Abstract
Purpose
3D images offer true depth perception, which overcomes one of the disadvantages of laparoscopic surgery. We evaluated differences in the use of 3D and 2D images in laparoscopic surgery based on the recording of traces of forceps.
Methods
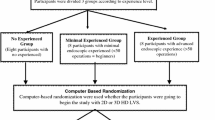
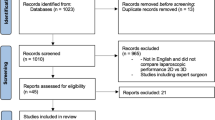
Twelve surgeons at our hospital participated in the study. The task consisted of one suture and three ligations, using a training box. The completion time and number of hold errors were noted, and forceps traces were recorded using the Behavior Checker system (Miura Medical). Participants were divided into two groups based on faster and slower completion times with 2D images.
Results
The median completion time in seconds (s) was significantly shorter when using 3D images than when using 2D images (51 s, range 34–146 vs. 63 s, range 38–265 s; p = 0.013). The 3D/2D completion time ratio was significantly higher in the faster 2D group (0.93 vs. 0.69, p = 0.030) indicating a greater effect of the 3D images on less experienced participants.
Conclusions
A quantitative evaluation showed that using 3D images enables more efficient use of laparoscopic forceps than 2D images. A system with 3D images is of particular benefit for inexperienced surgeons.




Similar content being viewed by others
References
Trastulli S, Cirocchi R, Listorti C, Cavaliere D, Avenia N, Gulla N, et al. Laparoscopic vs. open resection for rectal cancer: a meta-analysis of randomized clinical trials. Colorectal Dis. 2012;14:277–96.
Hasegawa S, Nagayama S, Nomura A, Kawamura J, Sakai Y. Autonomic nerve-preserving total mesorectal excision in the laparoscopic era. Dis Colon Rectum. 2008;51:1279–82.
Sakai Y, Nomura A, Masumori K, Kawamura J, Nagayama S. Recent interpretation of Denonvilliers’ fascia and the lateral ligament of the rectum. Asian J Endosc Surg. 2009;2:8–12.
Ohtani H, Tamamori Y, Azuma T, Mori Y, Nishiguchi Y, Maeda K, et al. A meta-analysis of the short- and long-term results of randomized controlled trials that compared laparoscopy-assisted and conventional open surgery for rectal cancer. J Gastrointest Surg. 2011;15:1375–85.
Hasegawa S, Hida K, Kawada K, Sakai Y. Laparoscopic surgery for rectal cancer (in Japanese with English abstract). J Jpn Soc Coloproctol. 2013;66:971–98.
Mizushima T, Nakajima K, Takeyama H, Naito A, Osawa H, Uemura M, et al. Single-incision laparoscopic surgery for stricturing and penetrating Crohn’s disease. Surg Today. 2016;46:203–8.
Ikeda A, Fukunaga Y, Akiyoshi T, Konishi T, Fujimoto Y, Nagayama S, et al. Laparoscopic right colectomy in patients treated with previous gastrectomy. Surg Today. 2016;46:209–13.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Katsuno H, Maeda K, Hanai T, Sato H, Masumori K, Koide Y, et al. Current status and future perspectives of robotic surgery for colorectal cancer (in Japanese with English abstract). J Jpn Soc Coloproctol. 2013;66:982–90.
Hanai T, Maeda K, Katsuno H, Masumori K. Robotic surgery for colorectal cancer in Japan (in Japanese with English abstract). J JSCAS. 2014;16:51–5.
LaGrange CA, Clark CU, Gerber EW, Strup SE. Evaluation of three different laparoscopic modalities: robotics versus three-dimensional vision laparoscopy versus standard laparoscopy. J Endourol. 2008;22:511–6.
Alaraimi B, El Bakbak W, Sarker S, Makkiyah S, Al-Marzouq A, Goriparthi R, et al. A randomized prospective study comparing acquisition of laparoscopic skills in three-dimensional (3D) vs. two-dimensional (2D) laparoscopy. World J Surg. 2014;38:2746–52.
Wilhelm D, Reiser S, Kohn N, Witte M, Leiner U, Muhlbach L, et al. Comparative evaluation of HD 2D/3D laparoscopic monitors and benchmarking to a theoretically ideal 3D pseudodisplay: even well-experienced laparoscopists perform better with 3D. Surg Endosc. 2014;28:2387–97.
Cicione A, Autorino R, Breda A, De Sio M, Damiano R, Fusco F, et al. Three-dimensional vs standard laparoscopy: comparative assessment using a validated program for laparoscopic urologic skills. Urology. 2013;82:1444–50.
Tanagho YS, Andriole GL, Paradis AG, Madison KM, Sandhu GS, Varela JE, et al. 2D versus 3D visualization: impact on laparoscopic proficiency using the fundamentals of laparoscopic surgery skill set. J Laparoendosc Adv Surg Tech A. 2012;22:865–70.
Uemura M, Yamashita M, Tomikawa M, Obata S, Souzaki R, Ieiri S, et al. Objective assessment of the suture ligature method for the laparoscopic intestinal anastomosis model using a new computerized system. Surg Endosc. 2015;29:444–52.
Harrysson IJ, Cook J, Sirimanna P, Feldman LS, Darzi A, Aqqarwal R. Systematic review of learning curves for minimally invasive abdominal surgery: a review of the methodology of data collection, depiction of outcomes, and statistical analysis. Ann Surg. 2014;260:37–45.
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg. 2004;91:146–50.
Boyle E, Kennedy AM, Traynor O, Hill AD. Training surgical skills using nonsurgical tasks: can Nintendo Wii™ improve surgical performance? J Surg Educ. 2011;68:148–54.
Acknowledgments
We thank Miura Medical for provision of the Behavior Checker and assistance with data analysis.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
Instrumentation supported by Miura Medical. Other funding from institutional sources only.
Conflict of interest
We have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Matsunaga, R., Nishizawa, Y., Saito, N. et al. Quantitative evaluation of 3D imaging in laparoscopic surgery. Surg Today 47, 440–444 (2017). https://doi.org/10.1007/s00595-016-1428-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-016-1428-z