Abstract
Background
There is a paucity of data concerning the safety and efficacy of surgical education for neurosurgical residents in the evacuation of chronic subdural hematomas (cSDH) by burr hole trepanation.
Methods
This is a retrospective analysis of prospectively collected data on consecutive patients receiving burr hole trepanation for uni- or bilateral cSDH. Patients operated by a supervised neurosurgery resident (teaching cases) were compared to patients operated by a board-certified faculty neurosurgeon (BCFN; non-teaching cases). The primary endpoint was surgical revision for any reason until the last follow-up. The secondary endpoint was occurrence of any complication until the last follow-up. Clinical status, type of complications, mortality, length of surgery (LOS), and hospitalization (LOH) were tertiary endpoints.
Results
A total of n = 253 cases were analyzed, of which n = 217 (85.8%) were teaching and n = 36 (14.2%) non-teaching cases. The study groups were balanced in terms of age, sex, surgical risk (ASA score), and preoperative status (Karnofsky Performance Scale (KPS), modified Rankin Scale (mRS), National Institute of Health Stroke Scale (NIHSS)). The cohort was followed for a mean of 242 days (standard deviation 302). In multivariate analysis, teaching cases were as likely as non-teaching cases to require revision surgery (OR 0.65, 95% CI 0.27–1.59; p = 0.348) as well as to experience any complication until the last follow-up (OR 0.79, 95% CI 0.37–1.67; p = 0.532). Mean LOS was about 10 min longer in teaching cases (53.0 ± 26.1 min vs. 43.5 ± 17.8 min; p = 0.036), but LOH was similar. There were no group differences in clinical status, mortality and type of complication at discharge, and the last follow-up.
Conclusions
Burr hole trepanation for cSDH can be safely performed by supervised neurosurgical residents enrolled in a structured training program, without increasing the risk for revision surgery, perioperative complications, or worse outcome.


Similar content being viewed by others
Abbreviations
- ASA:
-
American Society of Anesthesiology grading scale
- BCFN:
-
Board-certified faculty neurosurgeon
- CDG:
-
Clavien-Dindo grade
- cSDH:
-
Chronic subdural hematoma
- CT:
-
Computed tomography
- IQR:
-
Interquartile range
- LOH:
-
Length of hospitalization
- LOS:
-
Length of surgery
- KPS:
-
Karnofsky Performance Scale
- mRS:
-
Modified Rankin scale
- NIHSS:
-
National Institute of Health Stroke Scale
- MLS:
-
Midline shift
- PGY:
-
Postgraduate year
- SD:
-
Standard deviation
References
Babu R, Thomas S, Hazzard MA et al (2014) Worse outcomes for patients undergoing brain tumor and cerebrovascular procedures following the ACGME resident duty-hour restrictions. J Neurosurg 121(2):262–276
Babu R, Thomas S, Hazzard MA et al (2014) Morbidity, mortality, and health care costs for patients undergoing spine surgery following the ACGME resident duty-hour reform: clinical article. J Neurosurg Spine 21(4):502–515
Bartek J, Sjåvik K, Kristiansson H, Ståhl F, Fornebo I, Förander P, Jakola AS (2017) Predictors of recurrence and complications after chronic subdural hematoma surgery: a population-based study. World Neurosurg 106:609–614
Bellut D, Woernle CM, Burkhardt J-K, Kockro RA, Bertalanffy H, Krayenbühl N (2012) Subdural drainage versus subperiosteal drainage in burr-hole trepanation for symptomatic chronic subdural hematomas. World Neurosurg 77(1):111–118
Bina RW, Lemole GM, Dumont TM (2016) On resident duty hour restrictions and neurosurgical training: review of the literature. J Neurosurg 124(3):842–848
