Abstract
Background
Close relatives (CR) of patients with severe traumatic brain injury (TBI) and high-grade subarachnoid hemorrhage (SAH) suffer extraordinary distress during the treatment: Distress may lead to persisting mental illness symptoms within the spectrum of post-traumatic stress disorder (PTSD), anxiety disorders, and depression. The primary goal of this study was to determine the prevalence and severity of these symptoms in CR. The secondary goal was identification of associated factors.
Method
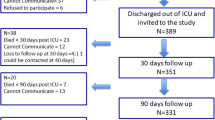
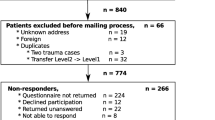
Standardized interviews were conducted with 53 CR (mean age of 57.7 ± 11.4 years) of patients with TBI °III (n = 27) and high-grade SAH H&H °III–V (n = 26) between 5 and 15 months after the event. The interviews contained a battery of surveys to quantify symptoms of PTSD, anxiety disorders, and depression, i.e., Impact of Event Scale (IES-R), 36-item Short-Form General Health Survey (SF-36), and Hospital Anxiety and Depression Scale (HADS). Fixed and modifiable possibly influencing factors were correlated.
Results
Twenty-eight CR (53 %) showed IES-R scores indicating a probable diagnosis of PTSD. Twenty-five CR (47 %) showed an increased anxiety score and 18 (34 %) an increased depression score using HADS. Mean physical component summary of SF-36 was not abnormal (49.1 ± 9.1), whereas mean mental component summary was under average (41.0 ± 13.2), indicating a decreased quality of life caused by mental effects. Perception of the interaction quality with the medical staff and involvement into medical decisions correlated negatively with severity of mental illness symptoms. Evasive coping strategies were highly significantly associated with symptoms.
Conclusions
This study quantifies an extraordinarily high prevalence of mental illness symptoms in CR of patients with critical acquired brain injury due to SAH and TBI. Modifiable factors were associated with severity of mental illness symptoms. Prospective studies testing efficiency of early psychotherapeutic interventions are needed.

Similar content being viewed by others
References
Azoulay E, Pochard F, Chevret S, Adrie C, Annane D, Bleichner G, Bornstain C, Bouffard Y, Cohen Y, Feissel M, Goldgran-Toledano D, Guitton C, Hayon J, Iglesias E, Joly LM, Jourdain M, Laplace C, Lebert C, Pingat J, Poisson C, Renault A, Sanchez O, Selcer D, Timsit JF, Le Gall JR, Schlemmer B (2004) Half the family members of intensive care unit patients do not want to share in the decision-making process: a study in 78 French intensive care units. Crit Care Med 32:1832–1838
Azoulay E, Pochard F, Chevret S, Arich C, Brivet F, Brun F, Charles PE, Desmettre T, Dubois D, Galliot R, Garrouste-Orgeas M, Goldgran-Toledano D, Herbecq P, Joly LM, Jourdain M, Kaidomar M, Lepape A, Letellier N, Marie O, Page B, Parrot A, Rodie-Talbere PA, Sermet A, Tenaillon A, Thuong M, Tulasne P, Le Gall JR, Schlemmer B (2003) Family participation in care to the critically ill: opinions of families and staff. Intensive Care Med 29:1498–1504
Azoulay E, Pochard F, Chevret S, Lemaire F, Mokhtari M, Le Gall JR, Dhainaut JF, Schlemmer B (2001) Meeting the needs of intensive care unit patient families: a multicenter study. Am J Respir Crit Care Med 163:135–139
Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, Fassier T, Galliot R, Garrouste-Orgeas M, Goulenok C, Goldgran-Toledano D, Hayon J, Jourdain M, Kaidomar M, Laplace C, Larche J, Liotier J, Papazian L, Poisson C, Reignier J, Saidi F, Schlemmer B (2005) Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 171:987–994
Beck JG, Grant DM, Read JP, Clapp JD, Coffey SF, Miller LM, Palyo SA (2008) The impact of event scale-revised: psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord 22:187–198
Bieber C, Nicolai J, Hartmann M, Blumenstiel K, Ringel N, Schneider A, Harter M, Eich W, Loh A (2009) Training physicians in shared decision-making-who can be reached and what is achieved? Patient Educ Couns 77:48–54
Bjelland I, Dahl AA, Haug TT, Neckelmann D (2002) The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 52:69–77
