Abstract
Aims
To analyze the visual outcome after early switch to dexamethasone (DEX) in eyes with diabetic macular edema previously treated with ranibizumab (RNB), based on structural spectral-domain optical coherence tomography (SD-OCT) features.
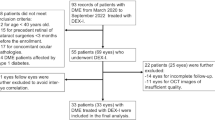
Methods
Retrospective study of data from 28 eyes which underwent a loading dose of three monthly RNB injections and were then shifted to DEX implant injection. SD-OCT analysis was performed before switch to DEX (week 12, 12W) according to the presence of integrity of ellipsoid zone (EZ) and external limiting membrane (ELM), disorganization of retinal inner layers (DRIL), and quantity of hyper-reflective spots (HRS). Best-corrected visual acuity (BCVA) changes at different time points after DEX (month 1, 1M; 4 months, 4M; and 12 months, 12M) were compared among groups.
Results
Significantly better BCVA was achieved at 1M in eyes with intact EZ (84.2 ± 12.3 letters; p = 0.04), with intact ELM (83.2 ± 11.5 letters; p < 0.01), and with fewer HRS (84.6 ± 12.5 letters; p = 0.03). However, the greatest percentage visual increase was achieved in eyes with disrupted EZ (+ 11.4%; p < 0.01), with disrupted ELM (+ 17.2%; p < 0.01), without DRIL (+ 12.5%; p < 0.01), and with more HRS (+ 14.3%; p = 0.04). After 12 months, a significant BCVA gain was observed only in eyes with intact retinal inner layers (+ 14.2%; p = 0.03).
Conclusions
Greater percentage BCVA improvement at 1M after switch to DEX was associated with EZ disruption, ELM disruption, intact retinal inner layers, and higher quantity of HRS. A switch to DEX therapy would be useful in patients with these SD-OCT features.

Similar content being viewed by others
References
The Eye Diseases Prevalence Research Group (2004) The prevalence of diabetic retinopathy among adults in the United States. Arch Ophthalmol 122(4):552–563
Bandello F, Cicinelli MV, Battaglia Parodi M (2015) Intravitreal ranibizumab for diabetic macular edema. Eur Ophthalmic Rev 9:25–31
Iacono P, Battaglia Parodi M, Bandello F (2010) Anti-vascular endothelial growth factor in diabetic retinopathy. Dev Ophthalmol 46:39–53
Bandello F, Berchicci L, La Spina C, Battaglia Parodi M, Iacono P (2012) Evidence for anti-VEGF treatment of diabetic macular edema. Ophthalmic Res 48:16–20
Shah SU, Maturi RK (2017) Therapeutic options in refractory diabetic macular oedema. Drugs 77:481–492
Nurözler Tabakcı B, Ünlü N (2017) Corticosteroid treatment in diabetic macular edema. Turk J Ophthalmol 47:156–160
Vujosevic S, Torresin T, Bini S et al (2016) Imaging retinal inflammatory biomarkers after intravitreal steroid and anti-VEGF treatment in diabetic macular oedema. Acta Ophthalmol 95:464–471
Bandello F, Cunha-Vaz J, Chong NV et al (2012) New approaches for the treatment of diabetic macular oedema: recommendations by an expert panel. Eye 26:485–493
Bandello F, Battaglia Parodi M, Tremolada G, Lattanzio R, De Benedetto U, Iacono P (2010) Steroids as part of combination treatment: the future for the management of macular edema? Ophthalmologica 224(1):41–45
Cicinelli MV, Cavalleri M, Querques L, Rabiolo A, Bandello F, Querques G (2017) Early response to ranibizumab predictive of functional outcome after dexamethasone for unresponsive diabetic macular oedema. Br J Ophthalmol 101:1689–1693
Fickweiler W, Schauwvlieghe AM, Schlingemann RO et al (2017) Predictive value of optical coherence tomographic features in the bevacizumab and ranibizumab in patients with diabetic macular edema (BRDME) study. Retina 38:812–819
Midena E, Bini S (2016) Multimodal retinal imaging of diabetic macular edema: toward new paradigms of pathophysiology. Graefes Arch Clin Exp Ophthalmol 254:1661–1668
Gonzalez VH, Campbell J, Holekamp NM et al (2016) Early and long-term responses to anti-vascular endothelial growth factor therapy in diabetic macular edema: analysis of protocol I data. Am J Ophthalmol 177:230–231
The Diabetic Retinopathy Clinical Research Network (2015) Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med 372(13):1193–1203
Maggio E, Sartore M, Attanasio M et al (2018) Anti-VEGF treatment for diabetic macular edema in a real-world clinical setting. Am J Ophthalmol 195:209–222
