Abstract
Purpose
The aim of this study was to investigate the influence of a history of diabetes mellitus (DM) and the glycated hemoglobin (HbA1c) level on the survival in patients who underwent complete resection for non-small cell lung cancer (NSCLC).
Methods
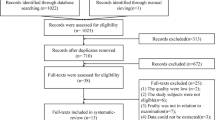
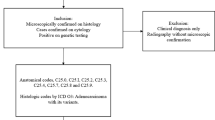
Of the patients who underwent complete resection for NSCLC between 2007 and 2015, 468 were classified into DM (who were currently taking medication for DM) and no DM groups as well as into high HbA1c (≥ 6.5) and normal HbA1c (< 6.5) groups.
Results
The overall survival (OS) did not differ significantly between either pair of groups. Among the elderly patients, the OS did not differ significantly between the DM and no DM groups, but was significantly higher in the normal-HbA1c group than in the high-HbA1c group (5-year survival rate: 84.7 versus 37.2%, respectively, p < 0.01). In the elderly patients, non-adenocarcinoma histology, advanced stage, a high Charlson comorbidity index, and a high preoperative HbA1c level were found to be independent risk factors for the OS.
Conclusion
We revealed that a high preoperative HbA1c level was associated with a poor OS in elderly patients who underwent complete resection for NSCLC. This suggests that it is necessary to achieve diabetic control prior to complete resection in NSCLC patients.


Similar content being viewed by others
References
Katanoda K, Hori M, Matsuda T, Shibata A, Nishino Y, Hattori M et al. An updated report on the trends in cancer incidence and mortality in Japan, 1958–2013. Jpn J Clin Oncol. 2015;45:390–401.
Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011;378:31–40.
Yuhara H, Steinmaus C, Cohen SE, Corley DA, Tei Y, Buffler PA. Is diabetes mellitus an independent risk factor for colon cancer and rectal cancer? Am J Gastroenterol. 2011;106:1911–21.
Liaw YP, Ko PC, Jan SR, Huang JY, Nfor ON, Lung CC, et al. Implications of type 1/2 diabetes mellitus in breast cancer development: a general female Population-based cohort study. J Cancer. 2015;6:734–9.
Lo SF, Chang SN, Muo CH, Chen SY, Liao FY, Dee SW, et al. Modest increase in risk of specific types of cancer types in type 2 diabetes mellitus patients. Int J Cancer. 2013;132:182–8.
Lee JY, Jeon I, Lee JM, Yoon JM, Park SM. Diabetes mellitus as an independent risk factor for lung cancer: a meta-analysis of observational studies. Eur J Cancer. 2013;49:2411–23.
Barone BB, Yeh HC, Snyder CF, Peairs KS, Stein KB, Derr RL,et al. Postoperative mortality in cancer patients with preexisting diabetes: systematic review and meta-analysis. Diabetes Care. 2010;33:931–9.
Jeong SS, Choi PJ, Yi JH, Yoon SS. Impact of lifestyle diseases on postoperative complications and survival in elderly patients with stage I non-small cell lung cancer. Korean J Thorac Cardiovasc Surg. 2017;50:86–93.
Hatlen P, Grønberg BH, Langhammer A, Carlsen SM, Amundsen T. Prolonged survival in patients with lung cancer with diabetes mellitus. J Thorac Oncol. 2011;6:1810–7.
Imai H, Kaira K, Mori K, Ono A, Akamatsu H, Matsumoto S, et al. Prognostic significance of diabetes mellitus in locally advanced non-small cell lung cancer. BMC Cancer. 2015;15:989. https://doi.org/10.1186/s12885-015-2012-4.
Kurishima K, Watanabe H, Ishikawa H, Satoh H, Hizawa N. Survival of patients with lung cancer and diabetes mellitus. Mol Clin Oncol. 2017;6:907–10.
Bartling B, Simm A, Sohst A, Silber RE, Hofmann HS. Effect of diabetes mellitus on the outcome of patients with resected non-small cell lung carcinoma. Gerontology. 2011;57:497–501.