Boerboom W, Jacobs EA, Khajeh L, van Kooten F, Ribbers GM, Heijenbrok-Kal MH (2014) The relationship of coping style with depression, burden, and life dissatisfaction in caregivers of patients with subarachnoid haemorrhage. J Rehabil Med 46:321–326
Brugha TS, Cragg D (1990) The List of Threatening Experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr Scand 82:77–81
Buchanan KM, Elias LJ, Goplen GB (2000) Differing perspectives on outcome after subarachnoid hemorrhage: the patient, the relative, the neurosurgeon. Neurosurgery 46:831–838, discussion 838–840
Carver CS (1997) You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med 4:92–100
Covey J, Noble AJ, Schenk T (2013) Family and friends’ fears of recurrence: impact on the patient’s recovery after subarachnoid hemorrhage. J Neurosurg 119:948–954
Curtis JR, Patrick DL, Shannon SE, Treece PD, Engelberg RA, Rubenfeld GD (2001) The family conference as a focus to improve communication about end-of-life care in the intensive care unit: opportunities for improvement. Crit Care Med 29:N26–N33
Davis LC, Sander AM, Struchen MA, Sherer M, Nakase-Richardson R, Malec JF (2009) Medical and psychosocial predictors of caregiver distress and perceived burden following traumatic brain injury. J Head Trauma Rehabil 24:145–154
Dennis M, O’Rourke S, Lewis S, Sharpe M, Warlow C (1998) A quantitative study of the emotional outcome of people caring for stroke survivors. Stroke 29:1867–1872
Gjerris A, Bech P, Bojholm S, Bolwig TG, Kramp P, Clemmesen L, Andersen J, Jensen E, Rafaelsen OJ (1983) The Hamilton Anxiety Scale. Evaluation of homogeneity and inter-observer reliability in patients with depressive disorders. J Affect Disord 5:163–170
Gries CJ, Engelberg RA, Kross EK, Zatzick D, Nielsen EL, Downey L, Curtis JR (2010) Predictors of symptoms of posttraumatic stress and depression in family members after patient death in the ICU. Chest 137:280–287
Hanks RA, Rapport LJ, Vangel S (2007) Caregiving appraisal after traumatic brain injury: the effects of functional status, coping style, social support and family functioning. NeuroRehabilitation 22:43–52
Harris IA, Young JM, Rae H, Jalaludin BB, Solomon MJ (2008) Predictors of post-traumatic stress disorder following major trauma. ANZ J Surg 78:583–587
Hinz A, Schwarz R (2001) Anxiety and depression in the general population: normal values in the Hospital Anxiety and Depression Scale. Psychother Psychosom Med Psychol 51:193–200
Hop JW, Rinkel GJ, Algra A, van Gijn J (1998) Quality of life in patients and partners after aneurysmal subarachnoid hemorrhage. Stroke 29:798–804
Hop JW, Rinkel GJ, Algra A, van Gijn J (2001) Changes in functional outcome and quality of life in patients and caregivers after aneurysmal subarachnoid hemorrhage. J Neurosurg 95:957–963
Horowitz M, Wilner N, Alvarez W (1979) Impact of Event Scale: a measure of subjective stress. Psychosom Med 41:209–218
Kentish-Barnes N, Lemiale V, Chaize M, Pochard F, Azoulay E (2009) Assessing burden in families of critical care patients. Crit Care Med 37:S448–S456
Noble AJ, Schenk T (2008) Posttraumatic stress disorder in the family and friends of patients who have suffered spontaneous subarachnoid hemorrhage. J Neurosurg 109:1027–1033
Paparrigopoulos T, Melissaki A, Tzavellas E, Karaiskos D, Ilias I, Kokras N (2014) Increased co-morbidity of depression and post-traumatic stress disorder symptoms and common risk factors in intensive care unit survivors: a two-year follow-up study. Int J Psychiatry Clin Pract 18:25–31
Pryzby BJ (2005) Effects of nurse caring behaviours on family stress responses in critical care. Intensiv Crit Care Nurs 21:16–23
Rothen HU, Stricker KH, Heyland DK (2010) Family satisfaction with critical care: measurements and messages. Curr Opin Crit Care 16:623–631
Smith LN, Norrie J, Kerr SM, Lawrence IM, Langhorne P, Lees KR (2004) Impact and influences on caregiver outcomes at one year post-stroke. Cerebrovasc Dis 18:145–153
Sundin EC, Horowitz MJ (2002) Impact of Event Scale: psychometric properties. Br J Psychiatry 180:205–209
