Abstract
Background
Post-traumatic hydrocephalus (PTH) is one of the main complications of decompressive craniectomy (DC) after traumatic brain injury (TBI). Then, the recognition of risk factors and subsequent prompt diagnosis and treatment of PTH can improve the outcome of these patients. The purpose of this study was to identify factors associated with the development of PTH requiring surgical treatment in patients undergoing DC for TBI.
Methods
In this study, we collected the data of 190 patients (149 males and 41 females), who underwent DC for TBI in our Center. Then we analyzed the type of surgical treatment for all patients affected by PTH and the risk factors associated with the development of PTH.
Results
Post-traumatic hydrocephalus (PTH) developed in 37 patients out of 130 alive 30 days after DC (28.4%). The development of PTH required ventriculoperitoneal shunt (VPS) in 34 patients out of 37 (91.9%), while, in the remaining 3 patients, cerebrospinal fluid hydrodynamic (CSF) disturbances resolved after urgent cranioplasty and temporary external lumbar drain. Multivariate analysis showed that the presence of interhemispheric hygroma (p < 0.001) and delayed cranioplasty (3 months after DC) (p < 0.001) was significantly associated with the need for a VPS or other surgical procedure for PTH. Finally, among the 130 patients alive after 30 days from DC, PTH was associated with unfavorable outcome as measured by the 6-month Glasgow Outcome Scale score (p < 0.0001).
Conclusions
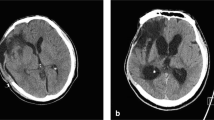
Our results showed that delayed cranial reconstruction was associated with an increasing rate of PTH after DC. The presence of an interhemispheric hygroma was an independent predictive radiological sign of PTH in decompressed patients for severe TBI.
Similar content being viewed by others
References
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ et al. (2017) Guidelines for the management of severe traumatic brain injury, Fourth Edition. Neurosurgery 80(1):6–15.
Cooper DJ, Rosenfeld JV, Murray L, Arabi YM, Davies AR, D’Urso P et al (2011) Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med 364(16):1493–1502
De Bonis P, Pompucci A, Mangiola A, Rigante L, Anile C (2010) Post-traumatic hydrocephalus after decompressive craniectomy: an underestimated risk factor. J Neurotrauma 27(11):1965–1970
De Bonis P, Sturiale CL, Anile C, Gaudino S, Mangiola A, Martucci M et al (2010) Decompressive craniectomy, interhemispheric hygroma and hydrocephalus: a timeline of events? Clin Neurol Neurosurg 115(8):1308–1312
Di Rienzo A, Iacoangeli M, Alvaro L, Colasanti R, Dobran M, Di Somma LG et al (2013) The sinking bone syndrome? Neurol Med Chir (Tokyo) 53(5):329–335
di Somma L, Iacoangeli M, Nasi D, Balercia P, Lupi E, Girotto R et al (2016) Combined supra-transorbital keyhole approach for treatment of delayed intraorbital encephalocele: a minimally invasive approach for an unusual complication of decompressive craniectomy. Surg Neurol Int 7(Suppl 1):S12–S16
Dobran M, Mancini F, Nasi D, Scerrati M (2017) A case of deep infection after instrumentation in dorsal spinal surgery: the management with antibiotics and negative wound pressure without removal of fixation. BMJ Case Rep 28:2017
Dobran M, Marini A, Gladi M, Nasi D, Colasanti R, Benigni R et al (2017) Deep spinal infection in instrumented spinal surgery: diagnostic factors and therapy. G Chir 38(3):124–129
Dobran M, Marini A, Nasi D, Gladi M, Liverotti V, Costanza MD et al (2017) Risk factors of surgical site infections in instrumented spine surgery. Surg Neurol Int 8:212
Dobran M, Nasi D, Esposito DP, Iacoangeli M (2016) Posterior fixation with C1 lateral mass screws and C2 pars screws for type ii odontoid fracture in the elderly: long-term follow-up. World Neurosurg 96:152–158
Honeybul S, Ho KM (2012) Incidence and risk factors for post-traumatic hydrocephalus following decompressive craniectomy for intractable intracranial hypertension and evacuation of mass lesions. J Neurotrauma 29(10):1872–1878
