the data acquisition. CK interpreted the data and helped to write the manuscript. VF helped to write the manuscript and to interpret the data. SK and MW helped with the interpretation and revised the manuscript. JG designed the study, wrote the manuscript, and helped to acquire the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Comments
Mader and colleagues provide a study about interesting aspects of a common and difficult problem in neurointensive care: intrathecal penetration of meropenem and vancomycin in ventriculitis, in this study administered by continuous infusion and controlled by therapeutic drug monitoring of CSF and serum. The limitations of the study—in my opinion especially the retrospective design of the study and possible differences in extend and stage of the infections—have adequately been discussed by the authors. As well as the authors conclude, this reviewer recommends performing a prospective study with a larger number of patients about this important topic in the future.
Marcus Reinges
Bremen, Germany
This article is part of the Topical Collection on Infection
Rights and permissions
About this article
Cite this article
Mader, M.MD., Czorlich, P., König, C. et al. Intrathecal penetration of meropenem and vancomycin administered by continuous infusion in patients suffering from ventriculitis—a retrospective analysis. Acta Neurochir 160, 2099–2105 (2018). https://doi.org/10.1007/s00701-018-3680-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3680-z