Thompson HJ (2009) A critical analysis of measures of caregiver and family functioning following traumatic brain injury. J Neurosci Nurs 41:148–158
Visser-Meily A, Post M, Schepers V, Lindeman E (2005) Spouses’ quality of life 1 year after stroke: prediction at the start of clinical rehabilitation. Cerebrovasc Dis 20:443–448
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Yehuda R (2002) Post-traumatic stress disorder. N Engl J Med 346:108–114
Zatzick DF, Jurkovich GJ, Gentilello L, Wisner D, Rivara FP (2002) Posttraumatic stress, problem drinking, and functional outcomes after injury. Arch Surg 137:200–205
Zatzick D, Jurkovich G, Rivara FP, Russo J, Wagner A, Wang J, Dunn C, Lord SP, Petrie M, O’Connor SS, Katon W (2013) A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg 257:390–399
Zirke N, Schmid G, Mazurek B, Klapp BF, Rauchfuss M (2007) Antonovsky’s Sense of Coherence in psychosomatic patients—a contribution to construct validation. Psychosoc Med 4, Doc03
Conflict of interest
The author(s) declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
This paper reports the results of a single-center study investigating mental illness symptoms in close relatives of patients with severe brain injury. An extraordinarily high prevalence of mental illness symptoms in relatives of patients with critical acquired brain injury is reported, and the results of the study are in concordance with previous studies within the field of neurorehabilitation. In neurorehabilitation, it is well established that there is an association between the condition of the patient and the condition of the relative. This association changes over time as the patient regains function and the family starts adapting to the changed situation of life. Consequently, it is necessary to collect information about the status of the patient when investigating the mental condition of close relatives. At the very least, establishing the rehabilitation status of the patient at follow-up is essential. The possible outcomes after severe brain injury are diverse, ranging from death to regaining physical and cognitive functioning, consequently affecting the mental condition of the relatives. Relatives of patients within rehabilitation facilities can experience hope and optimism regarding the future, whereas relatives of patients in nursing homes might experience despair, hopelessness, and symptoms of depression, etc. The only patient-related variable the authors used was the gross outcome measure Glasgow Outcome Scale (GOS), and they were not able to find any association between the patient’s GOS at time of the interview and the mental condition of the relative. However, this is not surprising, as the GOS is a gross distinction between broad categories ranging from dead to good recovery, and even patients categories with a ‘good recovery’ can have disabilities severely affecting the daily life of the family.
Patients scoring in the higher GOS categories will very often have more subtle and invisible deficits, however such may very well be more draining for the close relative than a hemiparesis, despite the fact that a hemiparesis can cause a lower GOS score because the patient may be depending on support. The lack of information about the status of the patient along with the varying follow-up interval limits the generalizability of the study. Nevertheless, the study does contribute to the existing literature in the field and emphasizes the vulnerability of the close relatives of patients with severe brain injury. Thus the study underlines the need for prospective studies testing efficiency of early psychotherapeutic interventions are needed, which the authors rightly state.
Anne Norup, Jannick Brennum
Copenhagen, Denmark
Rights and permissions
About this article
Cite this article
Rueckriegel, S.M., Baron, M., Domschke, K. et al. Trauma- and distress-associated mental illness symptoms in close relatives of patients with severe traumatic brain injury and high-grade subarachnoid hemorrhage. Acta Neurochir 157, 1329–1336 (2015). https://doi.org/10.1007/s00701-015-2470-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2470-0