Huh PW, Yoo DS, Cho KS, Park CK, Kang SG, Park YS et al (2006) Diagnostic method for differentiating external hydrocephalus from simple subdural hygroma. J Neurosurg 105(1):65–70
Hutchinson PJ, Kolias AG, Timofeev IS, Corteen EA, Czosnyka M, Timothy J et al (2016) Trial of decompressive craniectomy for traumatic intracranial hypertension. N Engl J Med 375(12):1119–1130
Kaen A, Jimenez-Roldan L, Alday R, Gomez PA, Lagares A, Alén JF, Lobato RD (2010) Interhemispheric hygroma after decompressive craniectomy: does it predict posttraumatic hydrocephalus? J Neurosurg 113(6):1287–1293
Kurland DB, Khaladj-Ghom A, Stokum JA, Carusillo B, Karimy JK, Gerzanich V et al (2015) Complications associated with decompressive craniectomy: a systematic review. Neurocrit Care 23(2):292–304
Malcolm JG, Rindler RS, Chu JK, Choksh F, Grossberg JA, Pradilla G et al. (2017) Early cranioplasty is associated with greater neurological improvement: a systematic review and meta-analysis. Neurosurgery 82:278–288.
Nasi D, Dobran M, Iacoangeli M, Di Somma L, Gladi M, Scerrati M (2016) Paradoxical brain herniation after decompressive craniectomy provoked by drainage of subdural hygroma. World Neurosurg 91:673.e1–4
Nasi D, Dobran M, Di Rienzo A, di Somma L, Gladi M, Moriconi E et al (2018) Decompressive craniectomy for traumatic brain injury: the role of cranioplasty and hydrocephalus on outcome. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.05.028
Stiver SI (2009) Complications of decompressive craniectomy for traumatic brain injury. Neurosurg Focus 26(6):E7
Vedantam A, Yamal JM, Hwang H, Robertson CS, Gopinath SP (2018) Factors associated with shunt-dependent hydrocephalus after decompressive craniectomy for traumatic brain injury. J Neurosurg 128(5):1547–1552
Waziri A, Fusco D, Mayer SA, McKhann GM 2nd, Connolly ES Jr (2007) Postoperative hydrocephalus in patients undergoing decompressive hemicraniectomy for ischemic or hemorrhagic stroke. Neurosurgery 61:489–493
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comments
In this retrospective observational study, Dr. Nasi et al. investigate the incidence rate of hydrocephalus following decompressive craniectomy (DC) for traumatic brain injury (TBI). In their patient cohort of 130 patients surviving the first month after DC, 37 patients (28%) were diagnosed with hydrocephalus defined by both progressive ventricular enlargement and clinical deterioration. The presence of an interhemispheric hygroma during the early phase after DC and cranioplasty later than 3 months after DC was independent risk factors for the development of symptomatic hydrocephalus requiring treatment. Interhemispheric hygroma may indeed be an indicator of disturbed cerebrospinal fluid circulation (caused by the trauma or the large skull defect resulting from the DC) and this radiological finding should be taken into account in evaluation of patients with clinical deterioration following DC, when hydrocephalus is suspected. The effect of cranioplasty timing is still debated and controversial. A recent (and larger) observational study by Morton et al. came to the opposite conclusion that cranioplasty later that 90 days after DC was associated with a lower risk of hydrocephalus. [1] This issue needs further exploration in future prospective (randomized?) studies.
Alexander Lilja-Cyron
Copenhagen, Denmark
1. Morton RP, Abecassis IJ, Hanson JF, et al (2017) Timing of cranioplasty: a 10.75-year single-center analysis of 754 patients. J Neurosurg 128(128):1-5
This article is part of the Topical Collection on Brain trauma
Rights and permissions
About this article
Cite this article
Nasi, D., Gladi, M., Di Rienzo, A. et al. Risk factors for post-traumatic hydrocephalus following decompressive craniectomy. Acta Neurochir 160, 1691–1698 (2018). https://doi.org/10.1007/s00701-018-3639-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3639-0