Zhu L, Cao H, Zhang T, Shen H, Dong W, Wang L, et al. The effect of diabetes mellitus on lung cancer prognosis: a PRISMA-compliant meta-analysis of cohort studies. Medicine (Baltimore). 2016;95:e3528. https://doi.org/10.1097/MD.0000000000003528.
Dhillon SS, Groman A, Meagher A, Demmy T, Warren GW, Yendamuri S. Metformin and not diabetes influences the survival of resected early stage NSCLC patients. J Cancer Sci Ther. 2014;6:217–22.
International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009; 32: 1327–34.
World Health Organization. Histological typing of lung and pleural tumors. 3rd ed. Geneva: Springer; 1999.
Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM classification of malignant tumours. J Thorac Oncol. 2007; 2:706–14.
Luo J, Chen YJ, Chang LJ. Fasting blood glucose level and prognosis in non-small cell lung cancer (NSCLC) patients. Lung Cancer. 2012;76:242–7.
Rao Kondapally Seshasai S, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364:829–41.
Peters G, Gongoll S, Langner C, Mengel M, Piso P, Klempnauer J, et al. IGF-1R, IGF-1 and IGF-2 expression as potential prognostic and predictive markers in colorectal-cancer. Virchows Arch. 2003;443:139–45.
Ma J, Li H, Giovannucci E, Mucci L, Qiu W, Nguyen PL, et al. Prediagnostic body-mass index, plasma C-peptide concentration, and prostate cancer-specific mortality in men with prostate cancer: a long-term survival analysis. Lancet Oncol. 2008;9:1039–47.
AGryko M, Kiśluk J, Cepowicz D, Zińczuk J, Kamocki Z, Guzińska-Ustymowicz K, et al. Expression of insulin-like growth factor receptor type 1 correlate with lymphatic metastases in human gastric cancer. Pol J Pathol. 2014;65:135–40.
Zhang M, Li X, Zhang X, Yang Y, Feng Z, Liu X. Association of serum hemoglobin A1c, C-peptide and insulin-like growth factor-1 levels with the occurrence and development of lung cancer. Mol Clin Oncol. 2014;2:506–8.
Hsu CN, Chang CH, Lin YS, Lin JW, Caffrey JL. Association of serum C-peptide concentrations with cancer mortality risk in pre-diabetes or undiagnosed diabetes. PLoS One. 2013;8(2):e55625. https://doi.org/10.1371/journal.pone.0055625.
Kim JS, Kim ES, Liu D, Lee JJ, Solis L, Behrens C, et al. Prognostic impact of insulin receptor expression on survival of patients with nonsmall cell lung cancer. Cancer. 2012;118:2454–65.
Kim JS, Kim ES, Liu D, Lee JJ, Solis L, Behrens C, et al. Prognostic implications of tumoral expression of insulin like growth factors 1 and 2 in patients with non-small-cell lung cancer. Clin Lung Cancer. 2014;15:213–21.
Zhao S, Qiu Z, He J, Li L, Li W. Insulin-like growth factor receptor 1 (IGF1R) expression and survival in non-small cell lung cancer patients: a meta-analysis. Int J Clin Exp Pathol. 2014;7:6694–704.
Gately K, Forde L, Cuffe S, Cummins R, Kay EW, Feuerhake F, et al. High coexpression of both EGFR and IGF1R correlates with poor patient prognosis in resected non-small-cell lung cancer. Clin Lung Cancer. 2014;15:58–66.
Yeo CD, Park KH, Park CK, Lee SH, Kim SJ, Yoon HK, et al. Expression of insulin-like growth factor 1 receptor (IGF-1R) predicts poor responses to epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors in non-small cell lung cancer patients harboring activating EGFR mutations. Lung Cancer. 2015;87:311–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interests associated with this study.
Rights and permissions
About this article
Cite this article
Motoishi, M., Sawai, S., Hori, T. et al. The preoperative HbA1c level is an independent prognostic factor for the postoperative survival after resection of non-small cell lung cancer in elderly patients. Surg Today 48, 517–524 (2018). https://doi.org/10.1007/s00595-017-1612-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-017-1612-9