Abstract
Background
Distress impacts the daily life of glioma patients. This study explored its course over time and the usage of psychosocial care.
Methods
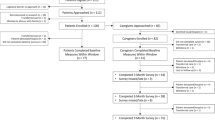
A consecutive sample of glioma patients completed the Hospital Anxiety and Depression Scale to assess distress levels at admission to the hospital (t1), before discharge (t2), after 3 months (t3), and after 6 months (t4). They were interviewed with the Structured Clinical Interview for DSM-IV to ascertain psychiatric disorders at t2. Psycho-oncological care in the hospital was determined with the Hospital Information System, and the use of outpatient treatment was evaluated with the Health Care Usage Questionnaire at t4. We compared the percentages of elevated distress, psychiatric co-morbidity, and care usage between men and women.
Results
During the study period, 37 patients were enrolled. Nineteen percent of the patients were diagnosed with a psychiatric disorder. The percentages of patients with elevated distress were 56, 59, 39, and 40% at t1, t2, t3, and t4, respectively. Participants who did not survive the 6 months presented with higher levels of distress. In the hospital, 14% of those with elevated distress were visited by a psycho-oncologist. In the outpatient setting, 43% of those with elevated distress visited a neuro-psychiatrist, and 14% went to a psychotherapist. There was no evidence for an effect of gender on psychiatric co-morbidity, distress, or care use.
Conclusions
A significant proportion of glioma patients report elevated distress during the hospital stay and thereafter. Only a fraction of them receive mental health care.


Similar content being viewed by others
References
Aaronson N, Ahmedzai S, Bergmann B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, de Haes JCJM, Kaasa S, Klee M, Osoba D, Razavi D, Rofe PB, Schraub S, Sneeuw K, Sullivan M, Takeda F, for the EORTC Study Group on Quality of Life (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Aaronson NK, Taphoorn MJB, Heimans JJ, Postma TJ, Gundy CM, Beute GN, Slotman BJ, Klein M (2011) Compromised health-related quality of life in patients with low-grade Glioma. J Clin Oncol 29:4430–4435
Boele FW, van Uden-Kraan CF, Hilverda K, Reijneveld JC, Cleijne W, Klein M, Verdonck-de Leeuw IM (2016) Attitudes and preferences toward monitoring symptoms, distress, and quality of life in glioma patients and their informal caregivers. Support Care Cancer 24:3011–3022
Borooah VK (2010) Gender differences in the incidence of depression and anxiety: econometric evidence from the USA. J Happiness Stud 11:663–682
Brebach R, Sharpe L, Costa DSJ, Rhodes P, Butow P (2016) Psychological intervention targeting distress for cancer patients: a meta-analytic study investigating uptake and adherence. Psychooncology 25:882–890
Briest S, Papsdorf K, Köhler U, Krauß O, Singer S (2015) Sind Brustkrebspatientinnen mit frühen Stadien weniger psychisch belastet als jene mit fortgeschrittenen Stadien? Onkologe 21:245–249
DAngelo C, Mirijello A, Leggio L, Ferrulli A, Carotenuto V, Icolaro N, Miceli A, D'Angelo V, Gasbarrini G, Addolorato G (2008) State and trait anxiety and depression in patients with primary brain tumors before and after surgery: 1-year longitudinal study. J Neurosurg 108:281–286
Dirven L, Reijneveld JC, Taphoorn MJB (2014) Health-related quality of life or quantity of life: a difficult trade-off in primary brain tumors? Semin Oncol 41:541–552
Efficace F, Taphoorn M (2012) Methodological issues in designing and reporting health-related quality of life in cancer clinical trials: the challenge of brain cancer studies. J Neuro-Oncol 108:221–226
Erharter A, Giesinger J, Kemmler G, Schauer-Maurer G, Stockhammer G, Muigg A, Hutterer M, Rumpold G, Sperner-Unterweger B, Holzner B (2010) Implementation of computer-based quality-of-life monitoring in brain tumor outpatients in routine clinical practice. J Pain Symptom Manag 39:219–229
First M, Spitzer R, Gibbon M, Williams J (1997) Structured clinical interview for DSM-IV Axis I disorders (SCID-I), clinician version. American Psychiatric Press, Washington, DC
Ford E, Catt S, Chalmers A, Fallowfield L (2012) Systematic review of supportive care needs in patients with primary malignant brain tumors. Neuro-Oncology 14:392–404