Borger V, Vatter H, Oszvald Á, Marquardt G, Seifert V, Güresir E (2012) Chronic subdural haematoma in elderly patients: a retrospective analysis of 322 patients between the ages of 65-94 years. Acta Neurochir 154(9):1549–1554
Brennan PM, Kolias AG, Joannides AJ et al (2016) The management and outcome for patients with chronic subdural hematoma: a prospective, multicenter, observational cohort study in the United Kingdom. J Neurosurg:1–8
Coulter IC, Kolias AG, Marcus HJ et al (2014) Proposal for a prospective multi-centre audit of chronic subdural haematoma management in the United Kingdom and Ireland. Br J Neurosurg 28(2):199–203
Gastone P, Fabrizia C, Homere M, Cacciola F, Francesco C, Alberto M, Nicola DL (2004) Chronic subdural hematoma: results of a homogeneous series of 159 patients operated on by residents. Neurol India 52(4):475–477
Han M-H, Ryu, JIL, Kim CH, Kim JM, Cheong JH, Yi H-J (2016) Predictive factors for recurrence and clinical outcomes in patients with chronic subdural hematoma. J Neurosurg 1–9
Ivamoto HS, Lemos HP, Atallah AN (2016) Surgical treatments for chronic subdural hematomas: a comprehensive systematic review. World Neurosurg 86:399–418
Joswig H, Gautschi OP, El Rahal A, Sveikata L, Bartoli A, Hildebrandt G, Schaller K, Stienen MN (2016) Cranioplasty: is surgical education safe? World Neurosurg 91:81–88
Joswig H, Haile SR, Hildebrandt G, Stienen MN (2017) Residents’ learning curve of lumbar transforaminal epidural steroid injections. J Neurol Surg A Cent Eur Neurosurg 78(5):460–466
Joswig H, Hock C, Hildebrandt G, Schaller K, Stienen MN (2016) Microscopic lumbar spinal stenosis decompression: is surgical education safe? Acta Neurochir 158(2):357–366
Joswig H, Jucker D, Lavalley A, Sprenger L, Gautschi OP, Hildebrandt G, Schaller K, Stienen MN (2017) Shunts: is surgical education safe? World Neurosurg 102:117–122
Kaliaperumal C, Khalil A, Fenton E, Okafo U, Kaar G, O’Sullivan M, Marks C (2012) A prospective randomised study to compare the utility and outcomes of subdural and subperiosteal drains for the treatment of chronic subdural haematoma. Acta Neurochir (Wien) 154(11):2083-8-9
Leroy H-A, Aboukaïs R, Reyns N, Bourgeois P, Labreuche J, Duhamel A, Lejeune J-P (2015) Predictors of functional outcomes and recurrence of chronic subdural hematomas. J Clin Neurosci 22(12):1895–1900
Liu W, Bakker NA, Groen RJM (2014) Chronic subdural hematoma: a systematic review and meta-analysis of surgical procedures. J Neurosurg 121(3):665–673
Mellergård P, Wisten O (1996) Operations and re-operations for chronic subdural haematomas during a 25-year period in a well defined population. Acta Neurochir 138(6):708–713
Nathan S, Goodarzi Z, Jette N, Gallagher C, Holroyd-Leduc J (2017) Anticoagulant and antiplatelet use in seniors with chronic subdural hematoma: systematic review. Neurology 88(20):1889–1893
Neidert MC, Schmidt T, Mitova T, Fierstra J, Bellut D, Regli L, Burkhardt J-K, Bozinov O (2016) Preoperative angiotensin converting enzyme inhibitor usage in patients with chronic subdural hematoma: associations with initial presentation and clinical outcome. J Clin Neurosci 28:82–86
Phang I, Sivakumaran R, Papadopoulos MC (2015) No association between seniority of surgeon and postoperative recurrence of chronic subdural haematoma. Ann R Coll Surg Engl 97(8):584–588
Santarius T, Kirkpatrick PJ, Ganesan D et al (2009) Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet (London, England) 374(9695):1067–1073
Sarnthein J, Stieglitz L, Clavien P-A, Regli L (2016) A patient registry to improve patient safety: recording general neurosurgery complications. PLoS One 11(9):e0163154
Schaller K (2013) Neurosurgical training under European law. Acta Neurochir 155(3):547