The Diabetic Retinopathy Clinical Research Network (2007) Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology 114:525–536
Maheshwary AS, Oster SF, Yuson RM, Cheng L, Mojana F, Freeman WR (2010) The association between percent disruption of the photoreceptor inner segment-outer segment junction and visual acuity in diabetic macular edema. Am J Ophthalmol 150:63–67
Santos AR, Costa M, Schwartz C et al (2018) Optical coherence tomography baseline predictors for initial best-corrected visual acuity response to intravitreal anti-vascular endothelial growth factor treatment in eyes with diabetic macular edema: the CHARTRES study. Retina 38:1110–1119
Zur D, Iglicki M, Busch C et al (2018) OCT biomarkers as functional outcome predictors in diabetic macular edema treated with dexamethasone implant. Ophthalmology 125:267–275
Seo KH, Yu SY, Kim M, Kwak HW (2016) Visual and morphologic outcomes of intravitreal ranibizumab for diabetic macular edema based on optical coherence tomography patterns. Retina 36(3):588–595
Sonoda S, Sakamoto T, Yamashita T, Shirasawa M, Otsuka H, Sonoda Y (2014) Retinal morphologic changes and concentrations of cytokines in eyes with diabetic macular edema. Retina 34(4):741–748
Sun JK, Lin MM, Lammer J et al (2014) Disorganization of the retinal inner layers as a predictor of visual acuity in eyes with center-involved diabetic macular edema. JAMA Ophthalmol 132:1309–1316
Vujosevic S, Bini S, Torresin T et al (2017) Hyperreflective retinal spots in normal and diabetic eyes: B-scan and en face spectral domain optical coherence tomography evaluation. Retina 37:1092–1103
Madeira MH, Boia R, Santos PF, Ambrósio AF, Santiago AR (2015) Contribution of microglia-mediated neuroinflammation to retinal degenerative diseases. Mediat Inflamm 2015:673090
Chatziralli I, Theodossiadis P, Parikakis E et al (2017) Dexamethasone intravitreal implant in diabetic macular edema: real-life data from a prospective study and predictive factors for visual outcome. Diabetes Ther 8:1393–1404
Hwang HS, Chae JB, Kim JY, Kim DY (2017) Association between hyperreflective dots on spectral-domain optical coherence tomography in macular edema and response to treatment. Investig Ophthalmol Vis Sci 58:5958–5967
Pilotto E, Bini S, Midena E (2018) Is diabetic retinopathy an inflammatory disease? Minerva Oftalmol 60:26–35
Funding
The contribution by IRCCS Fondazione Bietti in this paper was financially supported by Italian Ministry of Health and Fondazione Roma. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the conception or design of the work, the acquisition, analysis and interpretation of data, drafting the work, revising it critically for important intellectual content and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Michele Cavalleri, Maria Vittoria Cicinelli, Riccardo Sacconi, Daniele De Geronimo: none. Francesco Bandello consultant for: Alcon (Fort Worth,Texas,USA), Alimera Sciences (Alpharetta, Georgia, USA), Allergan Inc (Irvine, California,USA), Farmila-Thea (Clermont-Ferrand, France), Bayer Shering-Pharma (Berlin, Germany), Bausch And Lomb (Rochester, New York, USA), Genentech (San Francisco, California, USA), Hoffmann-La-Roche (Basel, Switzerland), NovagaliPharma (Évry, France), Novartis (Basel, Switzerland), Sanofi-Aventis (Paris, France), Thrombogenics (Heverlee,Belgium), Zeiss (Dublin, USA). Giuseppe Querques consultant for: Alimera Sciences (Alpharetta, Georgia, USA), Allergan Inc (Irvine, California,USA), Heidelberg (Germany), Novartis (Basel, Switzerland), Bayer Shering-Pharma (Berlin, Germany), Zeiss (Dublin, USA). Mariacristina Parravano consultant for: Allergan Inc (Irvine, California, USA), Bayer Shering-Pharma (Berlin, Germany), Novartis (Basel, Switzerland). Monica Varano consultant for: Allergan Inc (Irvine, California, USA), Bayer Shering-Pharma (Berlin, Germany), Novartis (Basel, Switzerland).
Ethical approval
This study was conducted in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Managed by Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cavalleri, M., Cicinelli, M.V., Parravano, M. et al. Prognostic role of optical coherence tomography after switch to dexamethasone in diabetic macular edema. Acta Diabetol 57, 163–171 (2020). https://doi.org/10.1007/s00592-019-01389-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01389-4