Geue K, Richter R, Buttstädt M, Brähler E, Böhler U, Singer S (2012) Art therapy in psycho-oncology - recruitment of participants and gender differences in usage. Support Care Cancer 20:679–686
Glaesmer H, Brahler E, Martin A, Mewes R, Rief W (2008) Gender differences in subjective help seeking threshold and health care utilization: is there an interrelation between both features? Int J Psychol 43:438
Goebel S, Strenge H, Mehdorn HM (2012) Acute stress in patients with brain cancer during primary care. Support Care Cancer 20:1425–1434
Goebel S, von Harscher M, Mehdorn HM (2011) Comorbid mental disorders and psychosocial distress in patients with brain tumours and their spouses in the early treatment phase. Support Care Cancer 19:1797–1805
Grassi L, Watson M, on behalf of the IPOS Federation of Psycho-Oncology Societies' co-authors (2012) Psychosocial care in cancer: an overview of psychosocial programmes and national cancer plans of countries within the International Federation of Psycho-Oncology Societies. Psycho-Oncology 21:1027–1033
Hickmann AK, Nadji-Ohl M, Haug M, Hopf N, Ganslandt O, Giese A, Renovanz M (2016) Suicidal ideation, depression, and health-related quality of life in patients with benign and malignant brain tumors: a prospective observational study in 83 patients. Acta Neurochir 158:1669–1682
Johnson M, Stone GL (1989) Logic and nurture - gender differences in thinking about psychotherapy. Prof Psychol Res Pract 20:123–127
Khan F, Amatya B (2013) Factors associated with long-term functional outcomes, psychological sequelae and quality of life in persons after primary brain tumour. J Neuro-Oncol 111:355–366
Kvale EA, Murthy R, Taylor R, Lee JY, Nabors LB (2009) Distress and quality of life in primary high-grade brain tumor patients. Support Care Cancer 17:793–799
Lin L, Chiang HH, Acquaye AA, Vera-Bolanos E, Gilbert MR, Armstrong TS (2013) Uncertainty, mood states, and symptom distress in patients with primary brain tumors: analysis of a conceptual model using structural equation modeling. Cancer 119:2796–2806
Litofsky NS, Farace E, Anderson F, Meyers CA, Huang W, Laws ER (2004) Depression in patients with high-grade glioma: results of the glioma outcomes project. Neurosurgery 54:358–366
Lyons Z, Janca A (2009) Diagnosis of male depression does general practitioner gender play a part? Aust Fam Physician 38:743–746
Mainio A, Hakko H, Niemela A, Koivukangas J, Rasanen P (2006) Gender difference in relation to depression and quality of life among patients with a primary brain tumor. Eur Psychiatry 21:194–199
Mehnert A, Brähler E, Faller H, Härter M, Keller M, Schulz H, Wegscheider K, Weis J, Boehncke A, Hund B, Reuter K, Richard M, Sehner S, Sommerfeldt S, Szalai C, Wittchen HU, Koch U (2014) Four-week prevalence of mental disorders in cancer patients across major tumor entitites. J Clin Oncol 32:3540–3546
Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N (2011) Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 12:160–174
Mitchell AJ, Symonds P (2013) Implementation of distress screening by Cancer clinicians during routine clinical care. Part I. Focus on efficiency and acceptability of frontline screening. Psychooncology 22:91
Pelletier G, Verhoef MJ, Khatri N, Hagen N (2002) Quality of life in brain tumor patients: the relative contributions of depression, fatigue, emotional distress, and existential issues. J Neuro-Oncol 57:41–49
Piil K, Jakobsen J, Christensen KB, Juhler M, Jarden M (2015) Health-related quality of life in patients with high-grade gliomas: a quantitative longitudinal study. J Neuro-Oncol 124:185–195
Renovanz M, Hickmann A-K, Coburger J, Kohlmann K, Janko M, Reuter AK, Keric N, Gutenberg A, Nadji-Ohl M, König J, Singer S, Giese A, Hechtner M (2017) Assessing psychological and supportive care needs in Glioma patients – feasibility study on the use of the supportive care needs survey short form (SCNS-SF34-G) and the supportive care needs survey screening tool (SCNS-ST9) in clinical practice. Eur J Cancer Care. https://doi.org/10.1111/ecc.12598
Robin AM, Walbert T, Mikkelsen T, Kalkanis SN, Rock J, Lee I, Rosenblum ML (2014) Through the patient's eyes: the value of a comprehensive brain tumor center. J Neuro-Oncol 119:465–472
Rooney AG, Carson A, Grant R (2011) Depression in cerebral Glioma patients: a systematic review of observational studies. J Natl Cancer Inst 103:61–76