Schwarz F, Loos F, Dünisch P, Sakr Y, Safatli DAL, Kalff R, Ewald C (2015) Risk factors for reoperation after initial burr hole trephination in chronic subdural hematomas. Clin Neurol Neurosurg 138:66–71
Soleman J, Lutz K, Schaedelin S, Mariani L, Fandino J (2016) Use of subperiosteal drain versus subdural drain in chronic subdural hematomas treated with burr-hole trepanation: study protocol for a randomized controlled trial. JMIR Res Protoc 5(2):e38
Stienen MN, Joswig H, Jucker D, Hildebrandt G, Schaller K, Gautschi OP (2015) Anterior cervical discectomy and fusion: is surgical education safe? Acta Neurochir 157(8):1395–1404
Stienen MN, Netuka D, Demetriades AK, Ringel F, Gautschi OP, Gempt J, Kuhlen D, Schaller K (2016) Working time of neurosurgical residents in Europe—results of a multinational survey. Acta Neurochir 158(1):17–25
Stienen MN, Netuka D, Demetriades AK, Ringel F, Gautschi OP, Gempt J, Kuhlen D, Schaller K (2016) Neurosurgical resident education in Europe—results of a multinational survey. Acta Neurochir 158(1):3–15
Stienen MN, Netuka D, Demetriades AK, Ringel F, Gautschi OP, Gempt J, Kuhlen D, Schaller K (2016) Residency program trainee-satisfaction correlate with results of the European board examination in neurosurgery. Acta Neurochir 158(10):1823–1830
Stienen MN, Smoll NR, Hildebrandt G, Schaller K, Gautschi OP (2014) Early surgical education of residents is safe for microscopic lumbar disc surgery. Acta Neurochir 156(6):1205–1214
Stienen MN, Smoll NR, Tessitore E, Schaller K, Hildebrandt G, Gautschi OP (2015) Surgical resident education in noninstrumented lumbar spine surgery: a prospective observational study with a 4.5-year follow-up. World Neurosurg 84(6):1589–1597
Stovell MG, Jenkinson MD (2014) Neurosurgery in octogenarians. Br J Neurosurg 28(5):611–615
Wada M, Yamakami I, Higuchi Y, Tanaka M, Suda S, Ono J, Saeki N (2014) Influence of antiplatelet therapy on postoperative recurrence of chronic subdural hematoma: a multicenter retrospective study in 719 patients. Clin Neurol Neurosurg 120:49–54
Wakai S, Hashimoto K, Watanabe N, Inoh S, Ochiai C, Nagai M (1990) Efficacy of closed-system drainage in treating chronic subdural hematoma: a prospective comparative study. Neurosurgery 26(5):771–773
Zumofen D, Regli L, Levivier M, Krayenbühl N (2009) Chronic subdural hematomas treated by burr hole trepanation and a subperiostal drainage system. Neurosurgery 64(6):1116-21–1116-22
Acknowledgements
The authors thank all resident and staff physicians of the department, who prospectively collected and verified the data that is the basis of the current analysis.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The local ethics committee (Kantonale Ethikkommission KEK-ZH 2012–0244) approved the prospective data collection in the patient registry. The study was registered at clinicaltrials.gov (NCT01628406) and follows the STROBE recommendation for observational studies.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
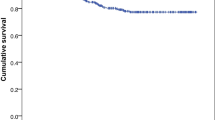
Supplementary Figure 1
Kaplan-Meier time-to-event estimates with time censored at 365 days postoperative. The endpoint is death in patients operated on by supervised neurosurgery residents (Teaching procedure) or experienced board-certified faculty neurosurgeons (No teaching procedure). There was no significant difference in the endpoint (Log-rank test: p = 0.322). (GIF 28 kb)
Rights and permissions
About this article
Cite this article
Maldaner, N., Sosnova, M., Sarnthein, J. et al. Burr hole trepanation for chronic subdural hematomas: is surgical education safe?. Acta Neurochir 160, 901–911 (2018). https://doi.org/10.1007/s00701-017-3458-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3458-8