Abstract
Purpose
To compare the pain and the duration of a panretinal photocoagulation (PRP) session using a conventional multispot laser (Quantel Medical) versus the Navilas® laser.
Methods
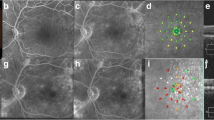
Treatment-naïve patients requiring bilateral PRP for diabetic retinopathy were included. For each patient, PRP was carried out using a conventional multispot laser (Quantel Medical, 577 nm) in one eye and the other eye was treated with the Navilas laser (OD-OS, 577 nm). For both PRP treatments, similar parameters (same power, exposure time, number, size and spacing of the spots) were used. For each eye, the duration of the session and the pain, measured using respectively a chronometer and a visual analogic scale (VAS), were recorded.
Results
Thirty-two eyes of sixteen patients (mean age 57 ± 13 SD, range 28–74), 11 men and 5 women, have been included. A mean of 1289 (1000–1500) spots with a mean power of 352 mW (300–450 mW) and an exposure time of 27 ms (20–30 ms) were delivered. The PRP session with the Navilas laser (mean time of 5.2 ± 0.8 min) was faster than with the conventional multispot laser (6.6 ± 1.1 min) (p = 0.02). Laser-induced pain was significantly reduced (VAS of 2.4 ± 1.6) using the Navilas laser compared to conventional laser (VAS: 7.1 ± 2) (p < 0.001).
Conclusion
The PRP sessions using the Navilas laser were significantly faster and less painful than with a conventional multispot laser in our series.




Similar content being viewed by others
References
Zheng Y, He M, Congdon N (2012) The worldwide epidemic of diabetic retinopathy. Indian J Ophthalmol 60(5):428–431
Writing Committee for the Diabetic Retinopathy Clinical Research Network, Gross JG, Glassman AR et al (2015) Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA 314:2137–2146
Beaulieu WT, Bressler NM, Melia M et al (2016) Panretinal photocoagulation versus ranibizumab for proliferative diabetic retinopathy: patient-centered outcomes from a randomized clinical trial. Am J Ophthalmol 170:206–213
Gross JG, Glassman AR, Liu D et al (2018) Five-year outcomes of panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol 136(10):1138–1148
Sivaprasad S, Prevost AT, Vasconcelos JC et al (2017) Clinical efficacy of intravitreal aflibercept versus panretinal photocoagulation for best corrected visual acuity in patients with proliferative diabetic retinopathy at 52 weeks (CLARITY): a multicentre, single-blinded, randomised, controlled, phase 2b, non-inferiority trial. Lancet 389(10085):2193–2203
American Academy of Ophthalmology Retina/Vitreous Panel (2016) Preferred practice pattern® guidelines. Diabetic retinopathy. American Academy of Ophthalmology, San Francisco, CA
Figueira J, Fletcher E, Massin P et al (2018) Ranibizumab plus panretinal photocoagulation versus panretinal photocoagulation alone for high-risk proliferative diabetic retinopathy (PROTEUS study). Ophthalmology 125(5):691–700
Early Treatment Diabetic Retinopathy Study Research Group (1985) Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol 103:1796–1806
Jain A, Blumenkranz MS, Paulus Y et al (2008) Effect of pulse duration on size and character of the lesion in retinal photocoagulation. Arch Ophthalmol 126(1):78–85
Nagpal M, Marlecha S, Nagpal K (2010) Comparison of laser photocoagulation for diabetic retinopathy using 532-nm standard laser versus multispot pattern scan laser. RETINA 30(3):452–458
Higaki M, Nozaki M, Yoshida M, Ogura Y (2018) Less expansion of short-pulse laser scars in panretinal photocoagulation for diabetic retinopathy. J Ophthal 2018:9371895
Muqit MM, Gray JC, Marcellino GR et al (2010) In vivo laser-tissue interactions and healing responses from 20- vs 100-millisecond pulse pascal photocoagulation burns. Arch Ophthalmol 128(4):448–455
Muqit MM, Marcellino GR, Gray GC et al (2010) Pain responses of Pascal 20 ms multi-spot and 100 ms single-spot panretinal photocoagulation: Manchester Pascal Study, MAPASS report 2. Br J Ophthal 94(11):1493–1498
Muqit MM, Marcellino GR, Henson DB et al (2011) Pascal panretinal laser ablation and regression analysis in proliferative diabetic retinopathy: Manchester Pascal Study Report 4. Eye 25(11):1447–1456
Kernt M, Cheuteu R, Vounotrypidis E et al (2011) Focal and panretinal photocoagulation with a navigated laser (NAVILAS®). Acta Ophthalmol 89(8):e662–e664
Kernt M, Cheuteu RE, Cserhati S et al (2012) Pain and accuracy of focal laser treatment for diabetic macular edema using a retinal navigated laser (Navilas). Clin Ophthalmol 6:289–296
Kim MS, Lee SW, Kim JS (2014) Comparison of the time required for panretinal photocoagulation and associated pain between Navilas® and conventional laser therapy in diabetic retinopathy. J Kor Ophthalmol Soc 55(8):1150
Chhablani J, Mathai A, Rani P et al (2014) Comparison of conventional pattern and novel navigated panretinal photocoagulation in proliferative diabetic retinopathy. Investig Opthalmol Vis Sci 55(6):3432–3438
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Eye Complications of Diabetes managed by Giuseppe Querques.
Rights and permissions
About this article
Cite this article
Amoroso, F., Pedinielli, A., Astroz, P. et al. Comparison of pain experience and time required for pre-planned navigated peripheral laser versus conventional multispot laser in the treatment of diabetic retinopathy. Acta Diabetol 57, 535–541 (2020). https://doi.org/10.1007/s00592-019-01455-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01455-x