Rooney AG, McNamara S, Mackinnon M, Fraser M, Rampling R, Carson A, Grant R (2011) Frequency, clinical associations, and longitudinal course of major depressive disorder in adults with cerebral Glioma. J Clin Oncol 29:4307–4312
Rooney AG, McNamara S, MacKinnon M, Fraser M, Rampling R, Carson A, Grant R (2013) The frequency, longitudinal course, clinical associations, and causes of emotional distress during primary treatment of cerebral glioma. Neuro-Oncology 15:635–643
Rooney AG, van Nieuwenhuizen D, Reijneveld JC, Grant R (2009) Female gender is not a proven risk factor for depression in glioma. J Neuro-Oncol 95:449
Rosenblum ML, Kalkanis S, Goldberg W, Rock J, Mikkelsen T, Remer S, Whitehouse S, Nerenz D (2009) Odyssey of hope: a physician's guide to communicating with brain tumor patients across the continuum of care. J Neuro-Oncol 92:241–251
Scaratti C, Leonardi M, Saladino A, Anghileri E, Broggi M, Lamperti E, Fariselli L, Ayadi R, Tringali G, Schiavolin S (2017) Needs of neuro-oncological patients and their caregivers during the hospitalization and after discharge: results from a longitudinal study. Support Care Cancer 25:2137–2145
Singer S, Bringmann H, Hauss J, Kortmann R-D, Köhler U, Krauß O, Schwarz R (2007) Häufigkeit psychischer Begleiterkrankungen und der Wunsch nach psychosozialer Unterstützung bei Tumorpatienten im Akutkrankenhaus. Dtsch Med Wochenschr 132:2071–2076
Singer S, Das-Munshi J, Brähler E (2010) Prevalence of mental health conditions in cancer patients in acute care – a meta-analysis. Ann Oncol 21:925–930
Singer S, Hohlfeld S, Müller-Briel D, Dietz A, Brähler E, Schröter K, Lehmann-Laue A (2011) Psychosoziale Versorgung von Krebspatienten - Versorgungsdichte und -bedarf. Psychotherapeut 56:386–393
Singer S, Kuhnt S, Götze H, Hauss J, Hinz A, Liebmann A, Krauß O, Lehmann A, Schwarz R (2009) Hospital anxiety and depression scale cut-off scores for Cancer patients in acute care. Br J Cancer 100:908–912
Tang PL, Wang HH, Chou FH (2015) A systematic review and meta-analysis of demoralization and depression in patients with Cancer. Psychosomatics 56:634–643
Taphoorn MJB, Sizoo EM, Bottomley A (2010) Review on quality of life issues in patients with primary brain tumors. Oncologist 15:618–626
Thode N, Bergmann E, Kamtsiuris P, Kurth M (2005) Einflussfaktoren auf die ambulante Inanspruchnahme in Deutschland. Bundesgesundheitsblatt 48:296–306
Velikova G, Coens C, Efficace F, Greimel E, Groenvold M, Johnson C, Singer S, van de Poll-Franse L, Young T, Bottomley A, on behalf of the EORTC Quality of Life Group (2012) Health-related quality of life in EORTC clinical trials - 30 years of progress from methodological developments to making a real impact on oncology practice. Eur J Cancer Suppl 10:141–149
Warrington TP, Bostwick JM (2006) Psychiatric adverse effects of corticosteroids. Mayo Clin Proc 81:1361–1367
Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jonsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, Fratiglioni L, Jennum P, Lieb R, Maercker A, van Os J, Preisig M, Salvador-Carulla L, Simon R, Steinhausen HC (2011) The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 21:655–679
Zeissig SR, Singer S, Koch L, Zeeb H, Merbach M, Bertram H, Eberle A, Schmid-Höpfner S, Holleczek B, Waldmann A, Arndt V (2015) Utilisation of psychosocial and informational services in immigrant and non-immigrant German cancer survivors. Psycho-Oncology 24:919–925
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Funding
This study was funded by the German Federal Ministry of Health (#NKP-332-026).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SS received a grant from Pfizer, the quality of life prize from Lilly, and lecture fees from Pfizer, Bristol-Myers Squibb, and Boehringer Ingelheim. These were unrelated to the study presented here. The other authors declare that they have no conflict of interest.
Ethics
All procedures performed were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments. The study protocol was approved by the local ethics committee. All participants provided written informed consent.
Rights and permissions
About this article
Cite this article
Singer, S., Roick, J., Danker, H. et al. Psychiatric co-morbidity, distress, and use of psycho-social services in adult glioma patients—a prospective study. Acta Neurochir 160, 1187–1194 (2018). https://doi.org/10.1007/s00701-018-3527-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3527-7